Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2587
Peer-review started: April 12, 2019
First decision: May 31, 2019
Revised: June 25, 2019
Accepted: July 20, 2019
Article in press: July 20, 2019
Published online: September 6, 2019
Processing time: 148 Days and 6.4 Hours
The history of allogenic tooth transplantation can be traced back to the 16th century. Although there have been many successful cases, much needs to be better understood and researched prior to the technique being translated to everyday clinical practice.
In the present report, we describe a case of allogenic tooth transplantation between a mother and her daughter. The first left maxillary molar of the mother was diagnosed with residual root resorption and needed to be extracted. The 3rd molar of the daughter was used as a donor tooth. Prior to transplantation, a 3D printing system was introduced to fabricate an individualized reamer drill specifically designed utilizing the donor’s tooth as a template. The specific design of our 3D printed bur allowed for the recipient site to better match the donor tooth. With the ability to 3D print in layers, even the protuberance of the root can be matched and 3D printed, thereby minimizing unnecessary bone loss.
Our study is a pioneering case combining 3D printing with allogenic tooth transplantation, which could be able to minimize unnecessary bone loss and improve the implant stability. This article aims to enhance our understanding of allogenic tooth transplantation and 3D printing, and may potentially lead to tooth transplantation being utilized more frequently - especially since transplantations are so commonly utilized in many other fields of medicine with high success rates.
Core tip: The history of allogenic tooth transplantation can be traced back to the 16th century. Although there have been many successful cases, much needs to be better understood and researched prior to the technique being translated to everyday clinical practice. Our study is a pioneering case combining 3D printing with allogenic tooth transplantation, which could be able to minimize unnecessary bone loss and improve the implant stability. What’s more, a review of the previous relevant research and the potential future avenues of research related to the novel introduction of 3D printing for tooth transplantation cases was performed.
- Citation: Xu HD, Miron RJ, Zhang XX, Zhang YF. Allogenic tooth transplantation using 3D printing: A case report and review of the literature. World J Clin Cases 2019; 7(17): 2587-2596
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2587.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2587
The history of allogenic tooth transplantation can be traced back to the 16th century, particularly during the last decades of the 20th century. While individual organs are often transplanted from one individual to the next, in the dental field, transplantation of teeth is much less frequently performed. Several innovations from basic and clinical translational research has improved patient matching tests and clinical techniques[1,2]. Allogenic tooth transplantation refers to tooth grafting between two individuals of the same species whereas autogenic tooth transplantation indicates tooth grafting from one site to another in the same individual[3]. Atkinson reported in the 1970s that an autograft can be orthotopic (when transplanted to the natural location) or heterotopic (when transplanted to a completely different site). Generally, allografts are rejected by immune cells, which may cause the most common histopathological symptoms including chronic inflammatory infiltration of the grafted tissue[4,5]. However, a few cases of allogenic tooth transplantation have been reported[6]. Little progress has been made owing to the high rate of potential immunological rejections and the increased use of titanium dental implants[7]. Nevertheless, allografts can still function normally and often symptomless for many years[8].
There are many successful cases of allo-transplantation. Ole Schwartz reported 73 allotransplanting cases which were carried out by three surgeons in humans from 1956 to 1980[8]. The mean functional (without symptoms) time of the grafted teeth was 6.8 years (maximum 28.5 years, which is also the maximum observation period)[4,6,9]. This study illustrates the potential long-term survival rates of allograft tooth transplants with rates influenced by a series of factors.
In previous cases, since differences in root shape and length exist, surgeons have had to reposition the donor tooth back to its original socket and remodel the recipient site with a round implant bur[10]. The remodeling of the recipient site adds additional time to the surgical procedure with the possibility of surgically removing more bone than needed, which could totally be improved by the utilization of 3D printing. Today, 3D printing has been used widely in many fields of organ engineering[11-17]. A typical 3D printing process involves data collection, model analysis, structure design, and final manufacture. Specifically, data initially can be collected by a variety of systems including computed tomography (CT), digital scanning, magnetic resonance imaging, and other image modality systems[18]. Computer-aided design (CAD) software was followed by a precisely conducted 3D printing process controlled by a computer-aided manufacturing printer. The advantages of 3D printing include accurate control of material distribution, fast speed, scalability, and cost-effectiveness, which render this technology highly suitable and relevant in many areas of medicine including dentistry[19,20]. One of the greatest advantages of 3D printing in tooth transplantation is that osteotomy drills can be customized to the three-dimensional geometry of the tooth root of the individual donor[21]. Such drills allow an optimal integration of transplanted tooth without unnecessary compression of tissues that may occur with standard burs, minimize unnecessary bone loss, and improve the implant stability[22,23]. Furthermore, allogenic tooth transplantation could be an alternative solution for financially compromised patients that by-pass the need for additional costs including an implant, abutment, and final crown. This case report is the first published case combining 3D printing technology for tooth transplantation, which aims to inspire future research endeavors into this largely unstudied field.
