Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3742
Peer-review started: August 14, 2019
First decision: October 14, 2019
Revised: October 21, 2019
Accepted: October 30, 2019
Article in press: October 30, 2019
Published online: November 26, 2019
Processing time: 103 Days and 11.1 Hours
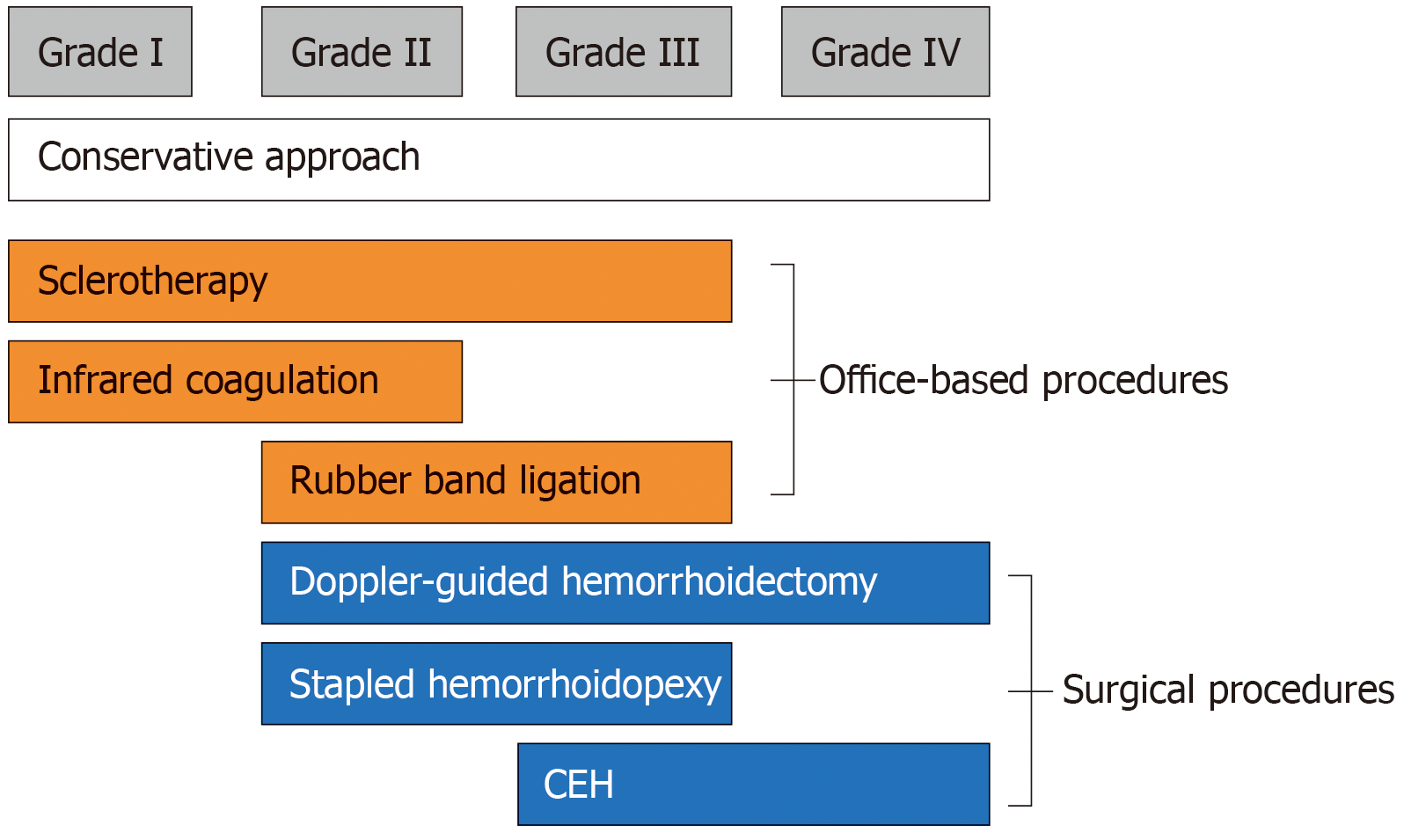
Hemorrhoidal disease is the most common anorectal disorder. Hemorrhoids can be classified as external or internal, according to their relation to the dentate line. External hemorrhoids originate below the dentate line and are managed conservatively unless the patient cannot keep the perianal region clean, or they cause significant discomfort. Internal hemorrhoids originate above the dentate line and can be managed according to the graded degree of prolapse, as described by Goligher. Generally, low-grade internal hemorrhoids are effectively treated conservatively, by non-operative measures, while high-grade internal hemorrhoids warrant procedural intervention.
