Published online Dec 26, 2019. doi: 10.12998/wjcc.v7.i24.4420
Revised: November 22, 2019
Accepted: November 30, 2019
Published online: December 26, 2019
Processing time: 100 Days and 5.7 Hours
Extramedullary myelinolysis is a rare demyelinating disease, often caused by rapid increases in serum sodium concentration in patients with hyponatremia. Clinical manifestations are neuropsychiatric symptoms, limb weakness, and dysarthria. Because of its poor prognosis and high disability rate, it poses a huge burden on the global economy, societies, and families. This article reports rehabilitation in a patient with pituitary dysfunction combined with extramedullary myelinolysis.
A 27-year-old Chinese man developed anorexia, vomiting, and limb weakness and was diagnosed with pituitary insufficiency. He had low serum sodium, slow movement, muscle weakness, and muscle tone abnormalities after sodium supplementation, involuntary limb shaking, ataxia, and dysarthria. According to the symptoms and signs and imaging reports, he was diagnosed with extramedullary myelinolysis. After treatment with hormone therapy and neurotrophic drugs, motor and speech function did not improve, so he was treated in the rehabilitation department for 4 wk. The patient’s physical status was improved substantially during his stay at the rehabilitation department.
Patients with extramedullary myelinolysis who actively participate in rehabilitation intervention can significantly improve their activities of daily living.
Core tip: Medical treatment of extramedullary myelinolysis is beneficial for alleviating development of the disease, but treatment of patients with motor dysfunction, dysarthria, and other complications is poor, leading to difficulties in patient daily living, self-care, and social activity. Active intervention in rehabilitation has a beneficial effect on patient functional recovery.
- Citation: Yang MX, Chen XN. Rehabilitation of anterior pituitary dysfunction combined with extrapontine myelinolysis: A case report. World J Clin Cases 2019; 7(24): 4420-4425
- URL: https://www.wjgnet.com/2307-8960/full/v7/i24/4420.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i24.4420
Anterior hypopituitarism is caused by hypophyseal lesions of different types, which lead to hypophysin secretion deficiency and secondary hypofunction of thyroid and adrenal glands. Adrenocortical dysfunction may cause abnormal water and sodium metabolism and hyponatremia[1]. Under these conditions, if serum sodium is rapidly corrected, cell metabolic disorder[2] and osmotic demyelination syndrome may occur in the central nervous system (CNS). Usually, osmotic demyelination syndrome includes central pontine and extrapontine myelolysis. Clinical features include dysarthria, quadriplegia, dyskinesia, encephalopathy, or atresia syndrome[3]. Generally, the prognosis of demyelinating diseases is poor and there is no effective treatment[4]. Therefore, it is suggested that patients should receive active rehabilitation including physical therapy, occupational therapy, and speech therapy[5].
A 27-year-old Chinese man with pituitary dysfunction presented with unclear speech and unstable walking for > 6 mo.
On February 21, 2019, the patient had oral ulcers and gradually developed anorexia, nausea, vomiting, constipation and limb weakness, pallor, and consciousness disorder. He went to the hospital for treatment, and was diagnosed with anterior pituitary hypofunction, pituitary crisis, and pituitary microadenoma. Serum sodium level was 102.7 mmol/L and he was treated with a high concentration of saline sodium. Over the next 3 d, serum sodium increased to 121.8, 134.5, and 137.7 mmol/L. Levels of sex hormones, growth hormone, and thyroid function were lower than normal. During hospitalization, the patient was treated with sodium, potassium, glucocorticoid, thyroid hormone and androgen supplementation, anti-infective agents, and gastric mucosal protective agents.
