Published online May 26, 2020. doi: 10.12998/wjcc.v8.i10.1950
Peer-review started: March 5, 2020
First decision: April 1, 2020
Revised: April 1, 2020
Accepted: April 28, 2020
Article in press: April 28, 2020
Published online: May 26, 2020
Processing time: 81 Days and 3.3 Hours
T4 esophageal cancer portends a poor prognosis, particularly when it is complicated by a tracheoesophageal fistula (TEF) either resulting from disease or occurring as a complication of treatment. Patients with TEF that occurs during treatment are commonly treated with palliative intent because fistula-associated treatment complications such as aspiration pneumonia and mediastinitis are associated with high morbidity and mortality. To date, there is no clear evidence on the optimal treatment of T4 esophageal cancer, particularly when a TEF formation occurs.
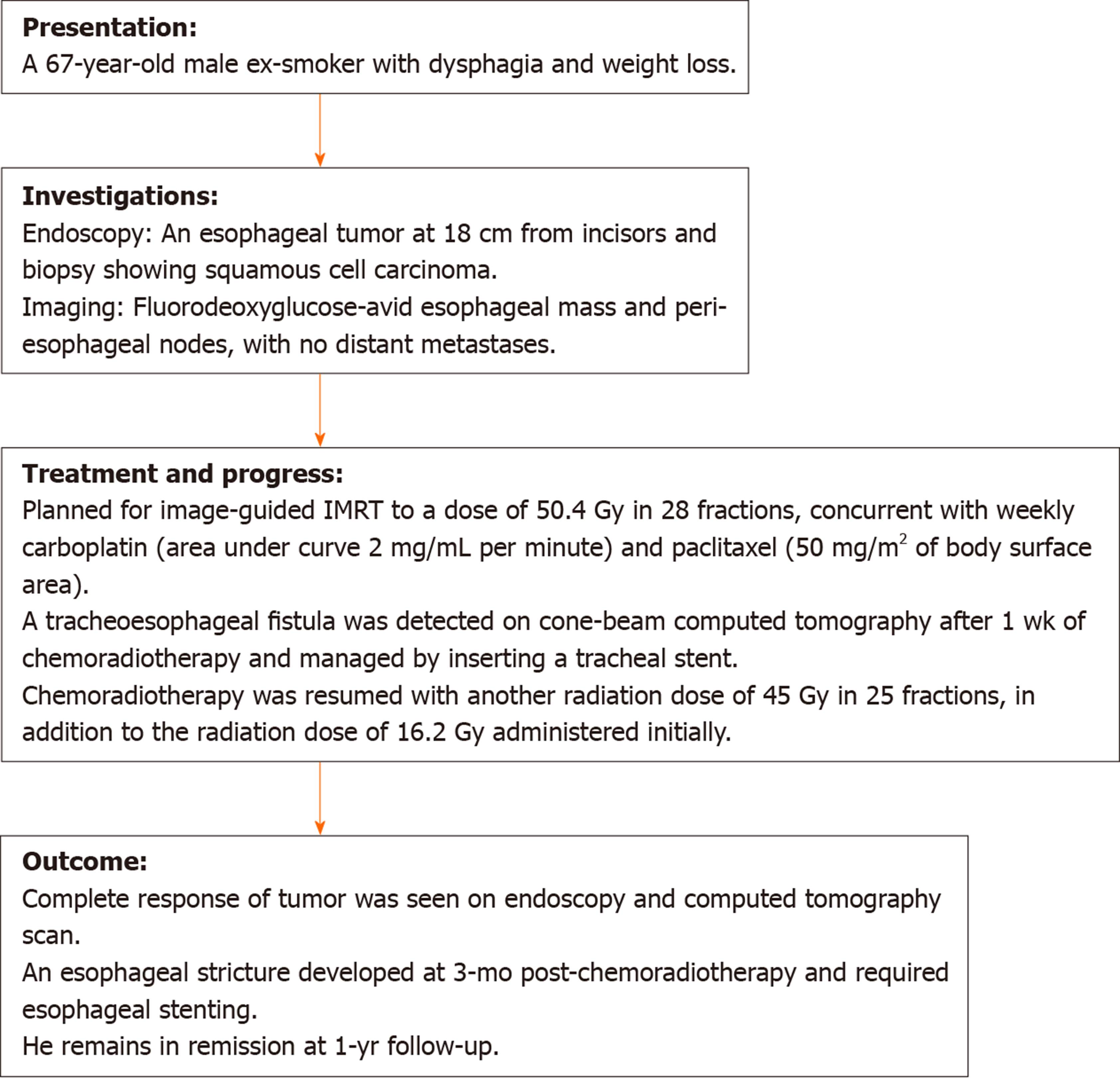
A 67-year-old gentleman who presented with dysphagia and weight loss. Endoscopy and imaging revealed a T4N1M0 cervical esophageal squamous cell carcinoma. He received image-guided intensity-modulated radiation therapy, with concurrent weekly carboplatin (area under curve 2 mg/mL per minute) and paclitaxel (50 mg/m2 of body surface area). One week after treatment initiation (16.2 Gy thus far), he developed cough on swallowing. A TEF was detected on image-guided radiation therapy using cone-beam computed tomography during the treatment course, for which a tracheal stent was inserted. After discussing the risks and morbidity of continuing treatment, he resumed chemoradiotherapy with an additional radiation dose of 45 Gy in 25 fractions. Three months after completion of chemoradiotherapy, he developed an esophageal stricture that required esophageal stenting and dilatation. The patient remains cancer-free at two year on follow-up. Complete response of esophageal cancer was evident on post-treatment endoscopy and computed tomography imaging, with successful closure of TEF.
This case highlights that successful curative treatment for esophageal cancer complicated by a TEF is possible using novel chemotherapeutic regimens and modern radiation technologies.
