Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3772
Peer-review started: August 11, 2019
First decision: September 9, 2019
Revised: September 19, 2019
Accepted: October 15, 2019
Article in press: October 15, 2019
Published online: November 26, 2019
Processing time: 112 Days and 5.4 Hours
Calcific tendinopathy denotes calcific deposits in a specific tendon. It is also known as calcifying tendinitis, calcifying periarticulitis, or periarticular apatite deposition disease. Recently, extracorporeal shock wave therapy (ESWT) has been reported to be effective in relieving and treating pain in calcific tendinopathy.
A 36-year-old female patient suffered from left hip joint pain for six months. The pain was increased during abduction of the hip, waking, and jumping. B-mode ultrasonography was performed by a physiatrist with an L12-5 linear transducer. A single session of ESWT was given in the marking area under ultrasound guidance at 4 Hz, 2500 shots with intensity of stimulation using energy of 0.1 mJ/mm2. The hip pain of the patient slowly decreased within 4 wk after starting the ESWT. After six weeks of ESWT, her hip pain was completely resolved. However, the size of calcification showed almost no reduction in simple radiography at the final follow-up.
Ultrasonography is a very good modality not only for diagnosing calcified tendinitis by classical appearance, but also for evaluating the effect of ESWT during the follow-up period.
Core tip: As a feature of ultrasonography, high resolution shows the presence of deposits and defines their locations in the tendon, plus their size and texture. This technique enables staging of the deposits by correlation of shadow cones. In the resting phase, the deposits appear hyperechoic and arc shaped, whereas they appear non-arc shaped (fragmented/punctate and cystic) in the resolving phase. These appearances can also be correlated with the symptomatic and asymptomatic phases of the disease.
- Citation: Lee CH, Oh MK, Yoo JI. Ultrasonographic evaluation of the effect of extracorporeal shock wave therapy on calcific tendinopathy of the rectus femoris tendon: A case report. World J Clin Cases 2019; 7(22): 3772-3777
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3772.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3772
Calcific tendinopathy denotes calcific deposits in a specific tendon. It is also known as calcifying tendinitis, calcifying periarticulitis, or periarticular apatite deposition disease[1,2]. Causes of calcific tendinopathy have not been clearly clarified yet. According to previous studies, repeated use of attachment site and focal ischemia, cartilage degeneration, and calcium deposition at the tendon attachment site are main causes of calcific tendinopathy. In addition, severe acute or chronic pain frequently occurs due to degradation of calcium deposits. To treat calcific tendinopathy, various methods have been used, including administration of nonsteroidal antiinflammatory drugs (NSAID) to the calcified lesion, needle aspiration, and extracorporeal shock wave therapy (ESWT). However, surgical treatment is rarely necessary.
Recently, ESWT has been reported to be effective in relieving and treating pain in calcific tendinopathy[3]. Investigating treatment effects is usually based on clinical measurement and typical findings of plain radiography, locating calcific depositions in the tendon or bursa[4]. However, plain radiography can lead to mistakes without additional check-up with other diagnostic tools such as computed tomography (CT) or magnetic resonance image (MRI). Recently, a few studies have used ultrasonography to determine the effect of treatment on calcific tendinopathy[5,6]. However, there are only two reports of ESWT for treating calcified tendinopathy around hip joint compared to that for treating calcified tendinopathy of rotator cuff or Achilles tendon[1,2].
To the best of our knowledge, no case report has described the usefulness of ultrasonography in the treatment of calcific tendinopathy around rectus femoris tendon using ESWT. Herein, we report a case of calcific tendinopathy of rectus femoris successfully treated with ESWT. Our case shows the importance of using ultrasonography to determine the effect of treatment when simple radiography does not reveal difference of calcific deposit over the rectus femoris tendon.
A 36-year-old female patient suffered from left hip joint pain for six months. The pain was increased during abduction of the hip, waking, and jumping.
Initially, the pain was treated with acetaminophen, with some success. Symptoms subsided the following day but recurred quite severely on the third day, requiring admission to a community hospital for treatment. The pain was non-radiating and was exacerbated with any movement of the left hip. There was no fever, chills, preceding systemic illness, or infection.
Since then, there was no pain improvement even after 6 mo of continuous treatment.
No other health conditions are reported.