A 47-year-old Chinese patient presented to the dental clinic at Wuhan University with a missing 1st molar for 2 mo. Her daughter (the donor) was a 21-year-old dental student with an impacted wisdom tooth.
The first left maxillary molar of the patient had been extracted in a private dental clinic 2 mo prior to the tooth transplantation. The root canal treatment for the 1st molar has failed, and tooth extraction was conducted after the roots fractured. The donor recently extracted two right third molars 2 wk prior to the donation (upper and lower).
No other health conditions are reported.
The patient is allergic to penicillin.
The mother has hypertension.
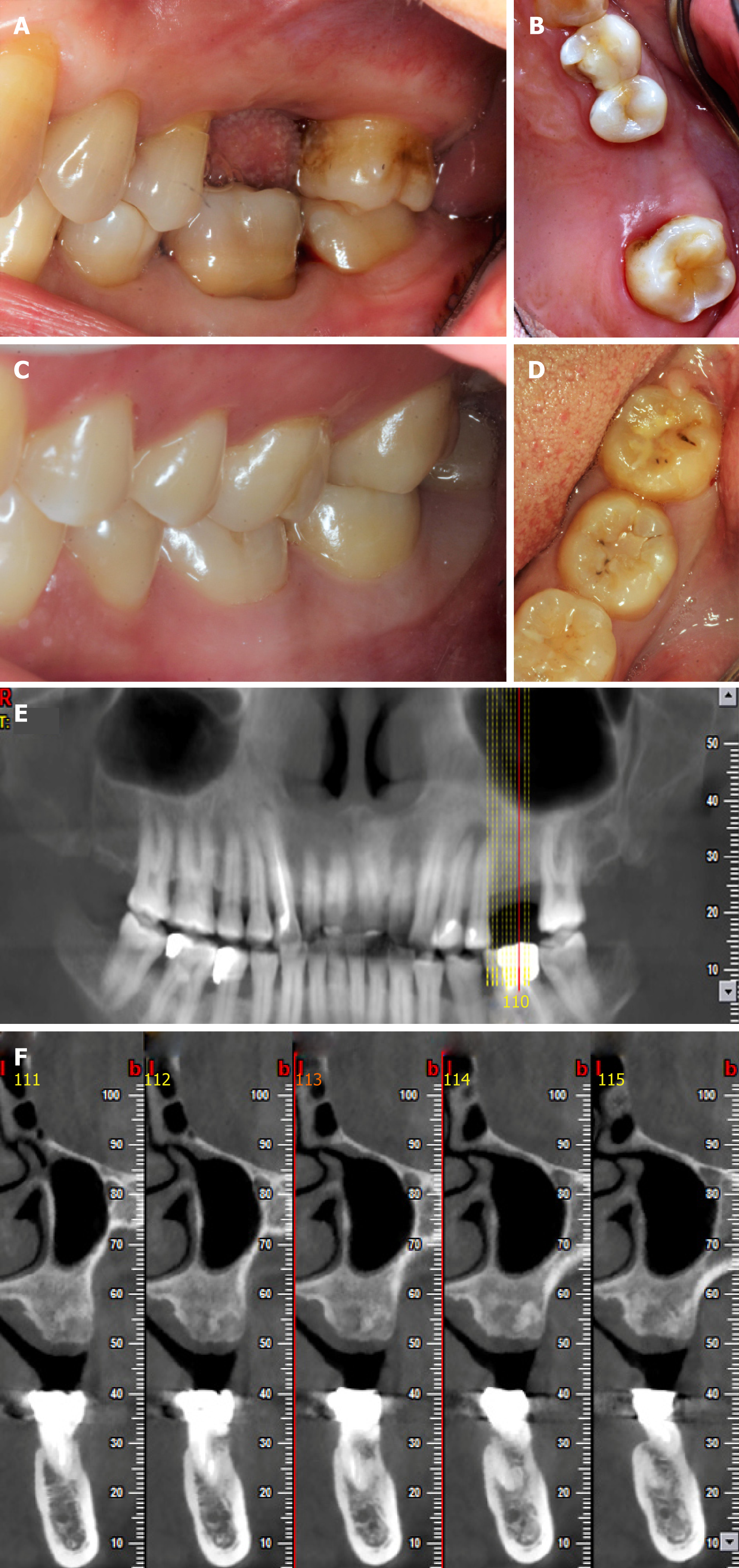
In the initial physical examination, the patient had a blood pressure of 128/84 mmHg with a pulse rate of 79 beats per minute (bpm). And the donor had a blood pressure of 92/62 mmHg with a pulse rate of 82 bpm. The extraction wound was well healed, and the anteroposterior gap of the defect was acceptable. The mandibular and maxillary distance had not been compromised, and the buccolingual width was about 7 mm. No obvious inclination of adjacent teeth was observed for the patient. The patient’s oral hygiene was acceptable, with little microbial plaque accumulation or associated trauma (Figure 1).
