Published online Jun 6, 2020. doi: 10.12998/wjcc.v8.i11.2312
Peer-review started: February 5, 2020
First decision: March 24, 2020
Revised: March 24, 2020
Accepted: April 22, 2020
Article in press: April 22, 2020
Published online: June 6, 2020
Processing time: 123 Days and 19.7 Hours
Thin-walled lung cancer manifests as a cystic lesion, mostly adenocarcinoma. It is often misdiagnosed as a benign lesion in clinical practice, thus delaying the diagnosis and surgical treatment. Its natural course is rarely recorded and observed; thus, the pathogenesis and diagnosis need to be clarified and improved.
A 66-year-old man developed a mass in the upper lobe of the right lung and a small, thin-walled cavity in the lower lobe of the right lung in 2007. The right upper lobe mass was confirmed to be adenocarcinoma after surgery. The cavity diameter increased from 11 mm to 31 mm over 10 years, and a ground glass opacity lesion appeared around the bulla on computed tomography. A second operation confirmed that the lesion was lepidic predominant adenocarcinoma. Here we report a rare case of lung cancer developing from a focal bulla to a thin-walled adenocarcinoma for more than 10 years and confirm that the check-valve mechanism explains the pathogenesis.
Solitary thin-walled lung adenocarcinoma is a rare tumor in terms of its clinical manifestations, pathogenesis, and disease progression. The check-valve mechanism can explain the cause of thin-walled lung cancer. Close follow-up and accurate imaging are necessary.
Core tip: We describe a rare case of lung adenocarcinoma with gradual enlargement of a thin-walled cavity surrounded by pure ground glass opacity on on computed tomography for more than 10 years. The natural course of the patient's thin-walled lung adenocarcinoma was observed and the check-valve mechanism can explain the cause of thin-walled lung cancer. To avoid misdiagnosis of such diseases close follow-up and accurate imaging are necessary.
- Citation: Meng SS, Wang SD, Zhang YY, Wang J. Lung cancer from a focal bulla into thin-walled adenocarcinoma with ground glass opacity — an observation for more than 10 years: A case report. World J Clin Cases 2020; 8(11): 2312-2317
- URL: https://www.wjgnet.com/2307-8960/full/v8/i11/2312.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i11.2312
Lung cancer has one of the highest mortality rates worldwide. Low-dose computed tomography (CT) has become an important method for screening and monitoring recurrence in lung cancer[1]. The manifestations of lung cancer on CT imaging are diverse. Solitary thin-walled lung adenocarcinoma is a special form of lung cancer, which is rare in clinical practice[2]. Its pathogenesis is inconclusive and diagnosis is very challenging. It is often misdiagnosed as a benign lesion such as a pulmonary cyst or tuberculous cavity, thus delaying diagnosis and surgical treatment[3]. We describe a rare case of lung adenocarcinoma with gradual enlargement of a thin-walled cavity surrounded by pure ground glass opacity (GGO) on CT for more than 10 years.
A 66-year-old male patient presented with a thin-walled cavity surrounded by a GGO in the right lung on CT in November 2017. The patient had no obvious discomfort.