After discharge on March 2, 2019 the patient developed speech difficulties, nausea, retching, constipation, fatigue, involuntary limb shaking, poor eating, and reduced stool frequency. He was readmitted on March 12, 2019. Pituitary computed tomography (CT) showed suspicious nodular foci, and cerebral CT showed multiple low-density lesions in the bilateral basal ganglia. Cranial magnetic resonance imaging (MRI) and diffusion-weighted imaging showed abnormal signals in the bilateral caudate nucleus and globus symmetry abnormality, which suggested metabolic or toxic encephalopathy; vacuolar saddle signs; and left and upper sinus submucosal cysts. The diagnosis was anterior pituitary hypofunction, extramedullary myelinolysis, and pituitary microadenomas. During hospitalization, he was treated with glucocorticoids, thyroid hormone supplementation, and anti-infective agents, which improved neurological function and nutritional status. At the time of discharge on March 25, 2019, there was no obvious relief in the symptoms, his speech was defective, and he had involuntarily limb shaking and increased muscle tension in the limbs. After repeated hospitalization in the endocrinology and neurology departments, the above symptoms were not significantly relieved. On July 25, 2019, he was treated in the department of rehabilitation medicine.
Seventeen years ago, the patient showed no obvious incentive for growth and development, his growth rate slowed down compared with that of his peers, and his height was significantly shorter.
The patient had no significant past history or family history.
The patient was conscious, spirited, of short stature, and had a female face. His speech was defective, and he did not cough when drinking water. The pupils on both sides were about 3.0 mm in diameter, and directly and indirectly sensitive to light reflection; nystagmus was absent, and tongue tremor was present. He had normal facial muscle activity, soft neck, and weak neck shrug. Manual muscle testing (MMT) scores were as follows: bilateral supraspinatus muscle: 3 points (active movement against gravity); left biceps brachii and triceps brachii muscle: 4 points (active movement against gravity and resistance); right biceps brachii and triceps