The patient has an O blood type. The donor presents with an A blood type. Routine blood count and coagulation profile for both the patient and donor were within normal limits.
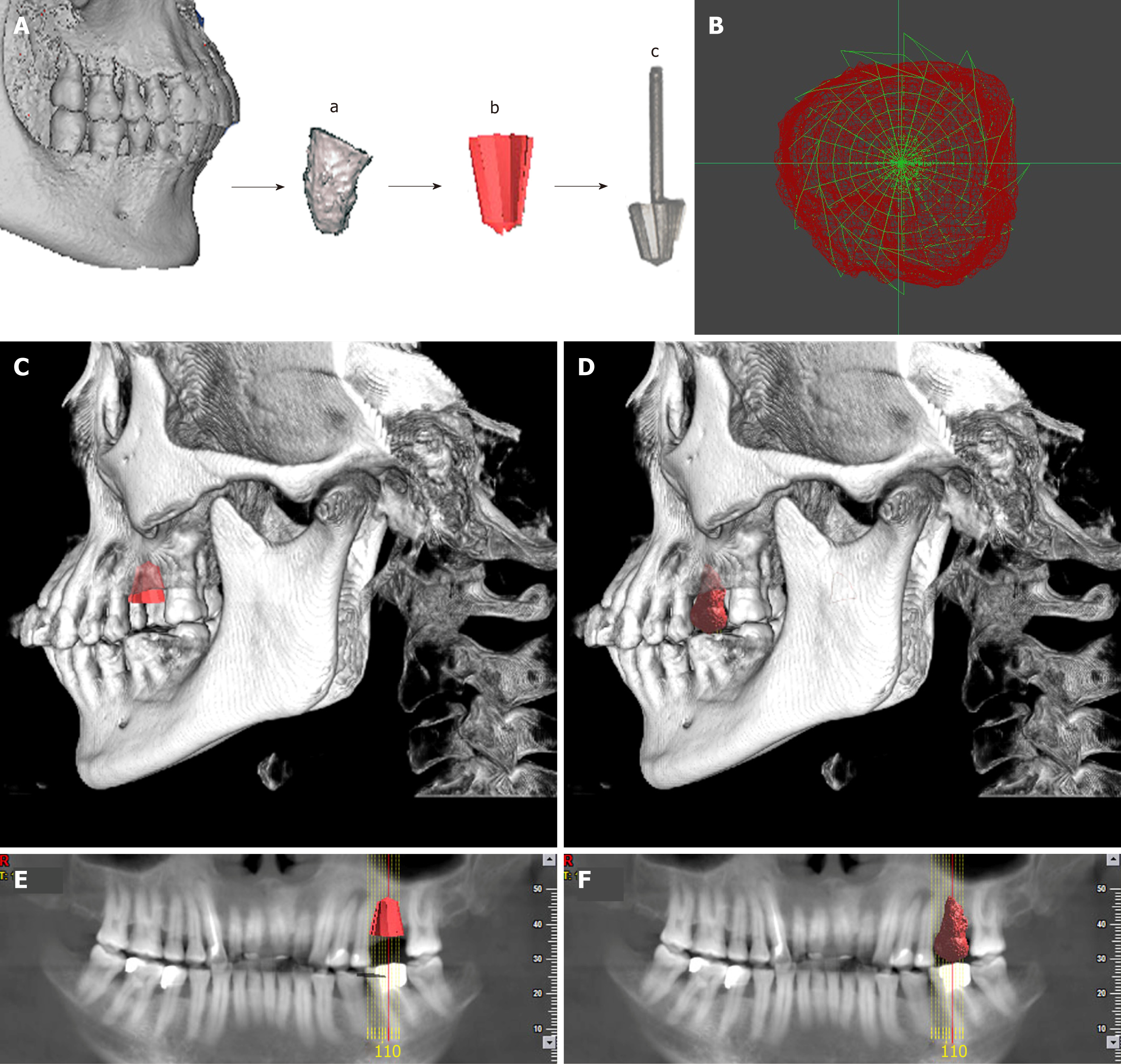
Cone beam computed tomography (CBCT) of the donor revealed a tapered root shape different in morphology from the recipient’s residual 1st maxillary molar root (3 roots), which eliminated the potential for an immediate transplantation. The lower 3rd mandibular molar (the donor tooth) was scanned, and the data of the morphology were collected and analyzed before an individualized implant drill was designed to match the contour of the donor tooth roots, with expectation that the shape of the recipient site could be identical to that of the original socket. A direct metal laser sintering 3D printing system was introduced to manufacture the drill (Figure 2).
Maxillary dentition defect.
