Published online Oct 6, 2019. doi: 10.12998/wjcc.v7.i19.3111
Peer-review started: July 17, 2019
First decision: August 2, 2019
Revised: August 12, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: October 6, 2019
Processing time: 79 Days and 22.9 Hours
Primary hypoparathyroidism (HPT) is rarely seen in the clinic, and it can be combined with rhabdomyolysis. There are few reports about this phenomenon. Therefore, it is significant to explore the etiology that is conducive to early diagnosis, timely treatment, and preventing the recurrence.
A 63-year-old man was admitted to our hospital with a severe upper respiratory tract infection and progressing decreased myodynamia of the lower limbs. Blood tests showed creatine kinase > 32000 U/L, creatinine 207.8 µmol/L, calcium 1.28 mmol/L, myoglobin 558.7 ng/mL, and parathyroid hormone 0 pg/mL. He was diagnosed with primary HPT with rhabdomyolysis, and severe upper respiratory tract infection was considered to be the initial trigger. He responded well to supplementation of intravenous calcium gluconate and oral calcium as well as bedside hemodialysis, fluid hydration, infection control, protecting the liver, etc. Creatine kinase, myoglobin, and serum calcium returned to normal, and muscle strength improved significantly. Symptoms improved after symptomatic treatment.
Severe infection should be prevented, which is the key cause of rhabdomyolysis in patients with HPT.
Core tip: We described progressively decreased myodynamia and elevated muscle enzymes in a man with primary hypoparathyroidism. He was eventually diagnosed with rhabdomyolysis and acute kidney injury based on primary hypoparathyroidism. After bedside dialysis, antibiotic treatment, supplementation with blood calcium, and other symptomatic treatments, muscle strength recovered. Regular monitoring of blood calcium and prevention of infection are necessary to prevent recurrence.
- Citation: Ding LN, Wang Y, Tian J, Ye LF, Chen S, Wu SM, Shang WB. Primary hypoparathyroidism accompanied by rhabdomyolysis induced by infection: A case report. World J Clin Cases 2019; 7(19): 3111-3119
- URL: https://www.wjgnet.com/2307-8960/full/v7/i19/3111.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i19.3111
Hypothyroidism (hypoparathyroidism, HPT) is a rare endocrine disease induced by a variety of causes of low parathyroid hormone and reduced blood calcium. According to statistics, the incidence of postoperative and nonsurgical HPT is 23 and 17 per 100000, respectively[1]. Neuromuscular excitation is the main symptom, and its complications can involve multiple organs that have important effects on the brain, cognition, muscles, heart, and kidneys[2,3]. Myopathy is a rare manifestation of HPT and may be associated with elevated muscle enzymes caused by hypocalcemia in HPT patients[4]. A small number of patients may have rhabdomyolysis under certain circumstances, and there have been few previous reports of primary HPT with rhabdomyolysis; the first appeared in 1983[5], and in the last thirty years, it has been rarely reported. It is conducive to early diagnosis, timely treatment, and prevention of recurrence to analyze the causes and pathogenesis in patients with HPT. Here, we report the data of a patient with primary HPT and rhabdomyolysis who was admitted to the endocrinology ward in 2019. His symptoms improved significantly when he was discharged from the hospital after timely and effective treatment.
A 63-year-old man who had suffered from cough and asthma with fatigue in both lower limbs for 1 wk was admitted to our hospital.
He had nasal congestion, runny nose accompanied by cough and spit, wheezing, and weakness of both lower limbs for a week before he was admitted to the hospital. The symptoms continued to progress even with the guidance of community doctors and treatment with oral cephalosporin. Subsequently, he was sent to the emergency department for loss of the ability to stand and walk.
The patient had suffered from chronic obstructive pulmonary disease for 2 years. There was no history of coronary heart disease, diabetes, chronic kidney disease, adrenal adenoma, adrenal hyperplasia, or autoimmune disease and no use of glycyrrhizic acid or statins.