Core tip: A trachea-esophageal fistula (TEF) may occur as a complication of treatment for definitive chemoradiotherapy for T4 esophageal cancer, particularly when treating with effective novel agents such as carboplatin-paclitaxel which may induce excellent tumor shrinkage. Because of the high morbidity and mortality associated with TEF, treatment intent is commonly switched from curative to palliative. The successful treatment in this case suggests that patients who develop TEF during treatment should carry on completing the planned treatment after discussion of potential benefits and risks. Excellent treatment responses may be obtained and the TEF may resolve completely.
- Citation: Lee CC, Yeo CM, Ng WK, Verma A, Tey JC. T4 cervical esophageal cancer cured with modern chemoradiotherapy: A case report. World J Clin Cases 2020; 8(10): 1950-1957
- URL: https://www.wjgnet.com/2307-8960/full/v8/i10/1950.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i10.1950
Despite recent advances in multidisciplinary treatments, the outcomes of patients with esophageal cancer invading into adjacent structures remain unsatisfactory[1,2]. T4 disease portends a poor prognosis, particularly when it is complicated by a tracheoesophageal fistula (TEF) which can result from the disease or occur as a complication of treatment due to the resultant tumor necrosis and shrinkage[3]. The incidence of malignant fistulas developing during chemoradiotherapy in esophageal cancer is reported to be 5% to 22%[4,5]. Closure of malignant fistulas have been observed in 70% patients after treatment[3].
To date, there is no consensus on the optimal treatment approach for T4 esophageal cancer complicated by a TEF[1]. The two-common curative-intent treatment approaches are definitive chemoradiotherapy and neoadjuvant chemoradiotherapy followed by surgical resection. However, treating clinicians may opt to switch the treatment intent from curative to palliative when a TEF forms during treatment, because TEF-associated treatment complications such as aspiration pneumonia and mediastinitis are associated with high morbidity and mortality[6,7].
Herein, we present a case of unresectable T4 cervical esophageal squamous cell carcinoma (SCC) complicated by a TEF during treatment, who completed treatment successfully with modern image-guided intensity-modulated radiation therapy (IMRT) and concurrent carboplatin-paclitaxel.
A 67-year-old male ex-smoker was referred from primary care physician to Department of General Surgery of our hospital in March 2018 with worsening dysphagia.
