Published online Sep 6, 2019. doi: 10.12998/wjcc.v7.i17.2505
Peer-review started: March 28, 2019
First decision: June 17, 2019
Revised: July 25, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 6, 2019
Processing time: 164 Days and 18.9 Hours
Sarcoidosis is a granulomatous disease of unknown etiology that most often impacts the lungs. Cutaneous manifestations of sarcoidosis are seen among 9%-37% of patients. Subcutaneous sarcoidosis is a rare presentation of cutaneous sarcoidosis with estimates of frequency ranging from 1.4%-16%. To date, very few articles and case reports have been written about this subject. In this paper, we describe a case of subcutaneous sarcoidosis and perform a review of the literature to determine if there are commonalities among patients who present with subcutaneous sarcoidosis.
A 38-year-old female, with a past medical history of arthritis and recurrent nephrolithiasis, presents with an 8-mo history of 4 firm, asymptomatic, skin-colored nodules on her left and right upper extremities and neck. Needle biopsy and post-excisional pathology report both revealed well-formed, dense, non-caseating granulomas localized to the subcutaneous tissue. Chest computed tomography revealed mild mediastinal lymphadenopathy. A diagnosis of subcutaneous sarcoidosis was made, and the lesions were surgically removed.
Commonalities among patients presenting with subcutaneous sarcoidosis include: middle-aged female, lesions localizing to the upper or lower limbs, lymphadenopathy or pulmonary infiltration on chest imaging, elevated serum angiotensin-converting enzyme.
Core tip: Recognizing patterns of subcutaneous sarcoidosis is important for hand surgeons and other surgical specialties that do not commonly see this patient population in order to rapidly identify and diagnose a disease that has extra-cutaneous manifestations and can lead to greater morbidity and mortality when not diagnosed or treated early.
- Citation: Mehrzad R, Festa J, Bhatt R. Subcutaneous sarcoidosis of the upper and lower extremities: A case report and review of the literature. World J Clin Cases 2019; 7(17): 2505-2512
- URL: https://www.wjgnet.com/2307-8960/full/v7/i17/2505.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i17.2505
Sarcoidosis is a chronic systemic granulomatous disease of unknown etiology characte-rized by the presence of non-caseating granulomas in affected organs[1]. he non-caseating granulomas of sarcoidosis can be found anywhere on the body and involve many different organs. In the head and neck, sarcoidosis typically impacts the cervical lymph nodes, globe, parotid, and larynx with up to 5% of patients demonstrating facial nerve involvement[2]. Ocular involvement is also seen, presenting as uveitis, scleritis, and chorioretinitis[2]. Typically, the lungs are the primary site of disease with cutaneous manifestations being the second most common site. Cutaneous manifestations of Sarcoidosis are seen in up to 9%-37% of patients[3,4]. One particular manifestation of cutaneous involvement, subcutaneous sarcoid nodules, is a rare finding. Previous estimates of the frequency of subcutaneous sarcoidosis ranged from 1.4%-6%, with more recent studies suggesting an occurrence rate of 11.8%-16% among patients presenting with cutaneous sarcoid involvement[3,5-7]. This variant of Sarcoidosis is defined clinically by asymptomatic, non-tender, flesh colored nodules usually ranging between 0.5-2.0 cm[6,8]. Histologically, subcutaneous sarcoidosis is defined by the presence of non-caseating granulomas present in the subcutaneous tissue[6]. On ultrasound imaging these lesions present as an irregularly defined mass with hyper and hypoechoic areas[9]. Fludeoxyglucose (FDG) positron emission tomography (PET) / computed tomography (CT) has also been used to identify sarcoid lesions and presents as increased uptake in subcutaneous areas[10]. While helpful, FDG PET/CT may not be able to differentiate between connective tissue diseases as Sjrogen’s Syndrome also presents as increased uptake[11]. Additionally, many soft tissue diseases can look similar on magnetic resonance imaging (MRI) making defining imaging characteristics of each disease important to diagnosis. On MRI imaging Sarcoid lesions involving the face and neck will appear with high signal intensity on T2-weighted images and enhancement on contrast-enhanced images[2]. Given that Wegener’s Granulomatosis can mimic Sarcoidosis in the head and neck, MRI imaging helps differentiate these two soft tissue diseases as Wegener’s Granulomatosis will appear as hypodense on T1 and T2-weighted images with variable degrees of enhancement with contrast[2]. Similarly, both sarcoidosis and Scleroma can impact the cervical lymph nodes making diagnosis difficult. MR imaging is again a useful tool in differentiating these two diseases in the lymph nodes as Scleroma will appear as low signal intensity on T1 and high signal intensity on T2 imaging with homogeneous pattern of contrast enhancement, and Sarcoidosis will have a foamy appearance on T1 weighted imaging[2,12]. Lupus Both Sarcoidosis and another soft tissue disease like scleroderma can impact the lymph nodes in the neck Recent literature has suggested a strong correlation between subcutaneous sarcoidosis and evidence of systemic sarcoid involvement, and that sarcoid lesions may be an early finding indicative of systemic disease[7,13,14]. Given its correlation with systemic illness, the ability to correctly identify subcutaneous sarcoid lesions is an important diagnostic tool for physicians in the early stages of sarcoidosis. We describe here a case of subcutaneous sarcoidosis and review the literature to determine if there are any commonalities in the presentation of this disease among patients, and to better assist clinicians with diagnosing this rare disorder.