He was misdiagnosed with and treated for epilepsy because of physical con-vulsions in his teenage years. Then, he was diagnosed with primary HPT 40 years ago in another hospital because of low parathyroid hormone but had no thyroidectomy, parathyroidectomy, or radiation exposure. After diagnosis, he took calcitriol 75 µg/d and calcium carbonate D3 375 µg/d regularly. He was hospitalized in our hospital 2 years ago because of sudden syncope and fatigue. Elevated creatine kinase, hypocalcemia, acute upper respiratory tract infection, and an abnormal increase in creatinine were detected, and symptoms improved after symptomatic treatment.
The lungs showed severe wheezing, and a high-pitched wet sound could be heard in the lower right lung. The upper limb muscle strength was grade 4, while the lower limb strength was grade 1. The muscle tension was normal, but the lower limbs had slight edema on physical examination.
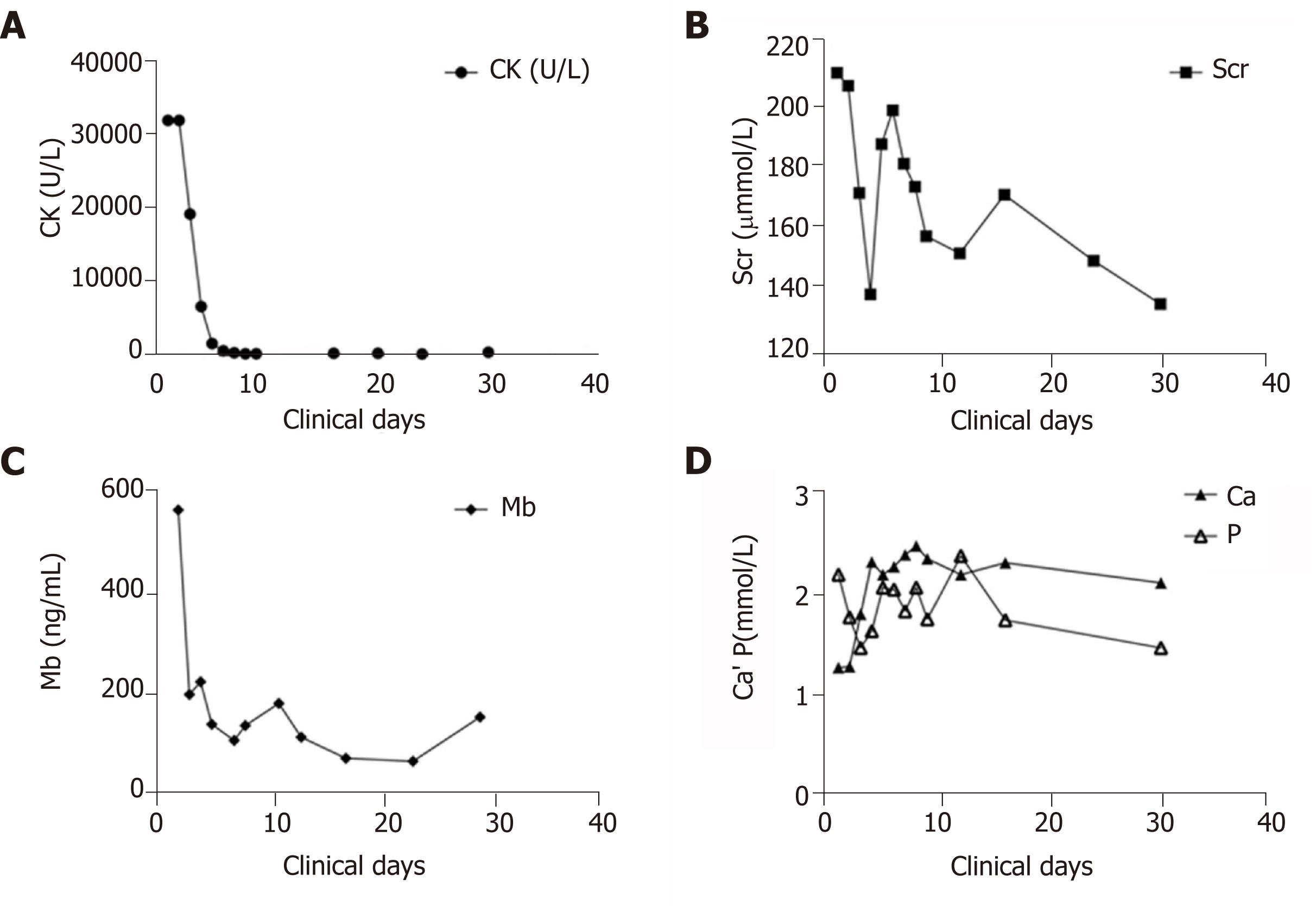
His blood test suggested a severe infection, severe hypocalcemia, hypokalemia, and elevated levels of anhydrase and creatinine. Myocardial zymography showed increased creatine kinase (> 32000 U/L), and the myoglobin level was abnormally elevated (558.7 ng/mL), with a B-type natriuretic peptide level of 200 pg/mL and a cardiac troponin I level of 0.2 ng/mL (Table 1). The changes in the pathological laboratory index during the disease course are presented in Figure 1.