Patient’s symptoms started 3 mo ago, associated with weight loss of 7 kg over past 2 mo.
He did not have any past medical or surgical illness, except appendicectomy.
His mother was diagnosed with cervix cancer.
His blood pressure was 103/67 mmHg and heart rate 91 beats per minutes. His oxygen saturation was 98% on room air. He had thin built with the body weight of 48 kg. There were no cervical or supraclavicular nodes palpable. Abdomen was soft and non-tender.
Hemoglobin level was 13.2 g/dL. Creatinine was 0.86 mg/dL with creatinine clearance of 57 mL/min using Cockcroft-Gault formula.
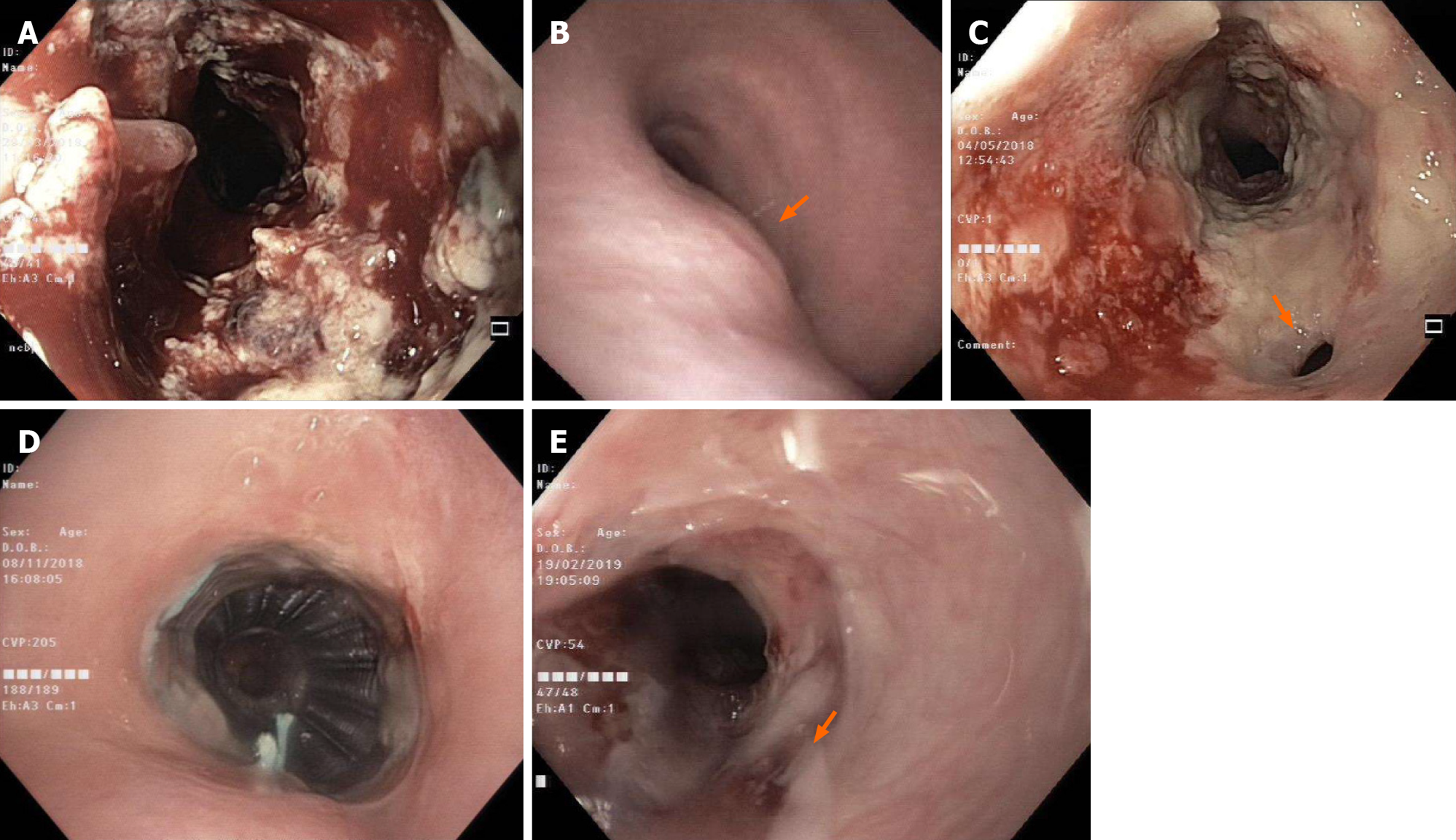