A literature search was performed of the MEDLINE and PubMed database using keywords as “Subcutaneous sarcoidosis” and “Subcutaneous Sarcoidosis”, combined with “hand”, “hand surgery”, “Upper extremity surgery”, yielding 202 results. The search includes all articles published since 2000. The search was limited to studies published in English and performed on humans. Cases without either a serum angiotensin-converting enzyme (ACE) level or a chest imaging study for all patients reported were excluded. Ultimately 29 articles were selected using the diagnostic criteria of subcutaneous sarcoidosis first proposed by Vainsencher et al[6]. These 29 articles represent 82 cases of subcutaneous sarcoidosis dating back to 1966.
A 38-year-old Caucasian female was referred to Plastic Surgery from Dermatology after presenting with an 8-mo history of 4 firm, asymptomatic, skin-colored nodules on her left and right upper extremities and neck.
A past medical history of arthritis and recurrent nephrolithiasis.
She denied any family history of soft tissue masses or autoimmune disorders.
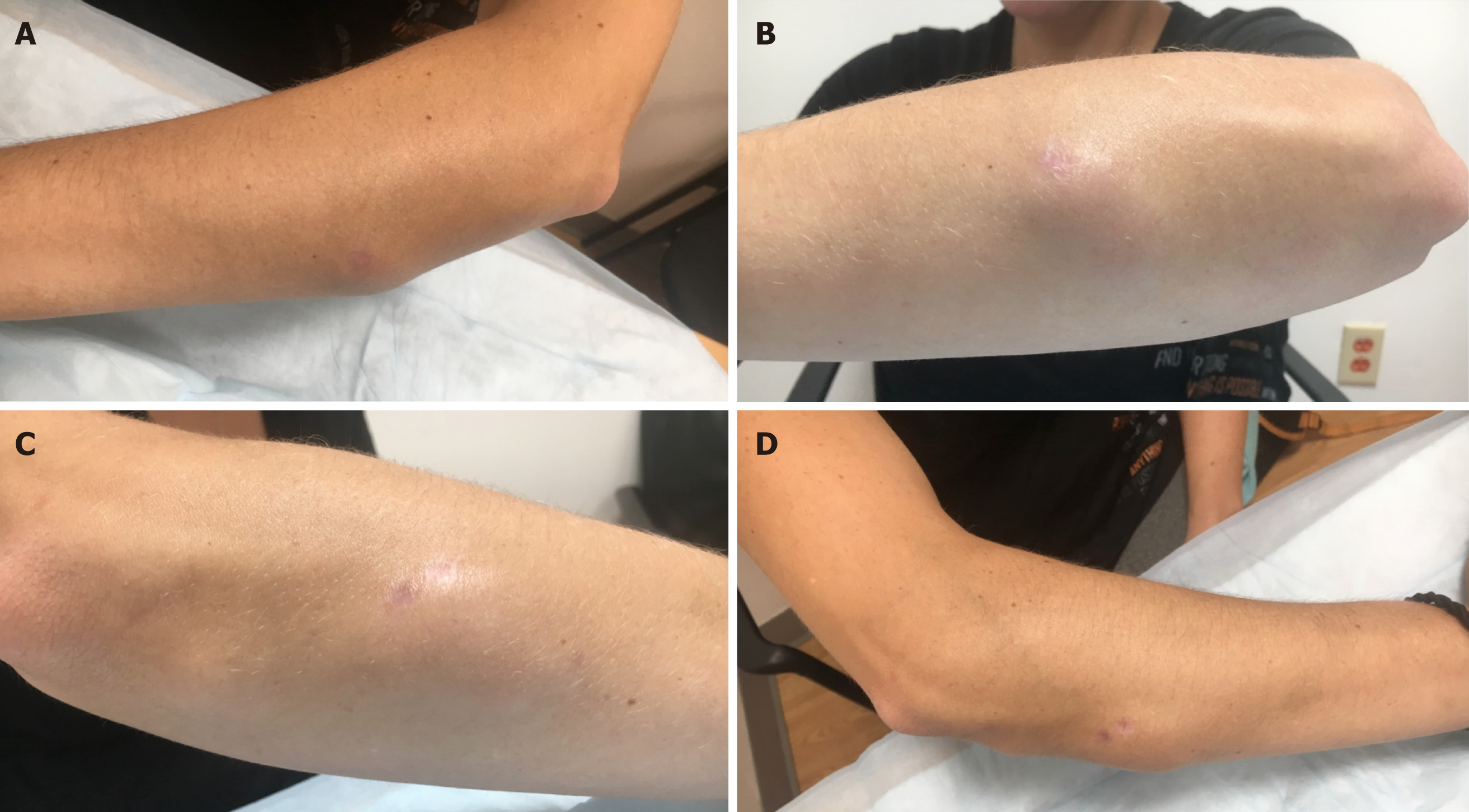
The mass on the posterior aspect of her neck measured 0.5 cm x 5 cm. The nodule on her left forearm measured 2 cm x 3 cm (Figure 1A and B). On the extensor surface of her right forearm were two masses measuring 1 cm x 1.4 cm and 3.5 cm x 4.5 cm respectively (Figure 1C and D). The overlying skin was normal. At the time of the plastic surgery consult, the patient was compliant with her medication regimen of dextroamphetamine-amphetamine 30 mg by mouth once daily, and acetaminophen 500 mg Tab as needed for arthritic pain.
The complete blood count with differential was normal. Comprehensive metabolic panel was normal. Erythrocyte sedimentation rate, C-Reactive Protein, Anti-SCL, Rheumatoid Factor, and antinuclear antibody were all within normal limits. Her Serum ACE level was also within normal limits with a value of 53 U/L (normal 9-67 U/L). While chest radiograph was normal, chest computed tomography revealed mild mediastinal lymphadenopathy.