To determine the application of clinical practice guidelines for the current management of hemorrhoids and colorectal surgeon consensus in Australia and New Zealand.
An online survey was distributed to 206 colorectal surgeons in Australia and New Zealand using 17 guideline-based hypothetical clinical scenarios.
There were 82 respondents (40%) to 17 guideline-based scenarios. Nine (53%) reached consensus, of which only 1 (6%) disagreed with the guidelines. This was based on low quality evidence for the management of acutely thrombosed external hemorrhoids. There were 8 scenarios which showed community equipoise (47%) and they were equally divided for agreeing or disagreeing with the guidelines. These topics were based on low and moderate levels of evidence. They included the initial management of grade I internal hemorrhoids, grade III internal hemorrhoids when initial management had failed and the patient had recognised risks factors for septic complications; and finally, the decision-making when considering patient preferences, including a prompt return to work, or minimal post-operative pain.
Although there are areas of consensus in the management of hemorrhoids, there are many areas of community equipoise which would benefit from further research.
Core tip: Clinical practice guidelines are created to recommend therapies based on the highest levels of evidence. It becomes important to determine whether clinical practice is reflecting management outlined in these guidelines. This paper is the first to assess Australian and New Zealand practice with guidelines in the management of hemorrhoids. While this study has identified areas of colorectal surgeon consensus with hemorrhoid clinical practice guidelines, many more areas of community equipoise have been found, including the initial management of internal hemorrhoids. It is these areas of uncertainty and disagreement which would benefit from high quality research.
- Citation: Fowler GE, Siddiqui J, Zahid A, Young CJ. Treatment of hemorrhoids: A survey of surgical practice in Australia and New Zealand. World J Clin Cases 2019; 7(22): 3742-3750
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3742.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3742
Hemorrhoidal disease is the most common anorectal disorder. In 2011, an epidemiologic study of hemorrhoids revealed a prevalence of 39% in an adult population, of whom 44.7% were symptomatic[1]. Painless rectal bleeding is the hallmark symptom of hemorrhoids, but patients may also experience a sensation or presence of a lump, pruritus ani, swelling or mucous discharge[2].
Hemorrhoids can be classified as external or internal, according to their relation to the dentate line. External hemorrhoids originate below the dentate line and are managed conservatively unless the patient cannot keep the perianal region clean, or they cause significant discomfort[3]. They can also become acutely thrombosed and surgery is advocated within 72 h of the onset of symptoms[3].
Internal hemorrhoids originate above the dentate line and can be managed according to the graded degree of prolapse (Figure 1), as described by Goligher[4]. Generally, low-grade internal hemorrhoids are effectively treated conservatively, by non-operative measures, while high-grade internal hemorrhoids warrant procedural intervention (Figure 1)[3]. Surgery is also used when conservative and office-based measures fail[5].
Decision-making in the management of hemorrhoids is complex and variable[6]. It can be influenced by a myriad of factors, including the site and grade of hemorrhoids, patient characteristics, current guidelines and postoperative complications, including pain and recurrence. Several societies have helped to condense these decisions into guidelines and practice parameters based on the level of evidence[6-10]. Only one recent study has assessed the consensus of current practice with recent clinical practice guidelines and this was a study in the Netherlands[11]. However, no surveys have been done in Australia and New Zealand.
The aim of this survey was to assess the consensus of current colorectal specialist practice in Australia and New Zealand with recent clinical practice guidelines for the management of hemorrhoids[7-10]. In addition to highlighting areas of equipoise that will benefit from future research.
An invitation letter to participate in an anonymous survey was mailed to all members of the Colorectal Surgical Society of Australia and New Zealand (CSSANZ). The letter included a survey link to RED Cap, a secure web application which was used to collect the data, and was hosted at The University of Sydney[12].
The University of Sydney Human Ethics Research Committee granted ethics approval (ref. 2017/416) and the CSSANZ Research Support Committee approved dissemination of the invitation letters. A reminder letter to participate was sent after two weeks to non-respondents.