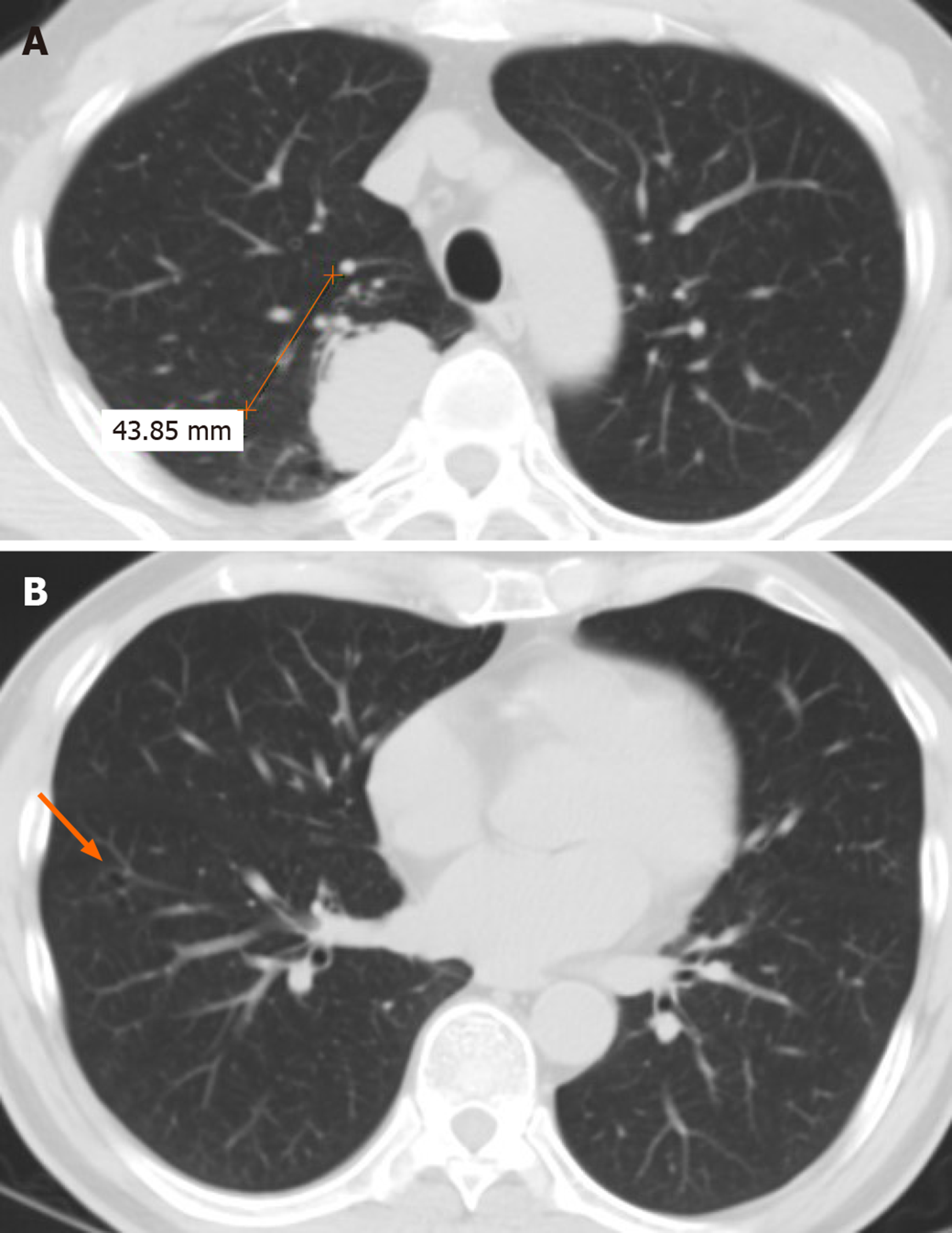
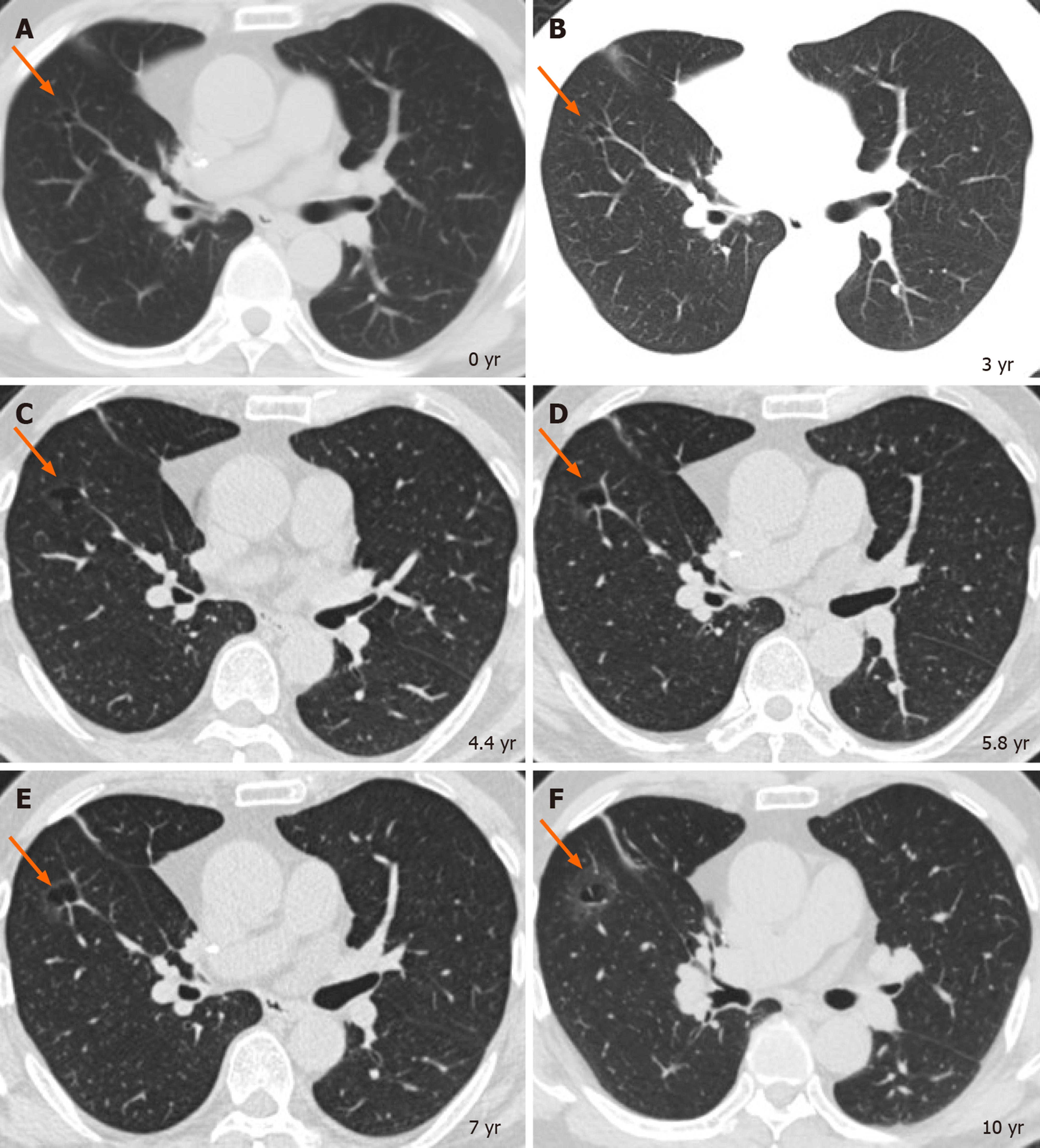
A previous chest CT in 2007 showed a 4.3 cm × 2.5 cm mass in the right upper lobe and a small thin-walled cavity in the right anterior basal segment (Figure 1). The patient underwent video-assisted thoracoscopic lobectomy for primary lung adenocarcinoma in the right upper lobe in August 2007, and pathology demonstrated a well differentiated adenocarcinoma of stage T2bN0M0 (stage 2A). The small thin-walled cavity was considered benign and was not treated. During his regular follow-up, no obvious change was observed in 2008, while the cavity gradually enlarged from 11 mm to 14 mm in diameter and no recurrence was observed on the chest CT from 2008 to 2014. During the next two years, the patient did not undergo any examinations and paid no attention to the cavity. In August 2017, his chest CT scan showed that the size of the lesion had increased to 31 mm and had become a bulla surrounded by GGO (Figure 2).
The patient was in good health with no comorbidities, except for a history of lung cancer surgery in 2007 (adenocarcinoma in the right upper lobe, at T2bN0M0 stage 2A).
The patient had a 40 pack-year history of cigarette smoking and a history of contact with tuberculosis patients, including his mother and sister.
His vital signs were stable, and no obvious abnormalities were found on examination.
Related tumor markers were negative.
We traced the CT data of this patient for 10 years. As mentioned earlier, the small thin-walled cavity gradually transformed into GGO around the bulla. On the enhanced CT scanning, the degree of enhancement of the lesion was difficult to evaluate, and the structure inside the cavity was irregular. Imaging physicians and lung cancer surgeons believed that the lesion was highly malignant, based on its imaging characteristics and the process of evolution in recent years.