She had no specific history of trauma or underlying disease.
On physical examination, limitation of range of motion was revealed due to pain. No evidence of infection was observed. There was evidence of infection such as fever, heating sensation, redness, fluctuation, and swelling.
All routine laboratory findings were within normal limits.
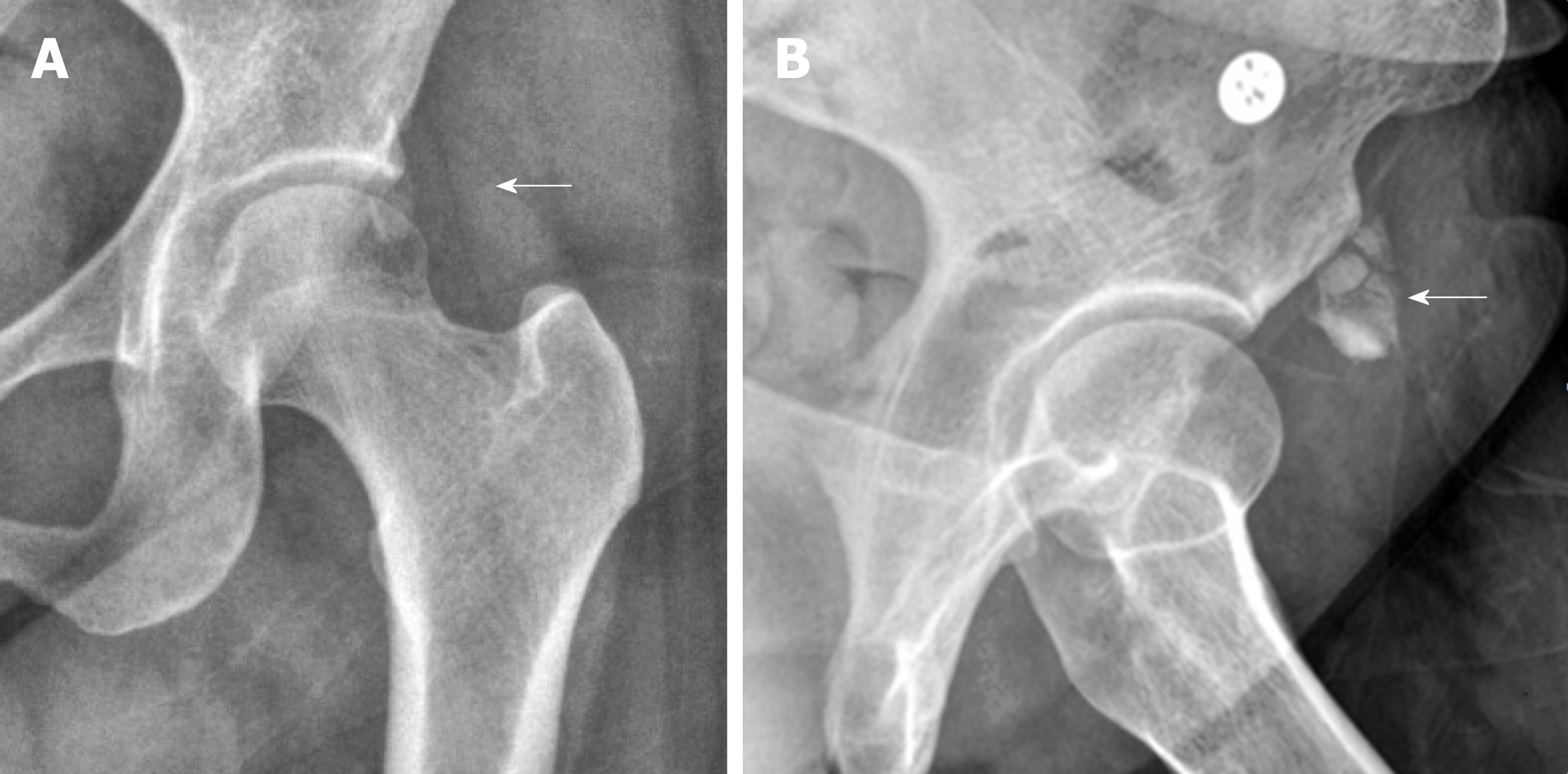
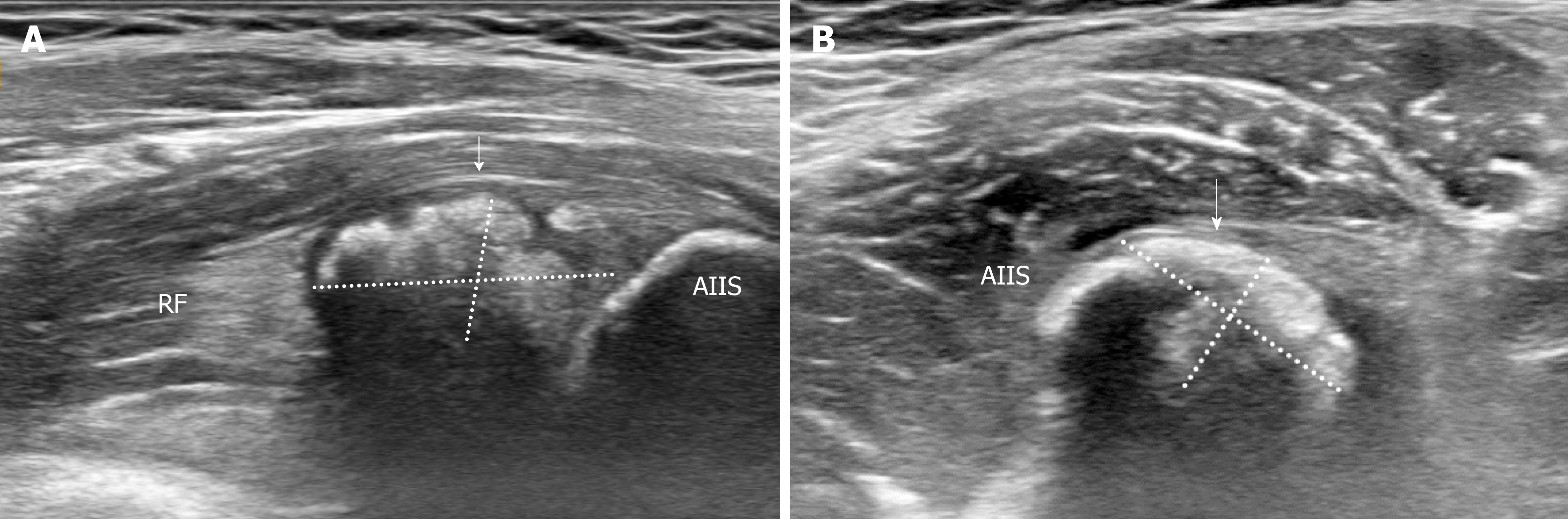
Simple radiograph including anteroposterior view and lateral view revealed nodular-shaped deposits at the anterior inferior iliac spine site as the origin of rectus femoris muscle (Figure 1). For further evaluation and ESWT, B-mode ultrasonography was performed by a physiatrist with expertise in using a Philips iU 22 ultrasound system (Philips Health Care, Andover, MA, United States) with an L12-5 linear transducer. The patient was asked to lie in a supine position on the examination table while her knee was straightened and the ankle was relaxed. Longitudinal and transverse ultrasonographic images of the calcification of the left rectus femoris were evaluated before ESWT (Figure 2). Dornier Aries (Dornier MedTech, Wessling, Germany) was used for ESWT.
Calcific tendinitis of rectus femoris muscle.
We marked the calcification with a pen to accurately deliver shock wave. Pressure pulses were focused at the marking area that was identified through the ultrasound. A single session of ESWT was given in the marking area under ultrasound guidance at 4 Hz, 2500 shots with intensity of stimulation using energy of 0.1 mJ/mm2. ESWT was performed a total of six times at an interval of 3-4 d. The patient’s posture was the same as that of the ultrasound scan. Complementary NSAIDs (Celecoxib) were started.