The survey collected demographic data including age, gender and location of subspecialty training and practice. It also consisted of seventeen clinical scenarios to capture the correlation of current practice in the management of hemorrhoids with recent guidelines[7-10]. An additional scenario was excluded from data analysis as a duplication error. The scenarios had four to five multiple choice responses with one or several responses matching to guideline recommendations. The areas covered included the management of both primary and recurrent internal hemorrhoids for each of the graded degrees of prolapse, and the various presentations of external hemorrhoids, whether small, large, simple or thrombosed. All scenarios were presentations based on a 35-year-old adult.
Statistical analysis was performed using IBM SPSS Statistics Version 22. Demographics were tabulated and descriptive statistics were calculated (proportion and mean ± SD).
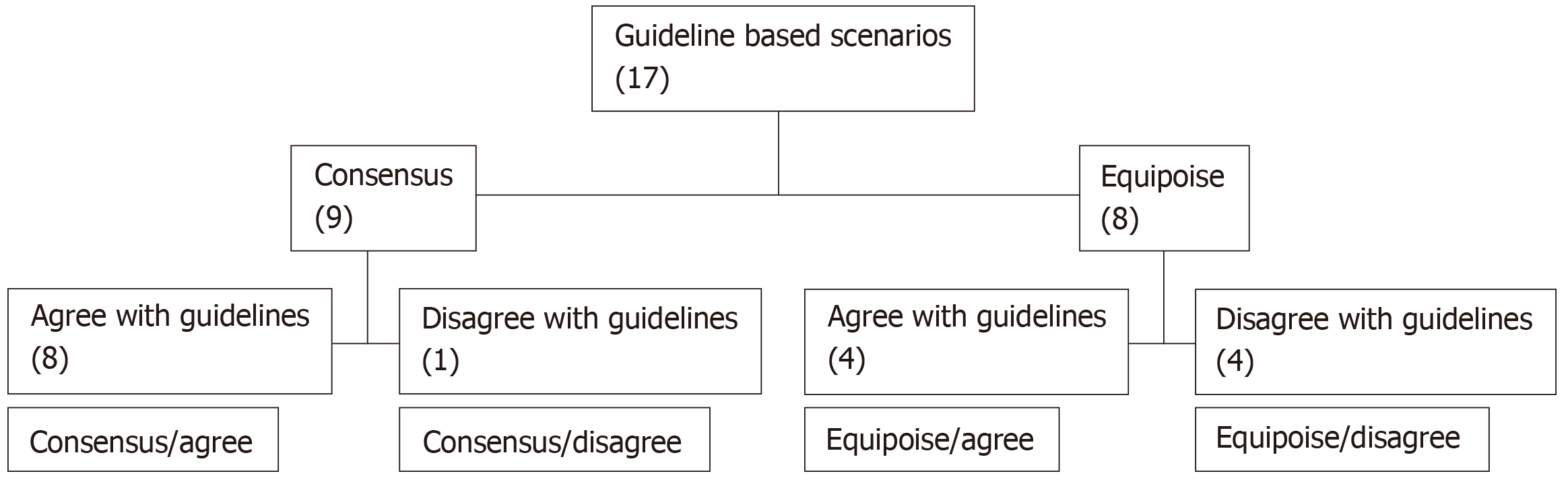
Evidence suggests community equipoise is low when > 70% of respondents choose a treatment option[13]. In this study, two groups were formed, those which agreed with guideline recommended responses for each scenario and the proportion forming a majority for a response. Thus, community equipoise was then assessed by classifying the survey scenarios into one of four categories: (1) Consensus/Agree: scenarios with > 70% of respondents choosing an option that agrees with guideline recommendations; (2) Consensus/Disagree: scenarios with > 70% of respondents choosing an option that disagrees with guideline recommendations; (3) Equipoise/Agree: scenarios with ≤ 70% of respondents choosing an option that agrees with guideline recommendations; and (4) Equipoise/Disagree: scenarios with ≤ 70% of respondents chose an option that disagrees with guideline recommendations.
All demographic data were tested for their association between these two groups. Univariate analysis was performed using the χ2 test or Fisher’s exact test. Multivariate logistic regression analysis was performed to assess associations between covariates. P values ˂ 0.05 were considered significant.