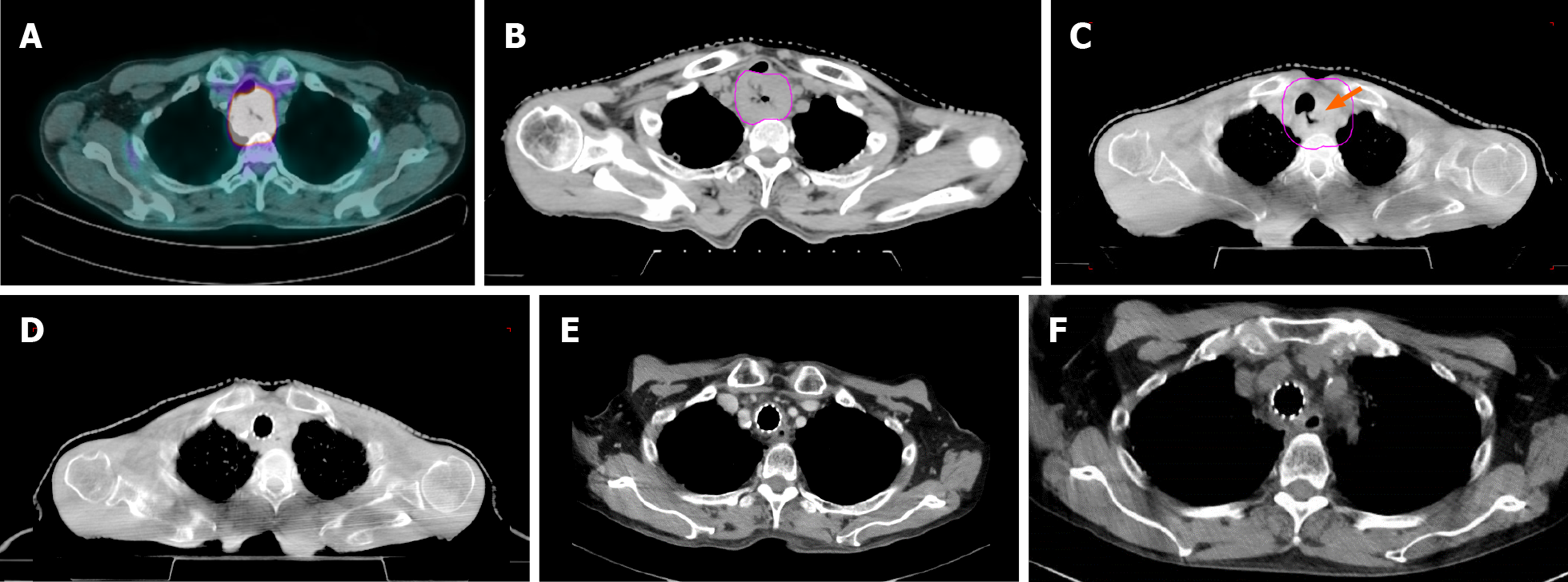
Esophagogastroduodenoscopy revealed an esophageal tumor with its proximal margin at 18 cm from incisors and biopsy showing SCC (Figure 1A). Positron emission tomography-computed tomography (PET-CT) reported an intensely fluorodeoxyglucose-avid esophageal mass and peri-esophageal nodes, without evidence of distant metastases (Figure 2A). Bronchoscopy showed a 4 mm-length extrinsic compression of the upper trachea with no invasion seen (Figure 1B).
The tumor was deemed unresectable as surgery may result in functional deficits and impairment of quality of life due to the tumor location.