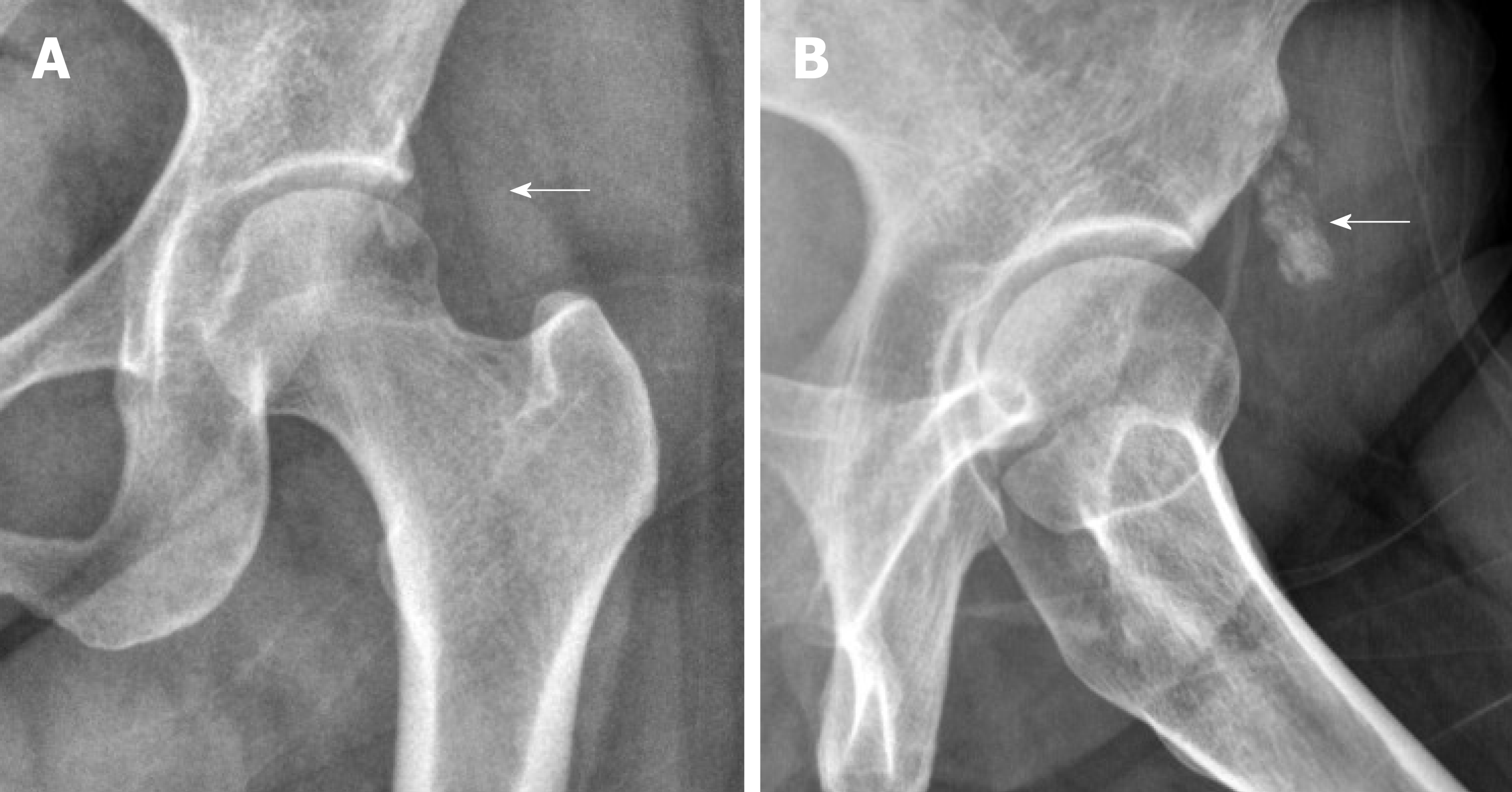
The hip pain of patient slowly decreased within four weeks after starting the ESWT. After 6 wk, her hip pain was completely resolved. However, the size of calcification showed almost no reduction in simple radiography at the final follow-up (Figure 3). We performed ultrasonography, showing that calcium deposit was decreased, with huge calcification disintegrated into smaller pieces on transverse image (Figure 4).
Several cases of calcific tendinopathy of the rectus femoris have been reported[7]. However, there is only one report of treatment using ESWT of calcified tendinopathy of the rectus femoris[1]. In that report, ESWT was administered in a total of three sessions at 7-d interval. The calcification was disintegrated in a month after ESWT and the pain was resolved completely at final 15-mo follow-up with complete resorption of calcific material in radiography. Calcific tendinopathy is usually a self-limiting condition. In light of this, improved pain after 15 mo can be caused by the natural course of pain, not by ESWT. In our case, ESWT was performed a total of six times. After six weeks of ESWT, calcium deposit showed almost no change in the radiography. However, calcium deposit was decreased and fragmented on ultrasonographic findings and her hip pain was completely resolved.