Based on the histopathological findings of the cutaneous nodules and the computed tomography finding of mediastinal lymphadenopathy, a diagnosis of subcutaneous sarcoidosis was made.
Patient was advised on various treatment options and chose to have the lesions surgically excised by a plastic surgeon.
Needle biopsy and post-excisional pathology report both revealed the presence of well-formed, dense, non-caseating granulomas located in the subcutaneous tissue. There was no evidence of organisms with Acid-Fast and Grocott’s Methamine Silver staining.
Among the articles selected for this literature review, 4 were hospital based retrospective chart reviews.
The largest study was conducted by Ahmed et al[14] in 2006 out of the Mayo Clinic[14]. The authors reviewed all cases filed under the diagnosis of sarcoidosis, nonspecific granulomas and granulomatous panniculitis between 1966-2001. Ultimately 21 cases of subcutaneous sarcoidosis were reviewed. Among the 21 patients diagnosed with subcutaneous sarcoidosis, 15 were female and 6 were male. The mean age was 46.3. In 20/21 patients, lesions were located on more than one anatomical site. The most common anatomical site was the upper extremity with all 21 patients presenting with a lesion in this area. Lower extremity lesions were also common as they were found in 16/21 patients. In 15/21 patients, other types of cutaneous lesions of sarcoidosis co-existed with the subcutaneous lesion with plaques presenting in 6 patients, papules in 4 patient, erythema nodosum in 4 patients, and scar sarcoidosis in 1 patient. Out of the 20 patients who were evaluated for systemic involvement, 16 had pulmonic involvement evidenced by an abnormal chest radiograph. 15/16 patients exhibited bilateral hilar lymphadenopathy, with 6 of these cases exhibiting an additional finding of paratracheal and pulmonary infiltrates. The most common systemic involvements, other than the lung, included arthritis, peripheral neuropathy and renal dysfunction. Out of the 11 patients tested for Serum ACE, 3 patients had elevated levels.