| Admission | Discharge | Follow up | Normal range | |
| Leucocytes, /L | 18.01 × 109 | 9.32 × 109 | 6.35 × 109 | 4-10 × 109 |
| Neutrophil, % | 90.6 | 72.9 | 70.2 | 50-70 |
| Hemoglobin, g/L | 119 | 107 | 103 | 120-160 |
| AST, U/L | 518 | 33 | - | < 38 |
| ALT, U/L | 88 | 41 | - | < 42 |
| CK, U/L | > 32000 | 354 | 96 | 24-195 |
| CK-MB, U/L | 420 | 13 | 10 | < 25 |
| LDH, U/L | 4864 | 226 | 234 | 135-225 |
| Urea, mmol/L | 7.2 | 11.31 | 10.62 | 1.7-8.3 |
| Creatinine, µmol/L | 212.1 | 134.5 | 137.3 | 44-110 |
| Potassium, mmol/L | 3.19 | 4.07 | 3.99 | 3.5-5.1 |
| Calcium, mmol/L | 1.27 | 2.13 | 2.44 | 2.1-2.95 |
| Uric acid, µmol/L | 688 | 631.8 | 579.3 | 200-420 |
| Phosphorus, mmol/L | 2.21 | 1.47 | - | 0.87-1.45 |
| Myoglobin, ng/mL | 558.7 | 141.5 | 58.6 | 17.4-105.7 |
| 25(OH)D, ng/L | 25.49 | - | 30.38 | - |
| PTH, pg/mL | 0 | 0 | 0 | 12.0-88.0 |
| CTn I, ng/mL | 0.2 | 0.04 | - | < 0.04 |
The cranial computed tomography showed multiple symmetrical patchy calcifications in the bilateral white matter, basal ganglia, thalamic area, and cerebellar hemisphere (Figure 2). The chest computed tomography demonstrated that there was no obvious lesion.
The blood gas analysis results of the patient suggested current type 1 respiratory failure, and it was necessary to increase oxygen inhalation. It was also recommended that methylprednisolone be used to relieve spasm and asthma.
Acute kidney injury is considered to be secondary to rhabdomyolysis, and the treatment should be based on stable electrolytes; if necessary, bedside continuous renal replacement therapy can be taken. Cardiac injury is a secondary injury and may be associated with severe hypocalcemia and elevated muscle enzymes. We checked the myocardial infarction index again after symptomatic treatment.
Primary HPT; rhabdomyolysis; hypocalcemia; acute kidney injury; chronic obstructive pulmonary disease with acute respiratory tract infection.
Based on these blood test results, we suspected multiorgan failure due to infectious diseases. We first tried intravenous methylprednisolone (40 mg) for 3 days to relieve spasm and asthma. Once the asthma was eased, we stopped using hormones, and we empirically used second-generation cephalosporin antibiotics combined with moxifloxacin to control infection. After the clear diagnosis by perfecting the test for myoglobin, bedside dialysis was performed periodically and continued for 3 days because of the continuous oliguria, despite rehydration, until the renal function improved, and the myoglobin and creatine kinase decreased. The man responded well to supplementation with intravenous calcium gluconate (2 g/d), calcium carbonate D3 (250 IU/d), and calcitriol (5 μg/d). Simultaneous rehydration, stable electrolytes, antibacterial therapy, and liver protection were equally important in the process.