Conventional radiography is the technique used most frequently for the detection of calcifications in calcific tendinopathy. However, plain radiography can lead to misdiagnosis without the use of additional diagnostic tools because of the limitation of two-dimensional projections[8]. CT allows the best visualization and localization in calcific tendinopathy. It is rarely used for the assessment of non-traumatic joint[9].
If possible, MRI can be an useful tool to diagnosis calcific tendinopathy as it confirms the presence of inflammation associated with the acute symptomatic phase of calcific tendinopathy excluding other etiologies of pain[10]. Although these diagnostic tools could be used for additional examination, they are not appropriate as screening test because they are associated with high radiation and excessive cost. On the other hand, ultrasonography is useful for evaluating of calcific tendinopathy. Especially, the real-time nature of ultrasonography allows its use for both diagnostic and therapeutic purpose. In our patient, a huge calcific nodule disintegrated and showed reduction in size after ESWT. Even if it was not real-time, ESWT was exactly applied to the calcified nodule by marking the calcification with a pen under ultrasound guidance. As a feature of ultrasonography, high resolution shows the presence of deposits and defines their locations in the tendon, plus their size and texture. This technique enables staging of deposits by correlation of shadow cones. In the resting phase, deposits appear hyperechoic and arc shaped, whereas they appear non-arc shaped (fragmented/punctate and cystic) in the resolving phase. These appearances can also be correlated with symptomatic and asymptomatic phases of the disease. In our study, we founded that larger and more arc shaped calcification changed into smaller fragmented calcification after ESWT through ultrasonography.
In conclusion, ultrasonography is a very good modality not only for diagnosing calcified tendinitis based on classical appearance, but also for evaluating the effect of ESWT during follow-up period.
| 1. | Oh KJ, Yoon JR, Shin DS, Yang JH. Extracorporeal shock wave therapy for calcific tendinitis at unusual sites around the hip. Orthopedics. 2010;33:769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Durst HB, Kuster MS. [Extracorporeal shock-wave lithotripsy for the treatment of calcific tendonitis of the glutaeus maximus tendon]. Z Orthop Ihre Grenzgeb. 2006;144:516-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Speed CA, Nichols D, Richards C, Humphreys H, Wies JT, Burnet S, Hazleman BL. Extracorporeal shock wave therapy for lateral epicondylitis--a double blind randomised controlled trial. J Orthop Res. 2002;20:895-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 119] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Chow HY, Recht MP, Schils J, Calabrese LH. Acute calcific tendinitis of the hip: case report with magnetic resonance imaging findings. Arthritis Rheum. 1997;40:974-977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Jo H, Kim G, Baek S, Park HW. Calcific Tendinopathy of the Gluteus Medius Mimicking Lumbar Radicular Pain Successfully Treated With Barbotage: A Case Report. Ann Rehabil Med. 2016;40:368-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Hong MJ, Kim YD, Park JK, Kang TU. Successful Treatment of Rectus Femoris Calcification with Ultrasound-guided Injection: A Case Report. Korean J Pain. 2015;28:52-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | IKobayashi H, Kaneko H, Homma Y, Baba T, Kaneko K. Acute Calcific Tendinitis of the Rectus Femoris: A Case Series. J Orthop Case Rep. 2015;5:32-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 8. | Farin PU, Räsänen H, Jaroma H, Harju A. Rotator cuff calcifications: treatment with ultrasound-guided percutaneous needle aspiration and lavage. Skeletal Radiol. 1996;25:551-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 110] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Farin PU. Consistency of rotator-cuff calcifications. Observations on plain radiography, sonography, computed tomography, and at needle treatment. Invest Radiol. 1996;31:300-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Holt PD, Keats TE. Calcific tendinitis: a review of the usual and unusual. Skeletal Radiol. 1993;22:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bazeed MF, Gao BL, Valek V S-Editor: Dou Y L-Editor: A E-Editor: Liu MY