In 2016, Ando et al[15] reviewed the charts of 130 patients diagnosed with systemic sarcoidosis between 2000-2012 out of Oita University of Japan medical center. 37/130 patients presented with cutaneous sarcoid lesions with 9/37 presenting with subcutaneous sarcoidosis. Among their cohort were 8 female patients and 1 male patient with an average age of 52.5 years. Six of the patients only had lesions on their lower extremities. The other 3 patients had lesions on their upper extremity and trunk, upper and lower extremities, and hip respectively. Two patients presented with sarcoid plaques and scars in addition to their subcutaneous nodules. All 9 patients were found to have lung involvement with 4 of these patients presenting with an additional involvement of their eyes, and 3 patients with an involvement of their muscles. On chest radiograph 3 patients had lymphadenopathy, and 6 patients had lymphadenopathy with pulmonary infiltrates.
In 2005, Marcoval et al[7] conducted a retrospective chart review analyzing 480 patients admitted with systemic sarcoidosis from 1974-2002 at the University Hospital of Bellvitge in Barcelona, Spain. A total of 85/480 patients demonstrated sarcoid cutaneous involvement with 10/85 demonstrating subcutaneous sarcoidosis. 9/10 of the patients were female, and the average age of presentation was 52.6 years. All of the patients presented with nodules on their upper extremities with 5 patients presenting with additional nodules on their lower extremities. In addition to subcutaneous nodules, 4 patients presented with erythema nodosum, and 1 patient presented with sarcoid plaques and papules. 8 patients presented with lymphade-nopathy on chest radiograph, and 1 patient presented with lymphadenopathy and pulmonary infiltrate.
In 2011 the same lead author, Marcoval et al[3], conducted a similar retrospective chart review analyzing 86 patients with systemic sarcoidosis who presented with cutaneous involvement to the Sarcoid Clinic of Bellvitge University Hospital in Barcelona, Spain. A total of 14/86 patients presented with subcutaneous nodules. Among the 14 patients, 11 were female and 3 were male. All 14 patients had nodules limited to the upper and lower extremities with 6 patients presenting with lesions on their arms, 1 patient presenting with lesions on their legs, and 7 patients presenting with lesions on both their upper and lower extremities. 13/14 patients were found to have abnormal chest radiograph findings with 11 patients exhibiting hilar lymphadenopathy, and 2 exhibiting hilar lymphadenopathy and lung infiltrate. Among the 14 patients, 12 had systemic involvement with arthritis being the most common presentation in 6 of the patients (Table 1).
| Authors | Sex | Average age | Serum angiotensin-converting enzyme | Chest X-ray | Most common site of lesion | Most common site of systemic involvement other than the lungs |
| Ahmed et al[14], 2006 | 15F/6M | 46.3 | 3/11 Elevated | 9/16 Lymphadenopathy, 6/16 Pulmonary infiltration | Upper extremities | Joints-arthritis |
| Ando et al[15], 2016 | 8F/1M | 52.5 | 7/9 Elevated | 3/9 Lymphadenopathy, 6/9 Lymphadenopathy with pulmonary infiltration | Upper extremities | Eyes |
| Marcoval et al[7], 2005 | 9F/1M | 52.6 | NA | 8/10 Lymphadenopathy, 1/10 Lymphadenopathy with pulmonary infiltration | Upper extremities | NA |
| Marcoval et al[3], 2011 | 11F/3M | N/A | NA | 11/14 Lymphadenopathy, 2/14 Lymphadenopathy with pulmonary infiltration | Upper and lower extremities | Joints-arthritis |
In our literature review we found 25 case reports representing 28 unique cases of subcutaneous sarcoidosis between 2000-2019. Notable features of these cases are listed in Table 2. The average age of patients among all reports was 53 years old and 21/28 of the patients were female.