Definitive concurrent chemoradiotherapy was recommended. The proposed chemotherapeutic regimen was weekly carboplatin (area under curve 2 mg/mL per minute) and paclitaxel (50 mg/m2 of body surface area) doublet combination.
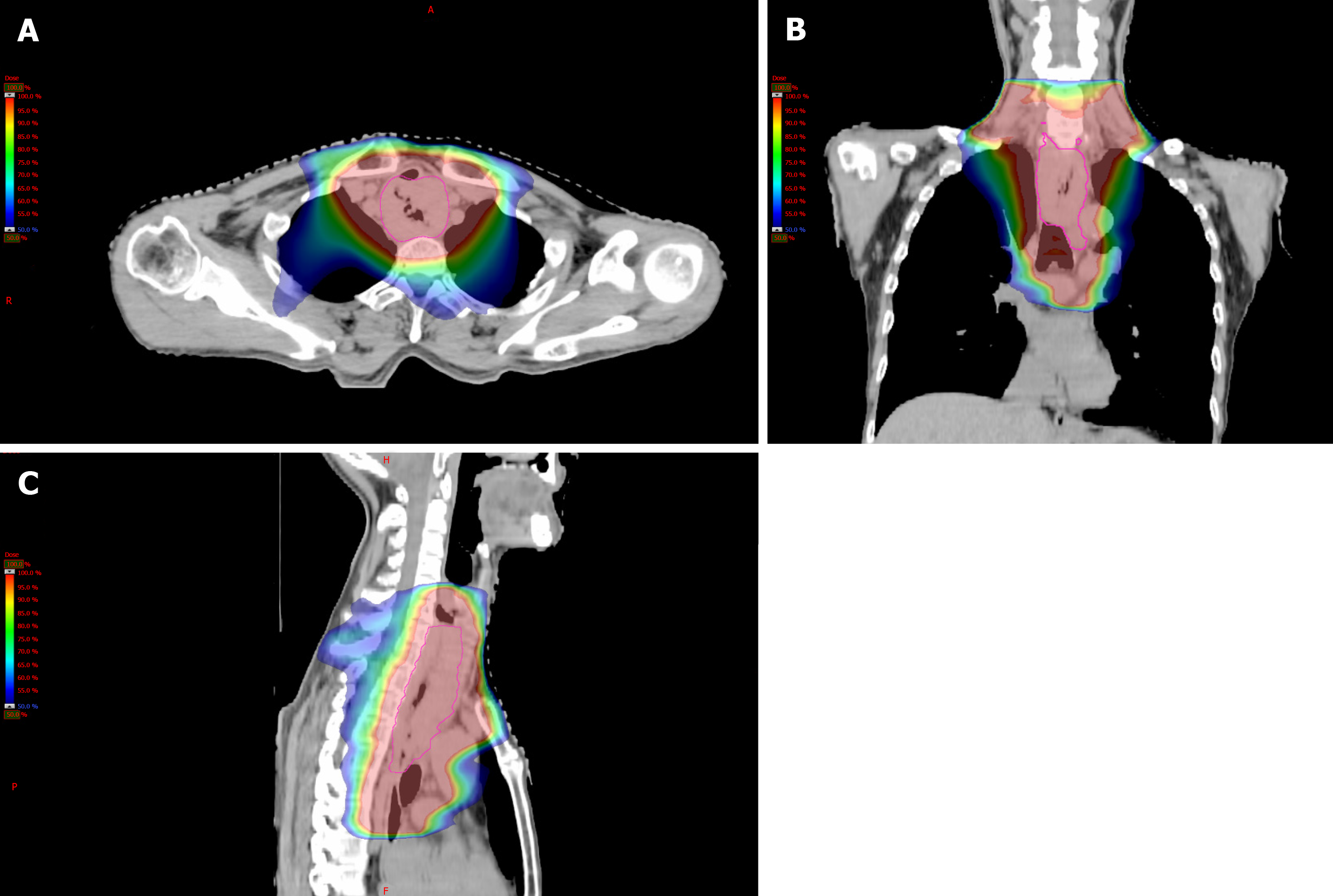
Definitive concurrent chemoradiotherapy was recommended. Image-guided IMRT to a total dose of 50.4 Gy in 28 fractions was offered.