The individual drill was produced by Wuhan Tianyu Intelligent Manufacturing Company using direct metal laser sintering as follows: (1) The 3d image of the donor’s tooth was extracted from the CBCT; (2) The data of the donor’s CBCT were imported into a STEP format CAD file using CAD software; (3) A CAD model was built using a measuring instrument to gather information regarding the shape and size of the tooth; (4) The shape of the drill was designed according to the donor’s tooth, and the taper and the base of the drill were in accordance with the tooth’s taper and the cervix, and then transferred into a CAD model; (5) The model was then sliced into discrete horizontal layers; and (6) A high-powered laser beam was focused onto a bed of powdered metal to fuse the model layer by layer. Each layer was printed followed by a subsequent layer of powder and printing to produce the next slice of the framework and fused with the first until all layers have been completely built. The laser was utilized to fuse the metal powder into metal solid particles and control their trajectory accurately.
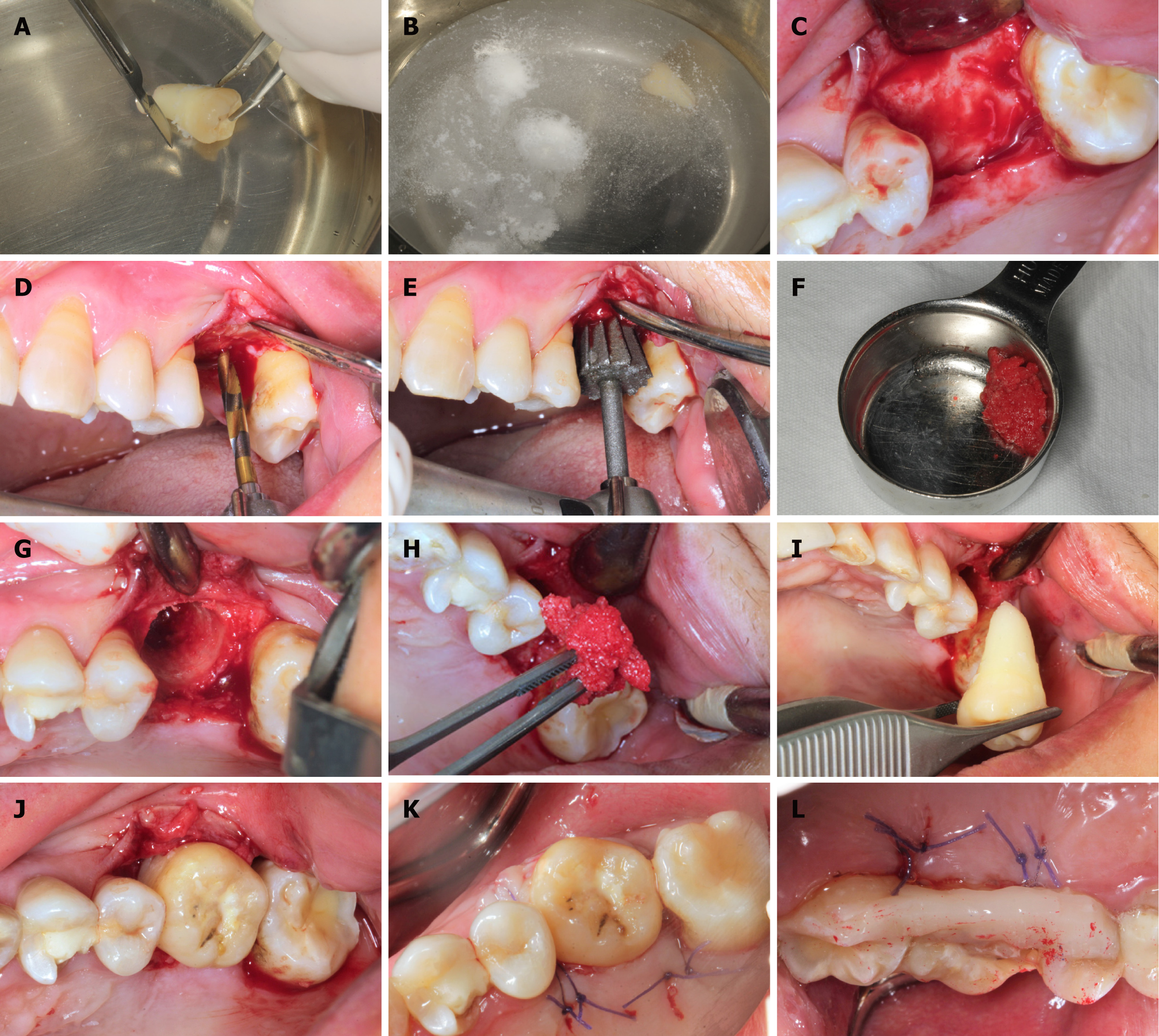
In order to mitigate a potential immunological rejection, the tooth which was carefully extracted with minimal trauma was treated with solutions of 10 g/L cephalosporin, 75 g/L clindamycin hydrochloride, and 50 g/L aspirin in sequence. Then the pilot hole was expanded with progressively wider drills, and the preparation was completed using the 3D printed individual drill. The autogenous bone was collected during the entire drill preparation technique and utilized to fill the compartment. After suture, the tooth was splinted with an acid-etch resin composite splint (Figure 3). The recipient was treated with antibiotics and a compound gargle solution of chlorhexidine gluconate was utilized for 2 wk. The follow-up radiographs and photos were taken after surgery (Figure 4).