| Authors | Sex | Average age | Serum angiotensin-converting enzyme | Chest computed tomography | Chest X-ray | Site of lesion | Extracutaneous involvement other than the lungs |
| Barnadas et al[16], 2000 | F | 38 | Normal | Normal | Normal | Upper and lower limbs | Malaise, joint pains |
| Girão et al[17], 2000 | M | 37 | Elevated | Lymphadenopathy | Lower limb | Hands and feet arthralgia | |
| Dalle Vedove et al[18], 2011 | 1F/1M | 75 | 2/2 Elevated | 1/2 Mediastinal Lymphadenopathy, 1/2 Lymphadenopathy with pulmonary infiltration | 2/2 Normal | Upper and lower limbs | 1/2 Uveitis |
| Kim et al[19], 2014 | M | 61 | Elevated | Normal | Trunk | Renal | |
| Fichtel et al[20], 2006 | F | 42 | Elevated | Normal | Upper and lower limbs | None | |
| Bosnic et al[21], 2010 | F | 51 | Elevated | Normal | Face | None | |
| Kim et al[22], 2017 | M | 33 | Lymphadenopathy with pulmonary infiltration | Face, toe | None | ||
| Won et al[23], 2016 | F | 54 | Normal | Lower limb | None | ||
| Marcoval et al[24], 2008 | F | 49 | Elevated | Lymphadenopathy | Upper and lower limbs | None | |
| Dulgueroy et al[25], 2015 | F | 34 | Elevated | Lymphadenopathy with pulmonary infiltration | Face | None | |
| Ruangchaijatuporn et al[26], 2016 | M | 56 | Normal | Lower limb | None | ||
| Watanbe et al[27], 2007 | F | 70 | Elevated | Lymphadenopathy | Lower limb | Polyneuropathy of limbs | |
| Janegova et al[28], 2016 | F | 59 | Lymphadenopathy with pulmonary infiltration | Foot | None | ||
| Yamaguchi et al[29], 2013 | F | 85 | Elevated | Lymphadenopathy with pulmonary infiltration | Lymphadenopathy | Upper and lower limbs | Joints arthralgia |
| Mori et al[30], 2018 | F | 72 | Elevated | Lower limb | Renal and cardiac dysfunction | ||
| Kwan et al[31], 2015 | F | 53 | Elevated | Lymphadenopathy | Upper and lower limbs | None | |
| Miida et al[32], 2009 | F | 62 | Elevated | Lymphadenopathy with pulmonary infiltration | Lymphadenopathy | Upper limbs | Uveitis, renal dysfunction, splenic nodules |
| Bianchini et al[33], 2010 | F | 38 | Elevated | Normal | Normal | Face | None |
| Kerner et al[34], 2008 | F | 53 | Lymphadenopathy | Lymphadenopathy | Upper and lower limbs | Facial nerve palsy, arthralgia | |
| Kim et al[35], 2013 | F | 52 | Elevated | Lymphadenopathy with pulmonary infiltration | Lymphadenopathy | Upper and lower limbs | None |
| Guccione et al[36], 2017 | M | 40 | Lymphadenopathy | Upper limbs, trunk | None | ||
| Meyer-Gonzalez et al[37], 2011 | 3F | 52.6 | 1/3 Normal, 2/3 Elevated | 1/3 Lymphadenopathy, 2/3 Lymphadenopathy with pulmonary infiltration | 3/3 Lymphadenopathy | Upper and lower limbs | Dactylitis, lower limb weakness |
| Moscatelli et al[38], 2011 | M | 41 | Lymphadenopathy with pulmonary infiltration | Normal | Hand | None | |
| Shigemitsu et al[39], 2008 | F | 65 | Lymphadenopathy | Upper extremity | None | ||
| Celik et al[40], 2010 | F | 53 | Elevated | Lymphadenopathy with pulmonary infiltration | Lymphadenopathy | Foot | None |
Out of the 20 reported cases that checked for serum ACE, elevated levels were found in 18 patients. Abnormal Chest Computed Tomography results were found in 16/21 patients. Abnormal Chest Radiograph results were found in 12/19 patients. The most common site of lesion seemed to be the upper and lower limbs with 17/25 patients presenting with subcutaneous sarcoid nodules in one or both of these locations. Most reports did not comment on extracutaneous involvement other than the lung, but those did reported a range of systemic findings including arthritis, renal dysfunction, uveitis, dactylitis, and limb weakness. Sarcoidosis is a chronic systemic granulomatous disease of unknown etiology[1]. Although the lungs are typically the primary site of disease, cutaneous manifestations of the Sarcoidosis can be seen in up to 9-37% of patients[3,4]. Subcutaneous sarcoid nodules, is a rare cutaneous sarcoidosis finding that typically presents as asymptomatic, non-tender, flesh colored nodules ranging in size between 0.5-2.0 cm[6,8]. Histological examination of a subcutaneous sarcoid nodule reveals the presence of non-caseating granulomas present in the subcutaneous tissue[6].