There were 82 respondents (40%) of the 205 members of the CSSANZ. Surgeon demographics are summarised in Table 1. Over half (57%) of the surgeons were ≥ 50 years old and the average years in practice was 16.8, Ninety percent were male. The majority (79.3%) worked in a city at a secondary referral centre. Eight-three percent practised in Australia and the majority (66%) did their subspecialist training (66%) in Australia/New Zealand.
| Characteristic | n (%) |
| Age range (yr) | |
| 30–39 | 7 (8) |
| 40–49 | 29 (35) |
| 50–59 | 30 (37) |
| Over 60 | 16 (20) |
| Gender | |
| Male | 74 (90) |
| Female | 8 (10) |
| Area of practice | |
| City (tertiary/quaternary referral centre) | 11 (13.4) |
| City (secondary referral) | 65 (79.3) |
| Rural and regional | 6 (7.3) |
| Location of practice | |
| New Zealand | 14 (17) |
| Australia | 68 (83) |
| New South Wales | 24 (29) |
| Victoria | 18 (22) |
| South Australia | 7 (9) |
| Western Australia | 4 (5) |
| Queensland | 15 (18) |
| Location of subspecialty traininga | |
| Australia/New Zealand | 54 (66) |
| Europe | 21 (25) |
| North America | 8 (9) |
| Average years in practice (yr ± SD) | 16.8 ± 9.7 |
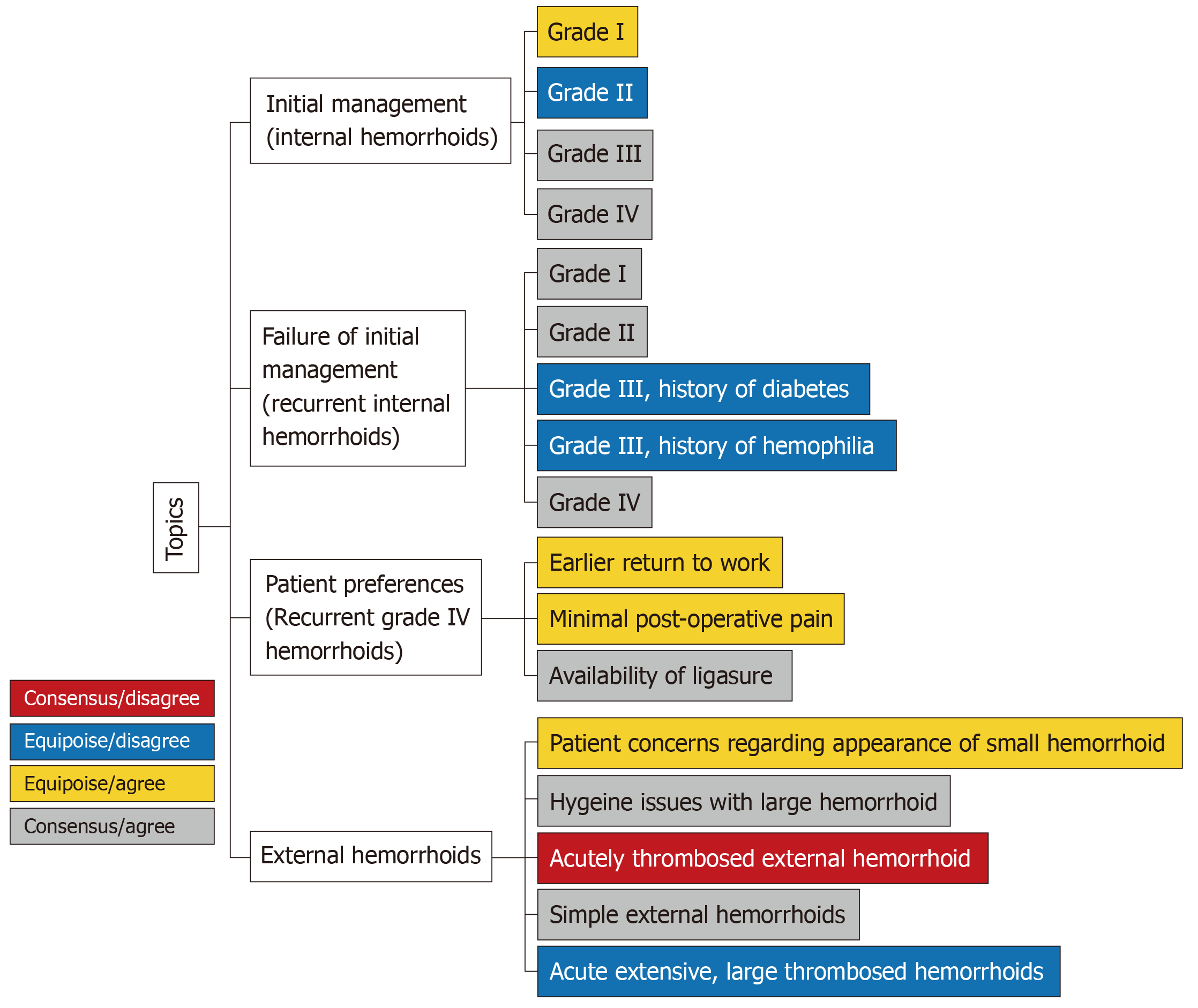
There were 17 clinical based scenarios, of which 9 (53%) reached consensus and only one (6%) disagreed with guidelines (Figure 2). There were 8 (47%) scenarios which showed community equipoise, and these were equally split for agreeing or disagreeing with the guidelines.