The final diagnosis of the present case was unresectable T4N1M0 cervical esophageal SCC.
He was started on image-guided IMRT to a planned dose of 50.4 Gy in 28 fractions (Figures 2B and 3A-C), with concurrent weekly carboplatin (area under curve 2 mg/mL per minute) and paclitaxel (50 mg/m2 of body surface area). After 1 wk of treatment, he developed cough when swallowing. Cone-beam CT (Figure 2C) demonstrated a TEF confirmed with endoscopy (Figure 1C). Esophageal stenting was explored but deemed technically not feasible due to the close proximity to the upper esophageal sphincter, limiting the ability for safe esophageal stenting. Tracheal stent insertion was attempted twice. Ultimately a tracheal stent (Ultraflex 20 mm × 60 mm) was inserted and sited 4 cm below the vocal cords, covering the fistula on the third attempt.
After 6 wk of treatment break, the patient resumed chemoradiotherapy after tracheal stenting was performed successfully. Restaging PET/CT prior to chemoradiotherapy confirmed no evidence of new disease. A percutaneous radiologically inserted gastrostomy (PRG) tube was inserted for nutrition support during this interim period while waiting for esophageal fistula to improve with time following the treatment. Percutaneous endoscopic gastrostomy (PEG) was not preferred because the tube will go through the esophageal cancer during the procedure with a risk of seeding at PEG stoma. Instead, a PRG was done to mitigate this risk. In addition to the radiation dose of 16.2 Gy delivered initially, he received another 45 Gy in 25 fractions uneventfully (Figure 2D).
Three months after completion of chemoradiotherapy, he developed an esophageal stricture that required esophageal stenting and dilatation. Complete response of esophageal cancer and closure of TEF was seen on post-treatment endoscopy and CT (Figures 1D, E and 2E, F). The patient remains cancer-free at two year on follow-up. The timeline of the events is summarized in Figure 4.
We presented a case of successful treatment of unresectable T4N1M0 cervical esophageal SCC complicated by a TEF during chemoradiotherapy, after which clinical complete response was achieved with the closure of TEF after treatment with modern image-guided IMRT and concurrent carboplatin-paclitaxel as a novel chemotherapeutic regimen. Image guidance played an important role in this case as it permitted early detection of TEF and subsequent close monitoring of TEF-associated complications throughout the treatment course.
T4 esophageal cancer associated with fistula formation often presents a clinical therapeutic dilemma. Most clinicians tend to propose palliative rather than curative intent treatment. As a result of the absence of high-quality evidence, there is currently no consensus on the optimal treatment strategy of T4 esophageal cancer complicated by a fistula. Despite lacking randomized controlled trials, neoadjuvant chemoradiotherapy followed by surgery and definitive chemoradiotherapy are the two commonly practiced treatment approaches. Two prospective phase 2 studies supported the use of neoadjuvant chemoradiotherapy followed by surgery in patients with T4 esophageal cancer, with reported 1-year overall survival of 68% to 83%, and pathological complete response rate of 8% to 20% and R0 resection rate of 92% to 95%[7,8]. Whereas another two prospective trials and retrospective studies examining the efficacy of definitive chemoradiotherapy using 5-Fluorouracil (5FU)-cisplatin doublet in patients with T4 disease or unresectable regional nodal metastases reported 1-year OS ranging between 30% and 56%[5,6,9,10]. Recently, the introduction of 5FU-cisplatin-docetaxel triplet in phase 2 trials has shown further improvement in 1-year OS to 66%-78%[4,11].