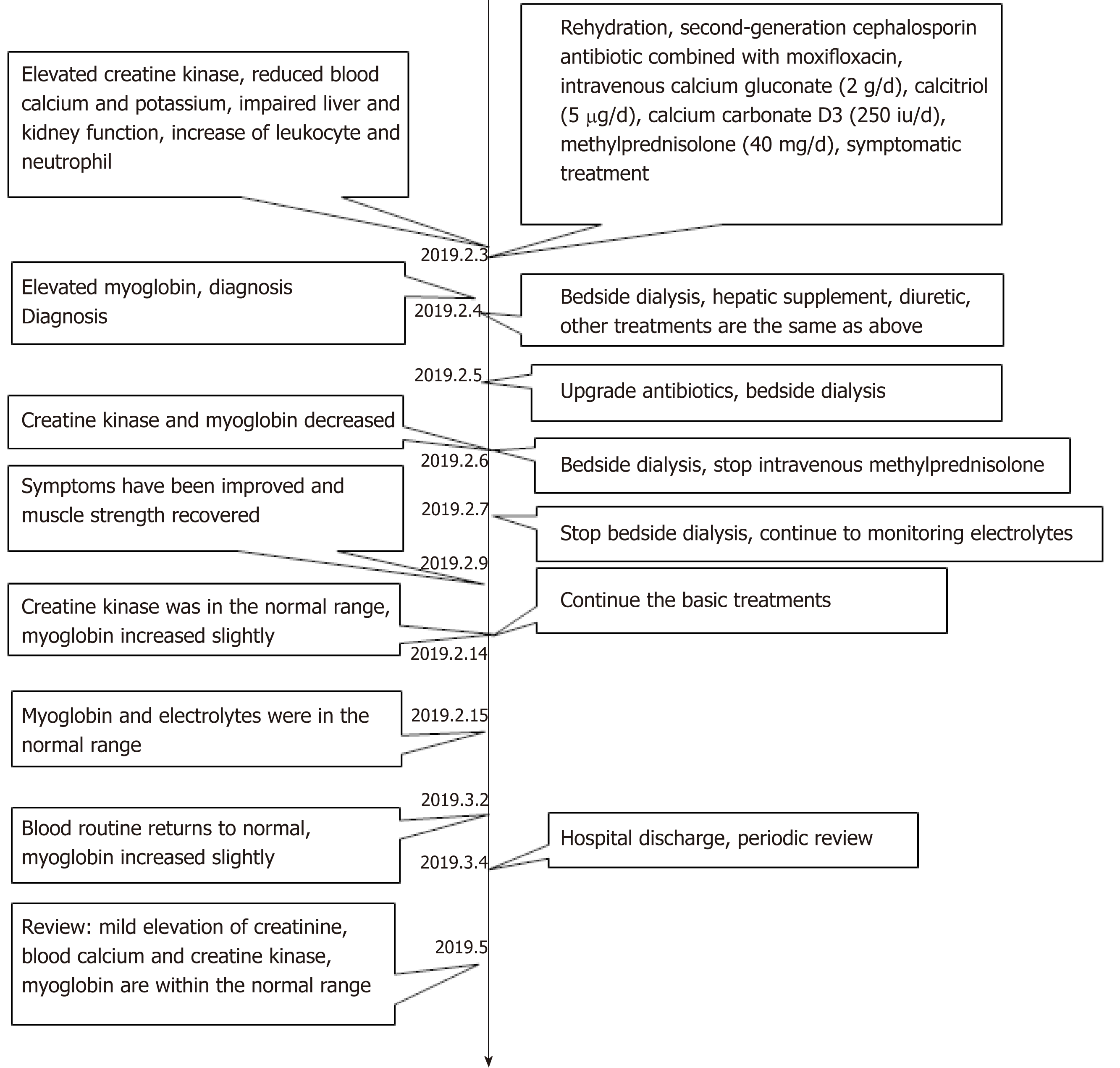
The patient’s symptoms improved by more than half, while the creatine kinase level decreased to normal, and muscle strength was restored to grade 4 12 days later. He was transferred to the rehabilitation center for further rehabilitation because of his remaining muscle strength. He was discharged with treatment with oral calcium (250 IU/d) and calcitriol (5 μg/d) and was advised to return to the endocrinology outpatient clinic regularly for calcium reexamination. No abnormalities occurred during 1 mo of follow-up after discharge. The man felt good in the most recent review, and the blood test suggested elevated creatinine and uric acid, while the blood calcium and myoglobin were within the normal range. It should be noted that the amount of calcium should be controlled to prevent hypercalcemia and rehospitali-zation because the young man who was treated by Sumnu et al[6] was hospitalized again during follow-up for hypercalcemia. A timeline was organized from information of the case report that was presented in the end (Figure 3)
We have described a man with primary HPT accompanied by muscle weakness and increased muscle enzymes who was finally diagnosed with rhabdomyolysis. Our case indicates that patients with severe infections are more likely to suffer from rhabdomyolysis if they have HPT, and the main reason may be related to the extremely elevated muscle enzymes caused by severe hypocalcemia. Severe respiratory infections and acute kidney injury, which are further exacerbated by the reduction of calcium, will contribute to the lower blood calcium to worsen the condition.