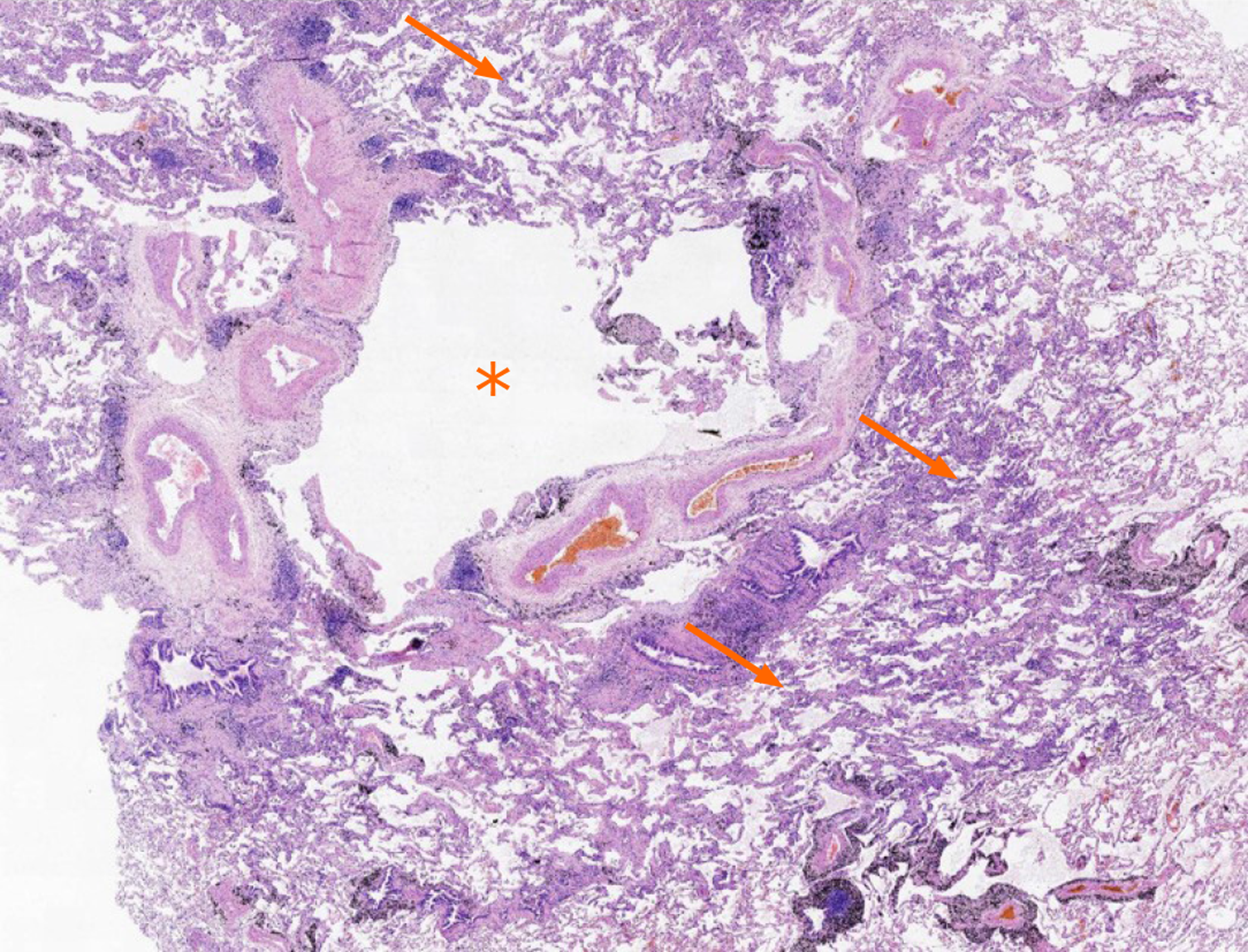
Final postoperative pathology diagnosis was lepidic predominant adenocarcinoma.
The patient underwent video-assisted thoracoscopic wedge resection of the right lower lobe on November 15, 2017. The surgical specimen showed a cavity with a malignant appearance in the surrounding tissue (Figure 3). The pathological result was lepidic predominant adenocarcinoma (Figure 4). No lymph node metastasis was observed and no further treatment was required after surgery.