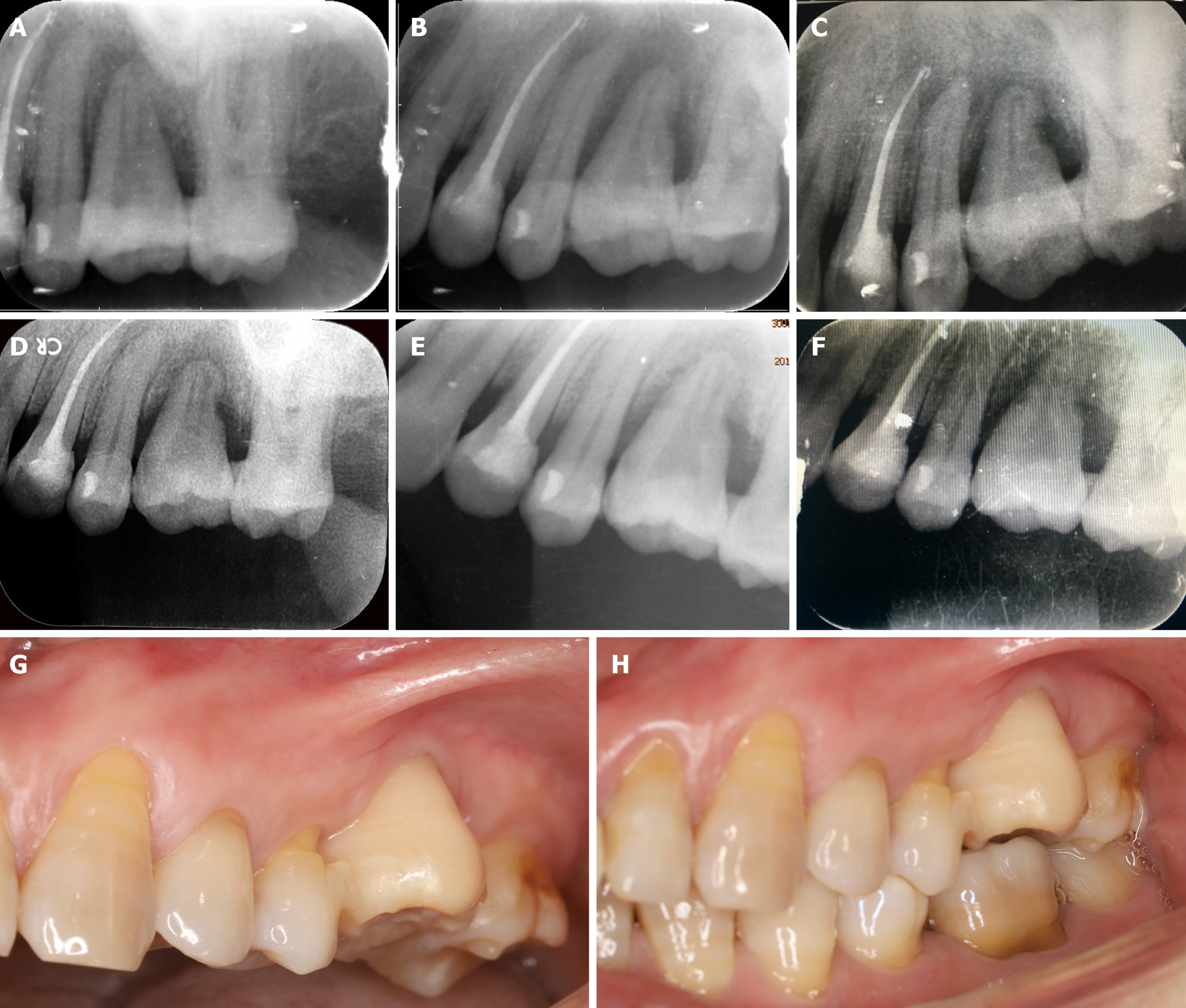
Inflammation in the periodontal area was observed during healing 1 wk after transplantation. Resorption initiated after 2 wk, which was further increased after 4 and 8 wk. Replacement resorption on the external surface showed increasing appea-rance time, initiating at 4 wk. The periodontal ligament was no longer visible by X-ray after 4 wk. No pain or swelling was present; however, the height of the peri-implant papillae began to show some recession. The outcome was less than optimal or reported previously and further observations are needed. Other tooth treating methods such as sintering will be studied and carried out in the future.