Here, we listed the cases of HPT with rhabdomyolysis that have been reported so far, whose clinical data were detailed (Table 2). In 1983, Liu et al[5] first reported the case of primary HPT with rhabdomyolysis without any cause, in which the blood calcium was found to be inversely proportional to myoglobin and lactate dehy-drogenase, and in 1993, it was reported that serum creatine kinase, lactate dehydrogenase, and blood calcium were inversely related[7]. Three cases[8-10] discussed the occurrence of primary HPT related to MTP deficiency caused by gene mutation, which were mainly considered to be mutation of the HADHB gene and HADHA gene. Sumnu et al[6] reported a case accompanied by acute kidney injury in a young male, whose main symptoms were pain in the leg muscles, nausea, and vomiting, and focused on the description of the cranial calcification. Overall, few of the published studies clarified the causes and possible mechanisms of the disease. In our table, patients who had no other medical history except primary HPT combined with rhabdomyolysis for different reasons at a relatively young age, the main symptoms were muscle weakness or tetany. However, the older male had a history of chronic obstructive pulmonary disease. For our patient, there were three characteristics during the disease: one is severe hypocalcemia, the second is severe respiratory tract infection, and the third is acute renal impairment. Here, we discuss the possible pathogenesis and the relationship among the three aspects.
| Ref. | Age/sex | Year | Main symptoms | CK | Calcium | Trigger | Treatment | Follow up |
| Liu et al[5] | 53/M | 1983 | Leg pain, swelling, erythema of extremity | 45000 | 1.175 | Cellulitis | Ergocalciferol (100000 U/d), gluconate calcium (20 g/d) | Normal |
| Akmal[7] | 45/F | 1993 | Tiredness, weakness,inappropriate, behavior | 26080 | 1.025 | None | Calcium gluconate and vitamin D2 | Normal |
| Hirata et al[13] | 30/M | 2001 | Tetany, hyporeflexia, fatigue | 3540 | 1.2 | None | Calcium and 1α-hydroxyvitamin D3 | Normal |
| Labarthe et al[10] | 4 m/M | 2006 | Muscular pains, areflexia | 10960 | 1.2 | Fasting | Alfacalcidol (20 μg/d) | Nuclear cataract |
| Naiki et al[8] | 2/F | 2014 | Tetany | 9577 | 1.48 | Infection | Intravenous fluids | Recurrence (3 yr old) |
| van Vliet et al[9] | 20/F | 2017 | Dyspnea, muscle weakness, vomiting | 193936 | 1.48 | Viral gastroenteritis | Intravenous hydration, calcium | Recurrence 14 wk later |
| Sumnu et al[6] | 26/M | 2015 | Pain and cramps in the legs, nausea, vomiting | 262000 | 0.925 | Tetany | Calcium and calcitriol, hydration | Hypercalcemia |
| Kutílek et al[19] | 16/M | 2018 | Convulsions, transient loss of consciousness | 1920 | < 1 | None | Calcium, cholecalciferol | Normal |
Rhabdomyolysis was firstly described in crush injuries, and it was thought to be associated with thermal injuries[11]. Other nontraumatic causes include electrolyte disorder, infection, and drugs (such as statins)[12] in later years. Direct muscle injury remains to be the most common cause of rhabdomyolysis. Our patient had no history of strenuous exercise or related drug intake. We believe that hypocalcemia and infection played a role in the incidence of the disease because there are studies showing that elevated muscle enzymes are associated with hypocalcemia[13] and infection[14]. Meanwhile, there is a direct relationship between hypocalcemia and primary HPT[15]. As hypocalcemia is the main feature of HPT[16]; we have reason to believe that patients with HPT may suffer from rhabdomyolysis easily.