The patient recovered well and was discharged one week after surgery. During the follow-up period of 24 mo, no recurrence was noted.
Lung cancer presenting as cystic lesions was first described by Anderson and Pierce in 1954[4]. A recent study suggested that the incidence of cystic lung cancer was 0.46% of surgical cases (15 of 3268)[5]. Histological analysis showed that most cases were adenocarcinoma. It is suggested that malignant imaging features often include asymmetric thickening of the wall, septum in the cavity, irregular margin, short spicules, and blood vessel convergence signs. Due to the thin walls, ordinary percutaneous needle biopsy and transbronchial biopsy rarely obtain sufficient diagnostic specimens. It is reported that the sensitivity of CT-guided percutaneous needle aspiration in these cases is 91%[5].
The pathogenesis of bullous lung cancer remains unclear. There are several hypotheses on the tumorigenesis: The check-valve mechanism; central necrosis and enzymatic digestion of solid lesions; lesions invading the original cyst structure, etc. It has been reported that the check-valve is formed as a result of bronchial wall collapse, which leads to the cavity, and as the internal pressure increases, the cavity gradually increases, and the irregular growth of the tumor tissue forms asymmetric thickening of the wall[6].
In the present case, the patient’s imaging data showed clearly the enlargement of the thin-walled lung adenocarcinoma. CT images 10 years previously did not provide sufficient evidence of malignancy. Without continuous observation over 10 years, this lesion may have been regarded as a tuberculous cavity or local inflammation. By analyzing the evolution of the lesion, an accurate diagnosis can be established and appropriate treatment provided. It can also enhance the surgeon’s awareness of this disease, and add experience of diagnosis and treatment. Observation and follow-up of suspicious lesions contribute to appropriate clinical decisions.
Previously reported cases of lung cancer presenting as thin-walled cysts had a maximum observation time of 6 mo[5]. Very few patients with multiple primary cancers have been reported. Lung adenocarcinoma with gradual enlargement of a thin-walled cavity surrounded by pure GGO for more than 10 years has never been reported before. We report the natural course of lung adenocarcinoma with a thin-walled cavity, which confirms the check-valve mechanism.
Solitary thin-walled lung adenocarcinoma is a rare tumor in terms of its clinical manifestations, pathogenesis, and disease progression. The check-valve mechanism explains the cause of thin-walled lung cancer. Due to the difficulty in diagnosing this disease, close follow-up and accurate imaging are required.
The authors appreciate the efforts of the surgeons, and doctors and nurses from pathology, radiology, and anesthesia departments in this case report.
| 1. | National Lung Screening Trial Research Team, Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8099] [Cited by in RCA: 8072] [Article Influence: 538.1] [Reference Citation Analysis (2)] |
| 2. | Lan CC, Wu HC, Lee CH, Huang SF, Wu YK. Lung cancer with unusual presentation as a thin-walled cyst in a young nonsmoker. J Thorac Oncol. 2010;5:1481-1482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Watanabe Y, Kusumoto M, Yoshida A, Shiraishi K, Suzuki K, Watanabe SI, Tsuta K. Cavity Wall Thickness in Solitary Cavitary Lung Adenocarcinomas Is a Prognostic Indicator. Ann Thorac Surg. 2016;102:1863-1871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Anderson HJ, PIERCE JW. Carcinoma of the bronchus presenting as thin-walled cysts. Thorax. 1954;9:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Guo J, Liang C, Sun Y, Zhou N, Liu Y, Chu X. Lung cancer presenting as thin-walled cysts: An analysis of 15 cases and review of literature. Asia Pac J Clin Oncol. 2016;12:e105-e112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Fintelmann FJ, Brinkmann JK, Jeck WR, Troschel FM, Digumarthy SR, Mino-Kenudson M, Shepard JO. Lung Cancers Associated With Cystic Airspaces: Natural History, Pathologic Correlation, and Mutational Analysis. J Thorac Imaging. 2017;32:176-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ebrahimifar M, Kung WM, Sugimura H S-Editor: Zhang L L-Editor: MedE-Ma JY E-Editor: Liu JH