Allogenic tooth transplantation has been utilized for five decades with publications occurring in the literature at irregular intervals[3]. While studies regarding the immunological aspects of tooth transplantation were not published until 1963[24], more recently, a greater number of studies concerning these aspects have been performed, demonstrating that teeth can be antigenic and elicit an immune response from the host patient[4]. Today, an overgrowing research development is placed on whole tooth regeneration, yet research in this field remains wishful. Advances in molecular biology, experimental embryology, developmental biology, and bioengineering may one day overcome present limitations[25]. Nevertheless, tooth transplantation has received very little research in comparison owing largely to the developing field of dental implants. In general, the number of tooth transplantation cases have been decreasing and the utilization of new and modern bioengineering techniques and findings from immunological research have been seldom applied to transplantation research in the dental field. This makes this case report provide an insight into the potential development of future avenues of research and discovery in the field of tooth transplantation.
Root resorption is reported to be the most relevant complication in tooth transplan-tation and plays an important role in the long-term prognosis of allotransplanted teeth. However, it is also very common in the first few weeks following surgery. It has been suggested that the selection of autogenic tooth versus allogenic tooth is prominent to reduce the apoptosis of odontoblast-lineage cells, but this study also showed that the immunological rejection may have nothing to do with periodontal tissues[26,27].
Root resorption usually happens as replacement resorption and inflammatory resorption[28]. In previous cases, a surgeon had to remodel the recipient site to the according donor root sizes, which would definitely increase the surgical time required to transplant the tooth, and therefore worsen the prognosis as well as potentially lead to greater bone loss without the precise bur size created from the donor tooth[10]. The replacement resorption is reported to be a response to the operative trauma, which can be lightened by the use of 3D printed burs. Alloimmune rejection also plays an important role during root resorption. Inflammatory resorption can be affected by the endodontic treatment and interestingly the age of recipient[8].
There is also a potential for loss of marginal periodontal attachment which can be caused by pre/preoperative loss of bone and/or inflammation as a result of donor tooth root fracture[8]. As a result, a number of cases end up being failed/lost. Accordingly, a previously study conducted by Schwartz et al[8] found that after 10 years, 76% of allograft tooth transplants were lost and after 15 years, only six grafts (8.2%) were still in function. The findings further concluded that the cause of graft loss was root resorption in 38 cases, inflammatory resorption in 11, replacement resorption in 27, marginal periodontal complication in 2, apical periodontitis in 1, prosthetic failure in 1, and an unknown etiology in 3[8].
In our case report, a similar failure caused by resorption is expected. Nevertheless, this case report is the first attempt at combining modern 3D imaging and printing with allogenic tooth transplantation, which demonstrated plenty of advantages such as an accurate control of material distribution, lower surgical times required, better stability of the transplanted tooth owing to the 3D morphology of the bur, and cost-effectiveness[19,20,29]. With the utilization of 3D printing during tooth transplantation, it is expected that surgical trauma will be minimized with better final tooth stability. Based on previous publications, the use of aspirin was utilized as a means to minimize alloimmune rejection[30]. Aspirin has been shown to inhibit TNF-α and IFN-γ levels and reverse proinflammatory cytokines which may cause a higher immune response, leading to apoptosis of bone marrow mesenchymal stem cells[31].
To date there have been quite a few methods to inhibit alloimmune rejections, including donor and recipient’s matching test, minimizing movement of the periodontal ligament of transplanted teeth, endodontic treatment prior to transplantation, repeated freezing treatment, irradiation of donor’s teeth, and treatment with fluorinated fluid[32,33]. For instance, although Schwartz et al[34] used a monkey model to study the influence of endodontic treatment, and found that the teeth that were endodontically treated significantly decreased inflammatory resorption (almost totally eliminated, P = 0.0003), it had significantly increased replacement resorption (P = 0.0004)[34]. Over 40 years ago, Robinson and Rowlands demonstrated that repeat freezing and thawing and incubation with collagenase and hyaluronidase turned the tooth grafts non-immunogenic[35]. These reports are quite old, yet no recent attempts have been made to further investigate if tooth transplan-tation can become a routine clinical procedure.
3D printing and bioprinting are modalities of additive manufacturing. Compared to other techniques used in tissue engineering, 3D printing has the advantages of accurate precision, resolution, efficiency, and accuracy[16,23]. Four main 3D printing techniques exist including inkjet, laser-assisted, extrusion, and stereolithography printing[36-39]. Although autogenic and allogenic tooth transplantation has a long history of use, several limitations still exist. In previous cases, since differences in root shape and length exist, surgeons have had to reposition the donor tooth back to its original socket and remodel the recipient site with a round implant bur[10]. The remodeling of the recipient site adds additional time to the surgical procedure with the possibility of surgically removing more bone than needed. In the present case report, the specific design of our 3D printed bur allowed for the recipient site to better match the donor tooth. With the ability to 3D print in layers, even the protuberance of the root can be matched and 3D printed, thereby minimizing unnecessary bone loss.