brachii muscle: 3 points; muscles associated with hand grip: 3 points; muscles of the left and right waists: 4 points; left and right hip flexors: 4 points; and left and right hip extensors: 3 points. Muscle tension in the limbs was normal. There were no obvious abnormalities in the bilateral deep and shallow sensation and complex sensation. He could maintain a dynamic balance while standing, and exercise was slow. Physiological reflexes were weakened and pathological reflexes were not elicited. Activities of daily living (ADL) score was 60 points (Table 1).
| Items | Admission | Discharge |
| Eating | 5 | 10 |
| Bathing | 0 | 5 |
| Grooming | 0 | 5 |
| Dressing | 5 | 10 |
| Bowel management | 10 | 10 |
| Bladder management | 10 | 10 |
| Toileting | 10 | 10 |
| Bed, chair, wheelchair transfer | 10 | 15 |
| Walking | 10 | 15 |
| Stairs | 0 | 10 |
| Total | 60 | 100 |
Laboratory test results were within normal limits.
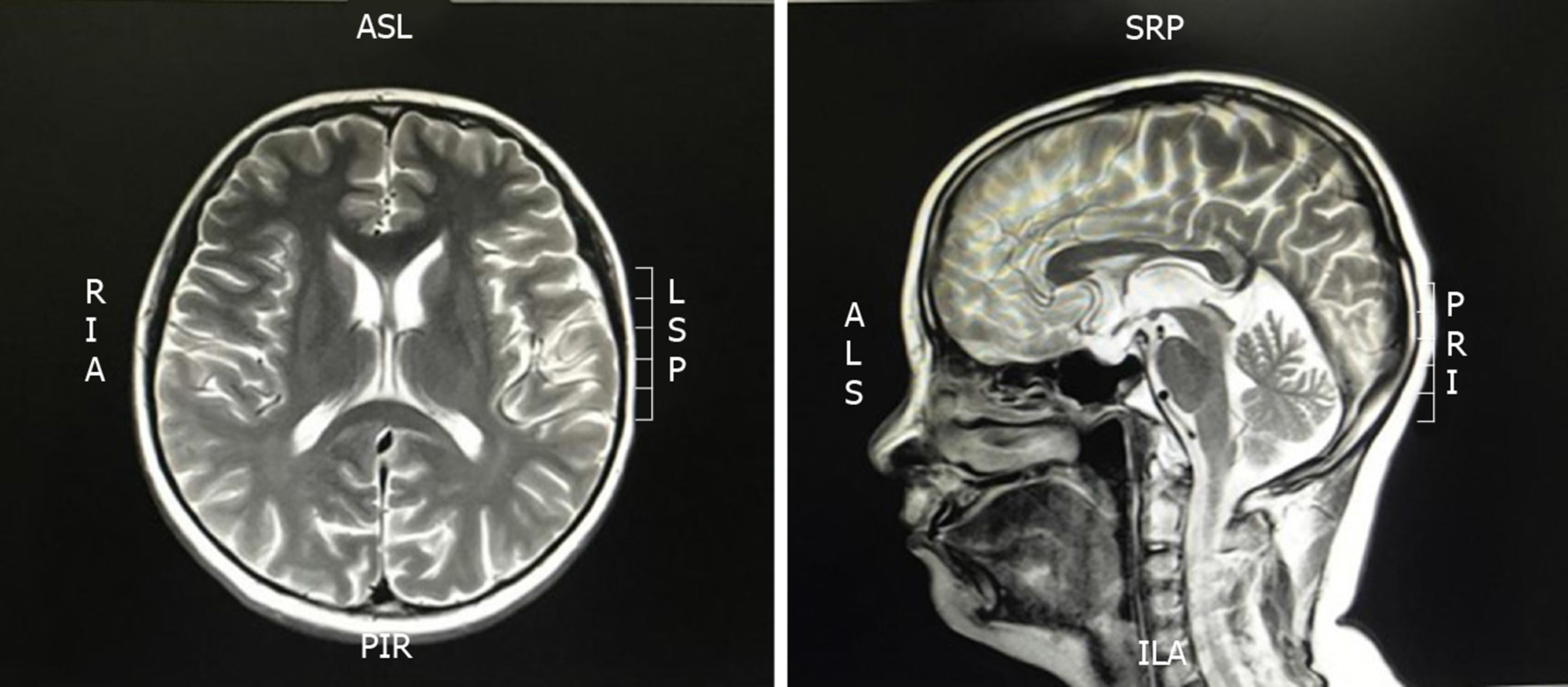
MRI craniocerebral plain scan on July 29, 2019 showed bilateral white globular abnormal signal, suspected hepatic encephalopathy, hepatocellular nuclear disease, and empty sella syndrome (Figure 1).
Extrapontine myelinolysis and pituitary dysfunction.
Rehabilitation: To promote CNS recovery by hyperbaric oxygen therapy daily (qd), to ensure adequate oxygen supply to the CNS to promote recovery of damaged nerves; provide comprehensive training for limbs qd, to increase limb muscle strength, and prevent disuse atrophy; joint treatment for limbs qd, to improve exercise and coordination function; for both hands with fine motor dysfunction, two-hand function training qd, to improve hand joint mobility, flexibility, grip, side pinch and other functions; hand exercise qd. Acupuncture treatment qd, to increase muscle strength, improve swallowing dysphonia, and promote CNS feedback to improve motor control. Popsicles were used to stimulate muscles in the mouth, low-frequency pulse electrotherapy was used to stimulate the throat muscles, and alphabet and pronunciation training was given to improve dysarthria.
Medication: Ganglioside 40 mg, i.v. qd; levothyroxine tablets 50 μg po qd; vitamin B1 tablets 10 mg po qd; and prednisolone acetate tablets 5 mg po qd were administered.