Previously, it was thought that hypocalcemia was characterized by decreased muscle strength, but not all hypocalcemia patients have clinical signs; these signs depend on the degree of low calcium and the rate of calcium decrease. Chronic hypocalcemia manifests as cataract, anxiety, basal ganglia calcification, or extrapyramidal dyskinesia, while acute hypocalcemia is presented as paresthesia, muscle weakness, or even paralysis[17]. Both acute and chronic hypocalcemia are associated with elevated muscle enzymes[3], which have also been found in the case of postoperative HPT[18] and pseudohypoparathyroidism[19]. The specific mechanism of elevated muscle enzyme in patients is not clear; one of the speculative mechanisms is that muscle enzyme leaks from the myocytes due to the change in membrane permeability under hypocalcemia[20] or a slight change in blood calcium levels. The destruction of muscle cells also result in the leakage of myoglobin, creatine kinase, aldolase phosphate, lactate dehydrogenase, and aspartate transaminase[11], which can explain the dramatic elevation of aspartate transaminase in patients with rhabdomyolysis.
Muscle cell changes inevitably occur in patients with mild to moderate myocyte vacuolation and focal hyalinosis. Muscle cell atrophy, multifocal myofibrillar degeneration, and sarcolemmal cell proliferation were found in myocytes through muscle biopsy, and there were different degrees of immune complexation. The change is thought to be connected to the duration and extent of low calcium[4]. We concluded that the absence of regular monitoring of the concentration of calcium may result in patients suffering from long-term low calcium levels or a sharp decrease in calcium because of certain causes.
Hypocalcemia is the key to the elevated muscle enzymes, but the occurrence of rhabdomyolysis requires a trigger, which in this case was the respiratory tract infection. Serum calcium is strongly associated with pulmonary infection, and it is estimated that at least half of rhabdomyolysis cases occur in elderly people with acute respiratory infections, which may be related to elevated temperature and high levels of proinflammatory mediators (such as cytokines and chemokines) caused by infectious diseases[21]. Furthermore, studies suggest that patients with hypocalcemia are more likely to develop respiratory diseases[22], whereas patients with respiratory diseases would have lower serum calcium levels, especially in elderly patients[23].
Serum potassium seems to play an equally important role in regulating skeletal muscle. According to decades of literature, severe hypokalemia was a main trigger of rhabdomyolysis caused by primary hyperaldosteronism, excessive consumption of glycyrrhizic drugs, diuretics, renal tubular acidosis, vomiting, and diarrhea. Interestingly, the concentrations of potassium in reported cases were within 2 mmol/L; additionally, scholars held that those with potassium below 2 mmol/L are more prone to suffer from rhabdomyolysis and arrhythmia[24]. In our case, the patient’s potassium was 3.12 mmol/L, and there was no lower potassium observed during the course; hence, we presumed that hypokalemia is not the major trigger.
It is well recognized that the nephrotoxic effect of myoglobin results in kidney damage, which is common in rhabdomyolysis[25]. Studies have shown that hypocalcemia is more likely to occur in the presence of a large volume of muscle damage and phosphate retention in rhabdomyolysis. Acute kidney injury during rhabdomyolysis further aggravates phosphate deposition. Ultimately, the use of phosphate depletes ATP and then impairs active calcium transport in the muscle, which causes a decrease in blood calcium[26]. All of the above possibilities combine with the history of primary HPT to make the decreased blood calcium worsen. The patient’s primary HPT, hypocalcemia, acute kidney injury, and infection formed a vicious circle. Despite this effect, the critical condition and the progressing decreased myodynamia could be reversed after timely treatment. The main goal is to avoid acute kidney injury[27]; on the one hand, active rehydration[28] may prevent acute kidney injury and contribute to the clearance of myoglobin. Once this occurs, continuous renal replacement therapy is a good choice that may provide benefits for people with rhabdomyolysis by removing myoglobin and stabilizing the hemodynamic and metabolic status[29]. On the other hand, symptomatic treatment needs to continue during the whole process.