Grade I (Equipoise, agree): The majority (67%) would initially advocate lifestyle changes, in concordance with guidelines, while 32% would opt for an office-based procedure, with 24% choosing rubber band ligation (RBL), 6% sclerotherapy and 1% both. The remaining 1% would “band and inject”.
Grade II (Equipoise, disagree): The majority opinion (65%) was to perform RBL, which was a less popular choice for European trained surgeons than non-European trained (44% vs 72%, X2P = 0.039). Only 27% of surgeons would initially advocate lifestyle changes, in concordance with guidelines.
Grade III (Consensus, agree): Eighty-nine percent of respondents would initially perform an office-based (78%) or operative treatment (11%), with the majority choosing RBL (44%) and none would perform Doppler-guided hemorrhoidectomy (DGH). The remaining 11% of respondents would initially advocate lifestyle changes.
Grade IV (Consensus, agree): Eighty-eight percent of respondents would initially perform an office-based (52%) or operative treatment (36%), with 12.5% initially advocating lifestyle changes. There was greater variation on which office-based or operative treatment to perform, compared to the initial management of grade III primary internal hemorrhoids. DGH (20%) and RBL (17%) were the two most popular choices in this scenario.
Grade I (Consensus, agree): The majority (92%) would perform an office-based procedure, with 80% performing RBL, 11% sclerotherapy and 1% performing both.
Grade II (Consensus, agree): Nighty-five percent would perform an office-based procedure, with the majority performing only RBL (92%). Other considerations (5%) were equally divided for lifestyle changes, hemorrhoidal energy therapy and “band and inject”.
Grade III, history of diabetes mellitus (Equipoise, disagree): The majority of respondents chose RBL (61%), despite a patient history of diabetes mellitus being considered an exclusion criteria for this procedure. Other chosen procedures included stapled hemorrhoidectomy (SH; 13%), surgical hemorrhoidectomy (11%), hemorrhoidal artery ligation and recto-anal repair (HAL/RAR; 5%) and sclerotherapy (2%).
Grade III, history of haemophilia (Equipoise, disagree): The majority (30%) would perform surgical hemorrhoidectomy, rather than an office-based procedure (33%) as recommended in the guidelines. Among this, sclerotherapy was the most popular (17%). Other popular decisions included RBL (16%), SH (16%), HAL/RAR (6%) and lifestyle changes (6%).
Grade IV (Consensus, agree): Seventy-three percent would treat these by surgical hemorrhoidectomy, as recommended in the guidelines. This decision was more likely if the surgeon was Australasian trained (81% vs 57% of Europe and North American trained surgeons, χ2P = 0.039). Other favourable decisions included SH (19%) and HAL/RAR (5%).
Grade IV, patient preferences: Prompt return to work after surgery (Equipoise, agree): The majority (58%) would perform SH (24%) or DGH (34%), in concordance with guideline recommendations. Multivariate analysis showed this decision was more likely if the surgeon was aged < 50 years old (85% vs 39%, P = 0.0001) and practiced for less than 17 years (76% vs 33%, P = 0.004) by multivariate analysis. While 36% of respondents would pursue conventional excisional hemorrhoidectomy (CEH), despite the reportedly longer return to normal activities post-procedure.