His speech was improved although still unclear, and he had no dizziness or fatigue. Mental condition was normal. Physical examination showed stable vital signs, good cooperation with examiners, and dysarthria. Ocular tremor was absent, tongue tremor was present, facial muscle activity was normal, neck was soft, and neck shrug was strong. MMT scores after treatment were all increased to 5 points except for muscles associated with hand grip with an increased score to 4 points, in which 5 points is defined as having normal muscle strength with active movement against full resistance without evident fatigue. There was no obvious abnormality in the bilateral deep and shallow sensation and complex sensation. The standing balance was normal. Bilateral knee reflex, Achilles tendon reflex, periosteal reflex and biceps reflex had no obvious abnormalities. Babinski sign, Brudzinski sign, Hoffmann sign, and finger test were negative. ADL score at discharge was 100 points (Table 1) (Figure 2).
Adrenocorticotropic hormone, produced by hypophysis, stimulates the production and secretion of adrenocortical hormone. Secondary adrenal insufficiency occurs when the anterior pituitary function is impaired. When adrenal insufficiency occurs, aldosterone secretion decreases and water and sodium excretion increase. In addition, the decrease of cortisol hormone can promote the secretion of antidiuretic hormone, causing the decrease of water excretion and hyponatremia. After rapid correction of sodium, demyelination of the CNS may occur. Patients with extramedullary myelinolysis have various behavioral abnormalities such as dance-like movements, lethargy, and apathy. The extrapyramidal symptoms can be expressed as skeletal muscle loss, parkinsonism, and hand and foot movements[2,6]. The mechanism is not completely clear at present, and the current view is that the steady-state condition of nerve cells depends on the migration of inorganic ions inside and outside the cell. When serum sodium is quickly corrected, the external conditions change. If the ion exchange of the cells does not reach equilibrium, the cells either synthesize the organic permeate or transport the ions from the external environment into the cell. Both methods need energy and time; if the extracellular tension rises too fast, the cells are not able to maintain osmotic pressure balance, resulting in damage. Oligodendrocytes are particularly susceptible to apoptosis due to the above process. Once patients have osmotic demyelination, it is usually only partially reversible[7] and drug therapy is essential. Thyroid-stimulating hormone and corticosteroids are effective, and plasma exchange is also used to treat extrapontine myelinolysis. In addition to active drug treatment, it is equally important to improve the quality of life of patients and prevent complications such as aspiration pneumonia, deep vein thrombosis and pulmonary embolism[8]. Therefore, such patients should actively carry out rehabilitation interventions to reduce morbidity and mortality.
Hyperbaric oxygen therapy is considered to improve blood circulation and perfusion, promote fibroblast growth, supply oxygen to damaged tissues, increase neuronal oxygen reserve, promote reversible nerve fiber regeneration and remyelination, and increase aerobic metabolism[9]. It has a good therapeutic effect on demyelination.
In the present case, before treatment, the patient’s limb movement was slow, his limbs performed daily life tasks poorly, and muscle strength was weak. He could only maintain a dynamic balance while standing. Therefore, he was treated mainly by comprehensive training for limbs, including the methods of proprioceptive neuromuscular facilitation and motor relearning program, to improve limb mobility and enhance muscle strength. After 2 wk, the patient’s muscle strength was significantly improved. At that time, motor function focused on coordination ability, and joint treatment of the limbs promoted coordinated movement of hands and feet to improve balance and walking function[10]. In addition, joint treatment of limbs improved motor function while preventing complications such as muscle atrophy, muscle contracture, and lung infection[11,12].
Two-hand function training and occupational therapy can improve hand function. Poor fine movement of the hands means that movement is slow. By functional training, flexibility of the hands is improved, hand-eye coordination training is emphasized, and the hand grip is improved. Occupational therapy is used to increase hand movement of patients’ daily tasks, which is important for improving activities of daily living and quality of life[13].
Acupuncture is believed to improve nerve conduction function, activate brain nerve function, increase muscle strength, and promote motor function recovery. Acupuncture protects the myelin sheath by promoting oligodendrocyte proliferation and inhibiting glial cell death[14]. Acupuncture in the oropharynx can improve dysarthria and swallowing function.