Our patient, a 38 year old female, presented with an 8 month history of 4 subcu-taneous nodules ranging in size from 0.5cm-5cm. Her past medical history was significant for arthritis and recurrent nephrolithiasis. Upon testing we found that she had a normal chest radiograph and her serum ACE levels were within normal limits. On chest computed tomography we found evidence of mild mediastinal lymphadenopathy, pathognomonic for sarcoidosis.
In analyzing the 29 publications from 2000-2019 along with our own case, we reviewed 83 cases of subcutaneous sarcoidosis. Among the 83 patients, 65 (78.3%) were female and the average age of presentation was 51.1 years old. The upper and lower extremities were the most common site of subcutaneous sarcoidosis development with 76/83 (91.6%) patients presenting with at least one lesion in these anatomical areas. In our analysis we learned that findings of lymphadenopathy or lymphadenopathy with pulmonary infiltrate was a very common chest radiograph finding among patients presenting with subcutaneous lesions. In total, 58/69 (84.1%) patients had abnormal chest radiograph findings. Among the 22 patients that received a chest computed tomography scan, abnormal findings of lymphadenopathy or pulmonary infiltrate were found in 17/22 (77.2%) patients. Elevated levels of serum ACE is also a common finding, although not as prevalent as lung involvement. In total, among the cases that measured serum ACE, 28/41 (68.3%) patients presented with elevated levels. Instances of sarcoidosis organ involvement other than the lung seems to be a rarer finding presenting in only 29/49 (59.1%) patients. Assessment of the number of patients with systemic involvement other than the lung, however, was difficult as some articles did not include this information within their study. In conclusion, our literature review shows that subcutaneous sarcoidosis primarily impacts middle-aged women, is most frequently found on the upper or lower limbs, and commonly presents with abnormal findings of lymphadenopathy or pulmonary infiltration on chest imaging as well as elevated levels of serum ACE. These patterns and findings are important for hand surgeons and other surgical specialties that do not commonly see this patient population to be able to rapidly identify and diagnose a disease that has extra-cutaneous manifestations and can lead to greater morbidity and mortality when not diagnosed and treated early.
| 1. | Lazarus A. Sarcoidosis: epidemiology, etiology, pathogenesis, and genetics. Dis Mon. 2009;55:649-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Razek AA, Castillo M. Imaging appearance of granulomatous lesions of head and neck. Eur J Radiol. 2010;76:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Marcoval J, Mañá J, Rubio M. Specific cutaneous lesions in patients with systemic sarcoidosis: relationship to severity and chronicity of disease. Clin Exp Dermatol. 2011;36:739-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Mañá J, Marcoval J, Rubio M, Labori M, Fanlo M, Pujol R. Granulomatous cutaneous sarcoidosis: diagnosis, relationship to systemic disease, prognosis and treatment. Sarcoidosis Vasc Diffuse Lung Dis. 2013;30:268-281. [PubMed] |
| 5. | Mayock RL, Bertrand P, Morrison CE, Scott JH. Manifestations of sarcoidosis. analysis of 145 patients, with a review of nine series selected from the literature. Am J Med. 1963;35:67-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 504] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Vainsencher D, Winkelmann RK. Subcutaneous sarcoidosis. Arch Dermatol. 1984;120:1028-1031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 53] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Marcoval J, Maña J, Moreno A, Peyri J. Subcutaneous sarcoidosis--clinicopathological study of 10 cases. Br J Dermatol. 2005;153:790-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Haimovic A, Sanchez M, Judson MA, Prystowsky S. Sarcoidosis: a comprehensive review and update for the dermatologist: part I. Cutaneous disease. J Am Acad Dermatol. 2012;66:699.e1-18; quiz 717-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 116] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Malik UT, Aslam F. Ultrasound for the rheumatologist - Subcutaneous Sarcoidosis. Acta Reumatol Port. 2016;41:376-377. [PubMed] |