Grade IV, patient preferences: Minimal post-operative pain (Equipoise, agree): The majority (59%) would choose either SH (22%) or DGH (38%), in concordance with clinical practice guidelines. This decision was more popular if the surgeon was aged < 50 years old (85% vs 42%, Fisher’s exact test P = 0.001) and practised for less than 17 years (84% vs 26%, P = 0.004), as shown by multivariate analysis. Thirty-four percent of respondents would perform CEH despite the higher reported levels of postoperative pain.
Grade IV, patient preferences: Minimal post-operative pain with availability of LigaSure (Consensus, agree): Eighty-nine percent of respondents would manage these surgically, with the majority (38%) performing CEH with LigaSure and only 6% performing CEH without LigaSure. Other popular decisions were DGH (33%) and SH (19%).
Patient concerns regarding the appearance of small hemorrhoids (Equipoise, agree): The majority (52%) would initially advise lifestyle changes, in line with the primary first-line management for patients with symptomatic hemorrhoid disease. Other decisions included office-based procedures (8% RBL and 1% infrared coagulation), CEH (28%) and excision of the tags by a variety of different reported methods (11%).
Hygiene issues with large external component (Consensus, agree): The majority (81%) would perform CEH with LigaSure, while 5% would choose an office-based procedure. Other responses included DGH (5%), SH (3%), HAL/RAR (2%), excision of skin tag (2%) and lifestyle advice (2%).
Acutely thrombosed external hemorrhoids (Consensus, disagree): Eighty-seven percent of surgeons felt these should be managed conservatively, as opposed to the guideline recommendation for surgical excision within 72 h of the onset of symptoms. Only 11% chose the latter.
Simple external hemorrhoids (Consensus, agree): Eighty-four percent would initially manage these conservatively, none would perform an office-based procedure and 8% would perform surgical hemorrhoidectomy.
Acute extensive, large thrombosed hemorrhoids (Equipoise, disagree): The majority (68%) would manage these conservatively, which was a more popular decision for surgeons who had practised greater than 17 years (42% vs 16%, χ2P = 0.022). While 27% would perform CEH in concordance with guideline recommendations. Twenty percent of those practising in a rural setting agreed with current clinical guidelines (20% vs 72%, Fisher’s exact test P = 0.032). A surgeon practising for more than 17 years was less likely to agree with the guideline recommendation (54% vs 78%, χ2P = 0.039).
This is the first survey to evaluate the correlation of current clinical practice in Australia and New Zealand with hemorrhoid clinical practice guidelines. This study has shown community equipoise in at least half of the guideline topics and where there is a consensus, the majority agree with guideline recommendations (Figure 3). Some decisions were found to be dependent on the area trained, area practised and duration trained.
Individual equipoise measures clinical uncertainty and arises when an individual clinician is completely undecided. Community equipoise is seen when there are differing views among a profession as a whole[14]. In this study, there were eight topics with community equipoise, of which four disagreed with the guidelines. These were topics based on both low and moderate levels of evidence.
Community equipoise was present for the initial treatment of symptomatic hemorrhoids, and disagreement existed with national guidelines for grade II internal hemorrhoids and acutely thrombosed external hemorrhoid. The American Society of Colon and Rectal Surgeons (ASCRS) practice parameters[7], Royal College of Surgeons commissioning guide[8], American College of Gastroenterology (ACG) clinical guideline[9] and Italian Society of Colorectal Surgery (SICCR) consensus statement[10] all recommend dietary modification (adequate fluid and fibre intake) as the initial treatment for symptomatic internal hemorrhoids, with more aggressive office-based or operative treatment for advanced hemorrhoidal disease (grades III to IV)[6,7]. In this study, there was consensus and agreement with the latter, but community equipoise for the management of low-grade hemorrhoidal disease. In particular, especially non-European trained surgeons, would choose RBL as the initial management of grade II hemorrhoids. A finding consistent with a Netherland based study, where 59% of respondents would also choose RBL[11]. While this may reflect a decision by colorectal surgeons once a patient has already tried dietary modification, it is still advocated as the initial non-operative treatment in clinical practice guidelines for the treatment of symptomatic hemorrhoid disease[7-10].
The ASCRS practice parameters[7], ACG clinical guideline[9] and SICCR consensus statement[10] all recommend office-based procedures when medical treatment fails to treat grade I–III hemorrhoid disease. RBL is reportedly the most widely performed of these therapies[15], and this is also reflected in Australasian practice. The most frequent exclusion criteria for this technique includes diabetes mellitus and coagulation disorders[10].