Given the tumor location in the cervical esophagus in this case, it was deemed unresectable due to the potential functional deficits and impairment in quality of life. Hence definitive chemoradiotherapy approach was recommended. Instead of the conventional 5FU-cisplatin combination, weekly carboplatin (area under curve 2 mg/mL per minute) and paclitaxel (50 mg/m2 of body surface area) was chosen for this patient due to its comparably tolerable side-effect profile. The efficacy basis of this chemotherapy regimen was extrapolated from the landmark CROSS trial which reported a survival benefit for neoadjuvant chemoradiotherapy followed by definitive surgery with an impressive pathological complete response rate of 49% in the patients of SCC histology subtype in patients with locally-advanced cancer of esophagus or esophagogastric junction[12]. Of note, CROSS trial has excluded T4 tumors. In light of the excellent treatment response in this patient, weekly carboplatin and paclitaxel which has not been evaluated in the previous studies on T4 esophageal cancer should be considered as a potential novel chemotherapeutic regimen as part of definitive chemoradiotherapy treatment in this population.
The utilization of modern radiation techniques has a clear role in improving the therapeutic ratio in cancer treatment. For instance, the implementation of IMRT in the treatment of esophageal cancers has allowed for greater dose conformality to the target volumes and avoidance of organs at risk such as the spinal cord, lungs and heart. In addition, image guided radiation therapy has allowed for precise target localization during the delivery of radiation. For patients with radiosensitive histology like SCC treated with this potentially effective chemotherapy regimen where excellent tumor response is anticipated, image-guided radiation therapy should be considered as an important adjunct to monitor for any radiologically detectable complications, such as fistula formation.
Malignant TEF is an undesirable complication and usually require endoscopic interventions. Literature suggests that stenting both trachea and esophagus conferred superior outcomes including better quality of life and possibly survival benefit compared to stenting either trachea or esophagus alone[13-16]. However, the role of double stenting (concomitant esophageal and tracheal stents) remains questionable. The suitability of esophageal and/or tracheal stenting should be evaluated by experienced endoscopists.
In conclusion, a successful curative treatment of esophageal cancer complicated by a TEF necessitates a multidisciplinary approach with various supportive interventions. While the optimal treatment regimen is not well-established, definitive concurrent chemoradiotherapy using image-guided IMRT and novel carboplatin-paclitaxel is an effective treatment option.
| 1. | Makino T, Yamasaki M, Tanaka K, Miyazaki Y, Takahashi T, Kurokawa Y, Motoori M, Kimura Y, Nakajima K, Mori M, Doki Y. Treatment and clinical outcome of clinical T4 esophageal cancer: A systematic review. Ann Gastroenterol Surg. 2019;3:169-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 41] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Akutsu Y, Matsubara H. Chemoradiotherapy and surgery for T4 esophageal cancer in Japan. Surg Today. 2015;45:1360-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Muto M, Ohtsu A, Miyamoto S, Muro K, Boku N, Ishikura S, Satake M, Ogino T, Tajiri H, Yoshida S. Concurrent chemoradiotherapy for esophageal carcinoma patients with malignant fistulae. Cancer. 1999;86:1406-1413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Higuchi K, Komori S, Tanabe S, Katada C, Azuma M, Ishiyama H, Sasaki T, Ishido K, Katada N, Hayakawa K, Koizumi W; Kitasato Digestive Disease and Oncology Group. Definitive chemoradiation therapy with docetaxel, cisplatin, and 5-fluorouracil (DCF-R) in advanced esophageal cancer: a phase 2 trial (KDOG 0501-P2). Int J Radiat Oncol Biol Phys. 2014;89:872-879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 5. | Shinoda M, Ando N, Kato K, Ishikura S, Kato H, Tsubosa Y, Minashi K, Okabe H, Kimura Y, Kawano T, Kosugi S, Toh Y, Nakamura K, Fukuda H; Japan Clinical Oncology Group. Randomized study of low-dose versus standard-dose chemoradiotherapy for unresectable esophageal squamous cell carcinoma (JCOG0303). Cancer Sci. 2015;106:407-412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 132] [Article Influence: 12.0] [Reference Citation Analysis (1)] |