There are many factors that may affect the implanted tooth’s primary stability including bone quality and quantity, surgical technique utilized, and the tooth geometry[40]. Since the shape of the donor’s and recipient’s roots are generally mismatching, implant stability is hard to predict and therefore the advantages of 3D printing may provide a better solution to the current standards. The advantages of 3D printing include accurate control of material distribution and sizing, fast production, scalability, and cost-effectiveness, which have made this technology successful in many areas of medicine with positive outcomes[19,20]. It is therefore conceivable that since various allogenic transplantations are utilized in many areas of medicine including heart, lungs, kidneys, and other complex organs, the ability for dental clinicians to utilize this technique in the coming years should not be deemed unrealistic. With the advancements made in modern medicine and tissue engineering, future research endeavors should be geared towards utilizing this low-cost modality where 3D printing may help improve the predictability of such cases. In the present case, we report the first published attempt at utilizing 3D printing during a tooth transplantation procedure. Future research is necessary to further improve this technology, but this article offers a pioneering first attempt at such a therapy.
Our study presents a pioneering case combining 3D printing with allogenic tooth transplantation. A 3D printing system was introduced to print an individualized reamer drill for preparing the implant placement bed and the donor’s tooth as a template for the drill. With the utilization of 3D printing, the surgical trauma was minimized and the tooth implant stability was more suitable. A detailed progress and prognosis of this cases were recorded, which makes the case very useful for reference purposes since it is the first study of its kind. Other tooth treating methods such as sintering will be studied and carried out in the future. This article hopes to enhance our understanding of allogenic tooth transplantation and 3D printing, and may potentially lead to tooth transplantation being utilized more frequently - especially since transplantations are so commonly utilized in many other fields of medicine with high success rates.
| 1. | Andreasen JO, Paulsen HU, Yu Z, Bayer T, Schwartz O. A long-term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur J Orthod. 1990;12:14-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 305] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | Adell R. Tissue integrated prostheses in clinical dentistry. Int Dent J. 1985;35:259-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Atkinson ME. Histopathological and immunological aspects of tooth transplantation. J Oral Pathol. 1978;7:43-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Atkinson ME. A histological study of tooth allografts transplanted to untreated and immunologically prepared mice. J Oral Pathol. 1975;4:167-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Atkinson ME. A histological study of tooth grafts in an inbred strain of mice. J Oral Pathol. 1972;1:115-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Revathy V, Suryakanth M, Poornima P, Subba Reddy VV. Allotransplantation of tooth: a case report. J Clin Pediatr Dent. 2012;37:1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Meffert RM, Langer B, Fritz ME. Dental implants: a review. J Periodontol. 1992;63:859-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 88] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Schwartz O, Frederiksen K, Klausen B. Allotransplantation of human teeth. A retrospective study of 73 transplantations over a period of 28 years. Int J Oral Maxillofac Surg. 1987;16:285-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Nordenram A. Allogeneic tooth transplantation with an observation time of 16 years. Clinical report of 32 cases. Swed Dent J. 1982;6:149-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Herrera H, Herrera H, Leonardo MR, de Paula e Silva FW, da Silva LA. Treatment of external inflammatory root resorption after autogenous tooth transplantation: case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e51-e54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Xiang Gu G, Su I, Sharma S, Voros JL, Qin Z, Buehler MJ. Three-Dimensional-Printing of Bio-Inspired Composites. J Biomech Eng. 2016;138:021006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 49] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Seunarine K, Gadegaard N, Tormen M, Meredith DO, Riehle MO, Wilkinson CD. 3D polymer scaffolds for tissue engineering. Nanomedicine (Lond). 2006;1:281-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Rasperini G, Pilipchuk SP, Flanagan CL, Park CH, Pagni G, Hollister SJ, Giannobile WV. 3D-printed Bioresorbable Scaffold for Periodontal Repair. J Dent Res. 2015;94:153S-157S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 197] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 14. | Wang X, Ao Q, Tian X, Fan J, Wei Y, Hou W, Tong H, Bai S. 3D Bioprinting Technologies for Hard Tissue and Organ Engineering. Materials (Basel). 2016;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 15. | Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol. 2014;32:773-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3943] [Cited by in RCA: 3914] [Article Influence: 355.8] [Reference Citation Analysis (0)] |