However, this study found community equipoise and disagreement with national guidelines for the management of grade III internal hemorrhoids in patients with such co-morbidities-known history of diabetes mellitus or a coagulation disorder (haemophilia A). RBL (61%) and surgical hemorrhoidectomy (30%) were the two most popular techniques for each of these scenarios respectively. Although septic complications of RBL are rare, they can be fatal[16]. There have been reported cases of pyogenic liver abscesses[16,17] and Fournier’s gangrene following RBL in patients known to have diabetes[18]. Sclerotherapy is an alternative and safer option in those with coagulation disorders who are at increased risk of post-procedure bleeding with RBL.
Decision-making in the management of hemorrhoids should consider patient preferences, including a prompt return to work and less pain post-operatively. This study found surgeons are more inclined to perform DGH or SH when a patient expressed these preferences. These two procedures were introduced to reduce post-hemorrhoidectomy pain, but with the caveat of higher recurrence rates than CEH[3-5]. CEH remains the gold standard for advanced hemorrhoids despite its association with greater postoperative pain and longer healing times than other procedures[5].
LigaSure hemorrhoidectomy is a frequently performed surgical procedure and with significantly less immediate postoperative pain than CEH[19]. This survey found more surgeons would use this technique than CEH alone to manage grade IV internal hemorrhoids for a patient requesting minimal post-operative pain (38% vs 6% respectively). However, the clinical practice guidelines advocating LigaSure hemorrhoidectomy are sparse[7-10]. This is despite the literature reporting LigaSure technique to be associated with less post-operative pain up to day 7 and significantly earlier return to work (4 studies, 451 patients, 4.88 d, CI 2.18 to 7.59)[19]. Although updated guidance from the ASCRS practice parameters now highlight bipolar techniques cause less postoperative pain when compared with closed hemorrhoidectomy[20].
There is a guideline consensus, albeit based on low quality evidence[7,10], that most patients presenting with thrombosed external hemorrhoids will benefit from surgical excision within 72 h of the onset of symptoms[7,9,12]. This survey found the majority of surgeons would rather manage these conservatively (88%). The guidelines acknowledge conservative management with eventual resolution of symptoms, but with longer resolution time, higher rates of recurrence and longer remission intervals[7,8,11]. This is certainly an area that could benefit from further research.
This study is limited by a suboptimal response rate (40%), although it has a much greater response rate than a Netherland based study, which had a 16% (100 of 619 contacts) returning a completed survey[11]. The suboptimal response rate may partly be due to the length of the scenarios which were necessary to explore the topic. We also do not have data from the non-respondents and whether their responses differed markedly from respondents. Only subspecialty colorectal surgeons were invited to participate in this survey in an effort to maximise the response rate. This limits the generalisability of the results when also considering the many other general surgeons who also treat hemorrhoids. Finally, this study has assessed colorectal surgeon consensus with international hemorrhoid clinical practice guidelines, since in the absence of Australian and New Zealand guidelines, surgeons practising in these two relatively small populations commonly refer to the latest guidelines in the English literature, particularly British and American influences.
In conclusion, this survey has identified areas of colorectal surgeon consensus with hemorrhoid clinical practice guidelines, but with many more areas of community equipoise. It is these areas of uncertainty and disagreement which would benefit from the prioritization of high-quality research, as they reflect guidelines based on both low and moderate levels of evidence.
Hemorrhoidal disease is the most common anorectal disorder. Hemorrhoids can be classified as external or internal, according to their relation to the dentate line. Generally, low-grade internal hemorrhoids are effectively treated conservatively, by non-operative measures, while high-grade internal hemorrhoids warrant procedural intervention.
This study is in addition to highlighting areas of equipoise that will benefit from future research.
In this study, the authors aimed to determine the application of clinical practice guidelines for the current management of hemorrhoids and colorectal surgeon consensus in Australia and New Zealand.
By using 17 guideline-based hypothetical clinical scenarios, an online survey was distributed to 206 colorectal surgeons in Australia and New Zealand.