| 6. | Nishimura Y, Suzuki M, Nakamatsu K, Kanamori S, Yagyu Y, Shigeoka H. Prospective trial of concurrent chemoradiotherapy with protracted infusion of 5-fluorouracil and cisplatin for T4 esophageal cancer with or without fistula. Int J Radiat Oncol Biol Phys. 2002;53:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Yokota T, Kato K, Hamamoto Y, Tsubosa Y, Ogawa H, Ito Y, Hara H, Ura T, Kojima T, Chin K, Hironaka S, Kii T, Kojima Y, Akutsu Y, Matsushita H, Kawakami K, Mori K, Nagai Y, Asami C, Kitagawa Y. Phase II study of chemoselection with docetaxel plus cisplatin and 5-fluorouracil induction chemotherapy and subsequent conversion surgery for locally advanced unresectable oesophageal cancer. Br J Cancer. 2016;115:1328-1334. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 113] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 8. | Ikeda K, Ishida K, Sato N, Koeda K, Aoki K, Kimura Y, Iwaya T, Ogasawara S, Iijima S, Nakamura R, Uesugi N, Maesawa C, Saito K. Chemoradiotherapy followed by surgery for thoracic esophageal cancer potentially or actually involving adjacent organs. Dis Esophagus. 2001;14:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Ishida K, Ando N, Yamamoto S, Ide H, Shinoda M. Phase II study of cisplatin and 5-fluorouracil with concurrent radiotherapy in advanced squamous cell carcinoma of the esophagus: a Japan Esophageal Oncology Group (JEOG)/Japan Clinical Oncology Group trial (JCOG9516). Jpn J Clin Oncol. 2004;34:615-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 183] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 10. | Ohtsu A, Boku N, Muro K, Chin K, Muto M, Yoshida S, Satake M, Ishikura S, Ogino T, Miyata Y, Seki S, Kaneko K, Nakamura A. Definitive chemoradiotherapy for T4 and/or M1 lymph node squamous cell carcinoma of the esophagus. J Clin Oncol. 1999;17:2915-2921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 326] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 11. | Miyazaki T, Sohda M, Tanaka N, Suzuki S, Ieta K, Sakai M, Sano A, Yokobori T, Inose T, Nakajima M, Fukuchi M, Ojima H, Kato H, Kuwano H. Phase I/II study of docetaxel, cisplatin, and 5-fluorouracil combination chemoradiotherapy in patients with advanced esophageal cancer. Cancer Chemother Pharmacol. 2015;75:449-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Shapiro J, van Lanschot JJB, Hulshof MCCM, van Hagen P, van Berge Henegouwen MI, Wijnhoven BPL, van Laarhoven HWM, Nieuwenhuijzen GAP, Hospers GAP, Bonenkamp JJ, Cuesta MA, Blaisse RJB, Busch ORC, Ten Kate FJW, Creemers GM, Punt CJA, Plukker JTM, Verheul HMW, Bilgen EJS, van Dekken H, van der Sangen MJC, Rozema T, Biermann K, Beukema JC, Piet AHM, van Rij CM, Reinders JG, Tilanus HW, Steyerberg EW, van der Gaast A; CROSS study group. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16:1090-1098. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1292] [Cited by in RCA: 1929] [Article Influence: 175.4] [Reference Citation Analysis (0)] |
| 13. | Ke M, Wu X, Zeng J. The treatment strategy for tracheoesophageal fistula. J Thorac Dis. 2015;7:S389-S397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 35] [Reference Citation Analysis (0)] |
| 14. | Freitag L, Tekolf E, Steveling H, Donovan TJ, Stamatis G. Management of malignant esophagotracheal fistulas with airway stenting and double stenting. Chest. 1996;110:1155-1160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 86] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Herth FJ, Peter S, Baty F, Eberhardt R, Leuppi JD, Chhajed PN. Combined airway and oesophageal stenting in malignant airway-oesophageal fistulas: a prospective study. Eur Respir J. 2010;36:1370-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | Włodarczyk J, Kużdżał J. Double stenting for malignant oesophago-respiratory fistula. Wideochir Inne Tech Maloinwazyjne. 2016;11:214-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koyanagi K, Ono T S-Editor: Wang YQ L-Editor: A E-Editor: Wu YXJ