Consonant function training, oral ice stimulation, and pulse electrotherapy are also used in patient rehabilitation. All types of dysarthria will have false vocalization. The reason is that dysfunction of the soft palate leads to insufficient oral pressure. Oral ice stimulation involves cold stimulation of oral muscle contraction, and increases muscle strength of muscles such as the tongue. Pulse electrotherapy uses electrical impulses to stimulate the throat muscles and enhance feedback. Articulation training establishes a normal pronunciation pattern using syllable training, corrects wrong articulation, and improves dysarthria.
Active rehabilitation for patients with extramedullary myelinolysis can improve the coordination and fine movement of patients, and significantly restore activities of daily living, but the recovery of speech function is slow.
| 1. | Yamamoto T, Fukuyama J, Kabayama Y, Harada H. Dual facets of hyponatraemia and arginine vasopressin in patients with ACTH deficiency. Clin Endocrinol (Oxf). 1998;49:785-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Singh TD, Fugate JE, Rabinstein AA. Central pontine and extrapontine myelinolysis: a systematic review. Eur J Neurol. 2014;21:1443-1450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 183] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 3. | Cheo SW, Low QJ, Tan YA, Kang CY. Trident sign in Osmotic Demyelination Syndrome. QJM. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Kamil K, Yazid MD, Idrus RBH, Das S, Kumar J. Peripheral Demyelinating Diseases: From Biology to Translational Medicine. Front Neurol. 2019;10:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Yuridullah R, Kumar V, Nanavati S, Singhal M, Chandran C. Clinical Resolution of Osmotic Demyelination Syndrome following Overcorrection of Severe Hyponatremia. Case Rep Nephrol. 2019;2019:1757656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Babanrao SA, Prahladan A, Kalidos K, Ramachandran K. Osmotic myelinolysis: Does extrapontine myelinolysis precede central pontine myelinolysis? Report of two cases and review of literature. Indian J Radiol Imaging. 2015;25:177-183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Garg P, Aggarwal A, Malhotra R, Dhall S. Osmotic Demyelination Syndrome - Evolution of Extrapontine Before Pontine Myelinolysis on Magnetic Resonance Imaging. J Neurosci Rural Pract. 2019;10:126-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Zhou Y, Zhu Y, Wang W, Xing B. Preoperative Extrapontine Myelinolysis with Good Outcome in a Patient with Pituitary Adenoma. J Korean Neurosurg Soc. 2016;59:161-164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Carrì MT, Valle C, Bozzo F, Cozzolino M. Oxidative stress and mitochondrial damage: importance in non-SOD1 ALS. Front Cell Neurosci. 2015;9:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Byun SD, Jung TD, Kim CH, Lee YS. Effects of the sliding rehabilitation machine on balance and gait in chronic stroke patients - a controlled clinical trial. Clin Rehabil. 2011;25:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Sohn MK, Nam JH. Locked-in Syndrome due to Central Pontine Myelinolysis: Case Report. Ann Rehabil Med. 2014;38:702-706. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Louis G, Megarbane B, Lavoué S, Lassalle V, Argaud L, Poussel JF, Georges H, Bollaert PE. Long-term outcome of patients hospitalized in intensive care units with central or extrapontine myelinolysis*. Crit Care Med. 2012;40:970-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Baron H, Hawrylyshyn N, Hunt SS, McDougall J. Understanding quality of life within occupational therapy intervention research: A scoping review. Aust Occup Ther J. 2019;66:417-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Huang S, Tang C, Sun S, Cao W, Qi W, Xu J, Huang J, Lu W, Liu Q, Gong B, Zhang Y, Jiang J. Protective Effect of Electroacupuncture on Neural Myelin Sheaths is Mediated via Promotion of Oligodendrocyte Proliferation and Inhibition of Oligodendrocyte Death After Compressed Spinal Cord Injury. Mol Neurobiol. 2015;52:1870-1881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Helias Tzamaloukas AH S-Editor: Zhang L L-Editor: Filipodia E-Editor: Liu JH