It is worth noting that in the early stage of treatment, the patient was treated with corticosteroids for asthma during our treatments. Although there was no significant effect on the increase in blood calcium in our case, the steroids inhibited intestinal calcium absorption and increased renal calcium excretion, leading to worsening of hypocalcemia[30] and worsening of symptoms. Considering this effect, early measurement of serum calcium is important. Blood calcium levels are targeted at or slightly below the lower limit of the normal range, to the extent possible, while being careful to avoid hypercalcemia, which may cause the sudden deterioration of the patient’s condition or even death during recovery[31].
Our case indicates that rhabdomyolysis occurs easily in patients with primary HPT under certain conditions (such as infections). Although the mortality rate is high, lethal outcomes can be avoided by active treatment. Considering the important role of serum calcium, long-term regular use of drugs to supplement calcium, detection of blood calcium concentration regularly, and avoiding triggers (such as infection) are necessary, which is important to maintain muscle enzymes within the normal range to prevent the recurrence of rhabdomyolysis.
| 1. | Vadiveloo T, Donnan PT, Leese GP. A Population-Based Study of the Epidemiology of Chronic Hypoparathyroidism. J Bone Miner Res. 2018;33:478-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 2. | Marcucci G, Cianferotti L, Brandi ML. Clinical presentation and management of hypoparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32:927-939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Tecilazich F, Formenti AM, Frara S, Giubbini R, Giustina A. Treatment of hypoparathyroidism. Best Pract Res Clin Endocrinol Metab. 2018;32:955-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Dai CL, Sun ZJ, Zhang X, Qiu MC. Elevated muscle enzymes and muscle biopsy in idiopathic hypoparathyroidism patients. J Endocrinol Invest. 2012;35:286-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Liu ET, Bristow MR, Stone MJ, Willerson JT. Serum myoglobin, ionized calcium, and parathyroid function during rhabdomyolysis. Arch Intern Med. 1983;143:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 6. | Sumnu A, Aydin Z, Gursu M, Uzun S, Karadag S, Cebeci E, Ozturk S, Kazancioglu R. A Case of Primary Hypoparathyroidism Presenting with Acute Kidney Injury Secondary to Rhabdomyolysis. Case Rep Nephrol. 2016;2016:3240131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Akmal M. Rhabdomyolysis in a patient with hypocalcemia due to hypoparathyroidism. Am J Nephrol. 1993;13:61-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Naiki M, Ochi N, Kato YS, Purevsuren J, Yamada K, Kimura R, Fukushi D, Hara S, Yamada Y, Kumagai T, Yamaguchi S, Wakamatsu N. Mutations in HADHB, which encodes the β-subunit of mitochondrial trifunctional protein, cause infantile onset hypoparathyroidism and peripheral polyneuropathy. Am J Med Genet A. 2014;164A:1180-1187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | van Vliet P, Berden AE, van Schie MKM, Bakker JA, Heringhaus C, de Coo IFM, Langeveld M, Schroijen MA, Arbous MS. Peripheral Neuropathy, Episodic Rhabdomyolysis, and Hypoparathyroidism in a Patient with Mitochondrial Trifunctional Protein Deficiency. JIMD Rep. 2018;38:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Labarthe F, Benoist JF, Brivet M, Vianey-Saban C, Despert F, de Baulny HO. Partial hypoparathyroidism associated with mitochondrial trifunctional protein deficiency. Eur J Pediatr. 2006;165:389-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Coban YK. Rhabdomyolysis, compartment syndrome and thermal injury. World J Crit Care Med. 2014;3:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (1)] |