Eight-two respondents to 17 guideline-based scenarios, nine reached consensus, of which only 1 disagreed with the guidelines. It was based on low quality evidence for the management of acutely thrombosed external hemorrhoids. There were 8 scenarios which showed community equipoise. These topics were based on low and moderate levels of evidence. And they included the initial management of grade I internal hemorrhoids, grade III internal hemorrhoids when initial management had failed and the patient had recognised risks factors for septic complications. Finally, the decision-making when considering patient preferences, including a prompt return to work, or minimal post-operative pain.
There are many areas of community equipoise which would benefit from further research.
| 1. | Riss S, Weiser FA, Schwameis K, Riss T, Mittlböck M, Steiner G, Stift A. The prevalence of hemorrhoids in adults. Int J Colorectal Dis. 2012;27:215-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 258] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 2. | Acheson AG, Scholefield JH. Management of haemorrhoids. BMJ. 2008;336:380-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 71] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Lohsiriwat V. Treatment of hemorrhoids: A coloproctologist's view. World J Gastroenterol. 2015;21:9245-9252. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 220] [Cited by in RCA: 150] [Article Influence: 13.6] [Reference Citation Analysis (18)] |
| 4. | Goligher JC. Advances in proctology. Practitioner. 1964;193:526-532. [PubMed] |
| 5. | Cerato MM, Cerato NL, Passos P, Treigue A, Damin DC. Surgical treatment of hemorrhoids: a critical appraisal of the current options. Arq Bras Cir Dig. 2014;27:66-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Buntzen S, Christensen P, Khalid A, Ljungmann K, Lindholt J, Lundby L, Walker LR, Raahave D, Qvist N; Danish Surgical Society. Diagnosis and treatment of haemorrhoids. Dan Med J. 2013;60:B4754. [PubMed] |
| 7. | Rivadeneira DE, Steele SR, Ternent C, Chalasani S, Buie WD, Rafferty JL; Standards Practice Task Force of The American Society of Colon and Rectal Surgeons. Practice parameters for the management of hemorrhoids (revised 2010). Dis Colon Rectum. 2011;54:1059-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 8. | The Royal College of Surgeons of England. Rectal Bleeding-Commissioning Guide. Library and Publications, London: RCS Pub 2013; . |
| 9. | Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109:1141-57; (Quiz) 1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 191] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 10. | Trompetto M, Clerico G, Cocorullo GF, Giordano P, Marino F, Martellucci J, Milito G, Mistrangelo M, Ratto C. Evaluation and management of hemorrhoids: Italian society of colorectal surgery (SICCR) consensus statement. Tech Coloproctol. 2015;19:567-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | van Tol RR, Bruijnen MPA, Melenhorst J, van Kuijk SMJ, Stassen LPS, Breukink SO. A national evaluation of the management practices of hemorrhoidal disease in the Netherlands. Int J Colorectal Dis. 2018;33:577-588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38562] [Cited by in RCA: 40192] [Article Influence: 2364.2] [Reference Citation Analysis (0)] |
| 13. | Young J, Harrison J, White G, May J, Solomon M. Developing measures of surgeons' equipoise to assess the feasibility of randomized controlled trials in vascular surgery. Surgery. 2004;136:1070-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Johnson N, Lilford RJ, Brazier W. At what level of collective equipoise does a clinical trial become ethical? J Med Ethics. 1991;17:30-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 92] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Brown SR. Haemorrhoids: an update on management. Ther Adv Chronic Dis. 2017;8:141-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Chau NG, Bhatia S, Raman M. Pylephlebitis and pyogenic liver abscesses: a complication of hemorrhoidal banding. Can J Gastroenterol. 2007;21:601-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Parker R, Gul R, Bucknall V, Bowley D, Karandikar S. Double jeopardy: pyogenic liver abscess and massive secondary rectal haemorrhage after rubber band ligation of haemorrhoids. Colorectal Dis. 2011;13:e184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Subramaniam D, Hureibi K, Zia K, Uheba M. The development of Fournier's gangrene following rubber band ligation of haemorrhoids. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Nienhuijs S, de Hingh I. Conventional versus LigaSure hemorrhoidectomy for patients with symptomatic Hemorrhoids. Cochrane Database Syst Rev. 2009;CD006761. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Davis BR, Lee-Kong SA, Migaly J, Feingold DL, Steele SR. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Management of Hemorrhoids. Dis Colon Rectum. 2018;61:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 179] [Article Influence: 22.4] [Reference Citation Analysis (2)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bordonaro M, Ji G S-Editor: Zhang L L-Editor: A E-Editor: Wu YXJ