| 16. | Mandrycky C, Wang Z, Kim K, Kim DH. 3D bioprinting for engineering complex tissues. Biotechnol Adv. 2016;34:422-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1198] [Cited by in RCA: 1043] [Article Influence: 104.3] [Reference Citation Analysis (1)] |
| 17. | Bajaj P, Schweller RM, Khademhosseini A, West JL, Bashir R. 3D biofabrication strategies for tissue engineering and regenerative medicine. Annu Rev Biomed Eng. 2014;16:247-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 507] [Cited by in RCA: 403] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 18. | Boyle I, Rong YM, Brown DC. A review and analysis of current computer-aided fixture design approaches. Robot Cim-Int Manuf. 2011;27:1-12. [DOI] [Full Text] |
| 19. | Legemate K, Tarafder S, Jun Y, Lee CH. Engineering Human TMJ Discs with Protein-Releasing 3D-Printed Scaffolds. J Dent Res. 2016;95:800-807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 20. | Shao H, Sun M, Zhang F, Liu A, He Y, Fu J, Yang X, Wang H, Gou Z. Custom Repair of Mandibular Bone Defects with 3D Printed Bioceramic Scaffolds. J Dent Res. 2018;97:68-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 21. | Jung JW, Lee JS, Cho DW. Computer-aided multiple-head 3D printing system for printing of heterogeneous organ/tissue constructs. Sci Rep. 2016;6:21685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 22. | Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants. 2007;22:743-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Mesa F, Muñoz R, Noguerol B, de Dios Luna J, Galindo P, O'Valle F. Multivariate study of factors influencing primary dental implant stability. Clin Oral Implants Res. 2008;19:196-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Cserepfalvi M. Clinical report of homotransplantation. J Am Dent Assoc. 1963;67:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Chai Y, Slavkin HC. Prospects for tooth regeneration in the 21st century: a perspective. Microsc Res Tech. 2003;60:469-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Unno H, Suzuki H, Nakakura-Ohshima K, Jung HS, Ohshima H. Pulpal regeneration following allogenic tooth transplantation into mouse maxilla. Anat Rec (Hoboken). 2009;292:570-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Saito K, Nakatomi M, Kenmotsu S, Ohshima H. Allogenic tooth transplantation inhibits the maintenance of dental pulp stem/progenitor cells in mice. Cell Tissue Res. 2014;356:357-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 28. | Lin S, Ashkenazi M, Karawan M, Teich ST, Gutmacher Z. Management of Ankylotic Root Resorption Following Dental Trauma: A Short Review and Proposal of a Treatment Protocol. Oral Health Prev Dent. 2017;15:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 29. | Diment LE, Thompson MS, Bergmann JHM. Clinical efficacy and effectiveness of 3D printing: a systematic review. BMJ Open. 2017;7:e016891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 30. | Shi S, Yamaza T, Akiyama K. Is aspirin treatment an appropriate intervention to osteoporosis? Fut Rheumatol. 2008;3:499-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Liu Y, Wang L, Kikuiri T, Akiyama K, Chen C, Xu X, Yang R, Chen W, Wang S, Shi S. Mesenchymal stem cell-based tissue regeneration is governed by recipient T lymphocytes via IFN-γ and TNF-α. Nat Med. 2011;17:1594-1601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 554] [Cited by in RCA: 572] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 32. | Li W, Deng F, Wang Y, Ma C, Wang Y. Immune tolerance of mice allogenic tooth transplantation induced by immature dendritic cells. Int J Clin Exp Med. 2015;8:5254-5262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (1)] |
| 33. | Mellberg JR, Shulman L. Treatment of human teeth with fluoride for replantation and allotransplantation. J Dent Res. 1974;53:844-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Schwartz O, Andreasen JO. Allotransplantation and autotransplantation of mature teeth in monkeys: the influence of endodontic treatment. J Oral Maxillofac Surg. 1988;46:672-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Robinson PJ, Rowlands DT. Evidence of the alloimmunogenic potential of donor periodontal ligament. Am J Pathol. 1974;75:503-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 36. | Bilgin MS, Erdem A, Dilber E, Ersoy İ. Comparison of fracture resistance between cast, CAD/CAM milling, and direct metal laser sintering metal post systems. J Prosthodont Res. 2016;60:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Mangano F, Chambrone L, van Noort R, Miller C, Hatton P, Mangano C. Direct metal laser sintering titanium dental implants: a review of the current literature. Int J Biomater. 2014;2014:461534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 38. | Prabhu R, Prabhu G, Baskaran E, Arumugam EM. Clinical acceptability of metal-ceramic fixed partial dental prosthesis fabricated with direct metal laser sintering technique-5 year follow-up. J Indian Prosthodont Soc. 2016;16:193-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Venkatesh KV, Nandini VV. Direct metal laser sintering: a digitised metal casting technology. J Indian Prosthodont Soc. 2013;13:389-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 34] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 40. | Sennerby L, Roos J. Surgical determinants of clinical success of osseointegrated oral implants: a review of the literature. Int J Prosthodont. 1998;11:408-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gonzalez F S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Xing YX