| 12. | Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis -- an overview for clinicians. Crit Care. 2005;9:158-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 486] [Cited by in RCA: 582] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 13. | Hirata D, Nagashima T, Saito S, Okazaki H, Kano S, Minota S. Elevated muscle enzymes in a patient with severe hypocalcemia mimicking polymyositis. Mod Rheumatol. 2002;12:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Tseytlin D, Maynard S. Severe rhabdomyolysis secondary to adenovirus infection: case report and literature review. Clin Nephrol. 2016;85:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Cusano NE, Bilezikian JP. Update on hypoparathyroidism. Curr Opin Rheumatol. 2019;31:381-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Siraj N, Hakami Y, Khan A. Medical Hypoparathyroidism. Endocrinol Metab Clin North Am. 2018;47:797-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Policepatil SM, Caplan RH, Dolan M. Hypocalcemic myopathy secondary to hypoparathyroidism. WMJ. 2012;111:173-175. [PubMed] |
| 18. | Cheema UY, Vogler CN, Thompson J, Sattovia SL, Vallurupalli S. Protracted hypocalcemia following post-thyroidectomy lumbar rhabdomyolysis secondary to evolving hypoparathyroidism. Ear Nose Throat J. 2015;94:113-116. [PubMed] |
| 19. | Kutílek Š, Plášilová I, Hasenöhrlová K, Černá H, Hanulíková K. Severe Hypocalcemia and Extreme Elevation of Serum Creatinkinase in a 16-Year Old Boy with Pseudohypoparathyroidism Type Ib. Acta Medica (Hradec Kralove). 2018;61:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Barber J, Butler RC, Davie MW, Sewry CA. Hypoparathyroidism presenting as myopathy with raised creatine kinase. Rheumatology (Oxford). 2001;40:1417-1418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Hamel Y, Mamoune A, Mauvais FX, Habarou F, Lallement L, Romero NB, Ottolenghi C, de Lonlay P. Acute rhabdomyolysis and inflammation. J Inherit Metab Dis. 2015;38:621-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 22. | Li X, Bie Z, Zhang Z, Li Y, Hu X, Liu W, Zhang S, Cheng G, Ai B. Clinical analysis of 64 patients with lung-cancer-associated hypercalcemia. J Cancer Res Ther. 2015;11 Suppl:C275-C279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Qin J, Deng X, Wei A, Qin Y, Wu Y, Liao L, Lin F. Correlation between hypocalcemia and acute exacerbation of chronic obstructive pulmonary disease in the elderly. Postgrad Med. 2019;131:319-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | de Wolff JF. Rhabdomyolysis. Br J Hosp Med (Lond). 2012;73:C30-C32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 25. | Zorova LD, Pevzner IB, Chupyrkina AA, Zorov SD, Silachev DN, Plotnikov EY, Zorov DB. The role of myoglobin degradation in nephrotoxicity after rhabdomyolysis. Chem Biol Interact. 2016;256:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Higaki M, Tanemoto M, Shiraishi T, Taniguchi K, Fujigaki Y, Uchida S. Acute Kidney Injury Facilitates Hypocalcemia by Exacerbating the Hyperphosphatemic Effect of Muscle Damage in Rhabdomyolysis. Nephron. 2015;131:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Torres PA, Helmstetter JA, Kaye AM, Kaye AD. Rhabdomyolysis: pathogenesis, diagnosis, and treatment. Ochsner J. 2015;15:58-69. [PubMed] |
| 28. | Michelsen J, Cordtz J, Liboriussen L, Behzadi MT, Ibsen M, Damholt MB, Møller MH, Wiis J. Prevention of rhabdomyolysis-induced acute kidney injury - A DASAIM/DSIT clinical practice guideline. Acta Anaesthesiol Scand. 2019;63:576-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 29. | Zeng X, Zhang L, Wu T, Fu P. Continuous renal replacement therapy (CRRT) for rhabdomyolysis. Cochrane Database Syst Rev. 2014;CD008566. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Compston J. Glucocorticoid-induced osteoporosis: an update. Endocrine. 2018;61:7-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 216] [Cited by in RCA: 309] [Article Influence: 38.6] [Reference Citation Analysis (11)] |
| 31. | Graziani G, Calvetta A, Cucchiari D, Valaperta S, Montanelli A. Life-threatening hypercalcemia in patients with rhabdomyolysis-induced oliguric acute renal failure. J Nephrol. 2011;24:128-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coban YK S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Xing YX