| 10. | Bompard F, de Menthon M, Gomez L, Gottlieb J, Saleh NS, Chekroun M, Grimon G, Goujard C, Durand E, Besson FL. 18F-FDG PET/CT of sarcoidosis with extensive cutaneous and subcutaneous nodules: the snow leopard sign. Eur J Nucl Med Mol Imaging. 2019;46:1980-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Abdel Razek AA. Imaging of connective tissue diseases of the head and neck. Neuroradiol J. 2016;29:222-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Abdel Razek AA. Imaging of scleroma in the head and neck. Br J Radiol. 2012;85:1551-1555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Marcoval J, Moreno A, Mañá J, Peyri J. Subcutaneous sarcoidosis. Dermatol Clin. 2008;26:553-556, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Ahmed I, Harshad SR. Subcutaneous sarcoidosis: is it a specific subset of cutaneous sarcoidosis frequently associated with systemic disease? J Am Acad Dermatol. 2006;54:55-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 73] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Ando M, Miyazaki E, Hatano Y, Nishio S, Torigoe C, Yamasue M, Mukai Y, Nureki S, Kadota J. Subcutaneous sarcoidosis: a clinical analysis of nine patients. Clin Rheumatol. 2016;35:2277-2281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Barnadas MA, Rodríguez-Arias JM, Alomar A. Subcutaneous sarcoidosis associated with vitiligo, pernicious anaemia and autoimmune thyroiditis. Clin Exp Dermatol. 2000;25:55-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Girão L, Bajanca R, Feio AB, Apetato M. Systemic sarcoidosis revealed by the coexistence of scar and subcutaneous sarcoidosis. J Eur Acad Dermatol Venereol. 2000;14:428-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Dalle Vedove C, Colato C, Girolomoni G. Subcutaneous sarcoidosis: report of two cases and review of the literature. Clin Rheumatol. 2011;30:1123-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 19. | Kim JM, Song YK, Park SJ, Hwang YH, Sung SA, Lee SY, Joo JE, Oh SW. Subcutaneous sarcoidosis presenting as a suprapubic mass, acute kidney injury, and hypercalcemia. Korean J Intern Med. 2014;29:535-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Fichtel JC, Duckworth AK, Soares T, Lesher JL. Subcutaneous sarcoidosis presenting after treatment of Cushing's disease. J Am Acad Dermatol. 2006;54:360-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Bosnić D, Baresić M, Bagatin D, Ilić I. Subcutaneous sarcoidosis of the face. Intern Med. 2010;49:589-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Kim KS, Lim DS, Choi JH, Hwang JH, Lee SY. Subcutaneous Sarcoidosis Occurring in Both Chin and Toe. Arch Craniofac Surg. 2017;18:207-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Won KY, Park SY, Lee SH. Subcutaneous Sarcoidosis Mimicking Cellulitis. J Rheumatol. 2016;43:674-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Marcoval J, Moreno A, Mañá J. Subcutaneous sarcoidosis localised to sites of previous desensitizing injections. Clin Exp Dermatol. 2008;33:132-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Dulguerov N, Vankatova L, Landis BN. Subcutaneous sarcoidosis in a rhinoplasty scar. BMJ Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 26. | Ruangchaijatuporn T, Chang EY, Chung CB. Solitary subcutaneous sarcoidosis with massive chronic prepatellar bursal involvement. Skeletal Radiol. 2016;45:1741-1745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 27. | Watanabe T, Yoshida Y, Yamamoto O. Subcutaneous sarcoidosis with sarcoidal polyneuropathy. Acta Derm Venereol. 2007;87:374-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Janegova A, Janega P, Kovac O, Dragun J, Zakutansky A, Mihalova R, Marinova P, Babal P. Plantar subcutaneous sarcoidosis - a rare form of skin sarcoidosis: unusual plantar aponeurosis location of sarcoidosis as primary manifestation of asymptomatic systemic disease. J Cutan Pathol. 2016;43:475-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Yamaguchi S, Shinoda K, Taki H, Hounoki H, Okumura M, Tobe K. Systemic sarcoidosis with subcutaneous lesions in an 85-year-old female. J Am Geriatr Soc. 2013;61:306-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Mori T, Yamamoto T. Secondary calcification associated with subcutaneous sarcoidosis. J Dermatol. 2018;45:e282-e283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Kwan JM, Satter EK. JAAD Grand Rounds. A 53-year-old woman with multifocal subcutaneous nodules. J Am Acad Dermatol. 2015;72:924-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 32. | Miida H, Ito M. Cutaneous sarcoid with varied morphology associated with hypercalcaemia and renal impairment. Clin Exp Dermatol. 2009;34:e656-e659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 33. | Bianchini C, Tosin E, Ciorba A, Pelucchi S, Pastore A. Subcutaneous sarcoidosis: a rare involvement of the paralateral nasal region. Acta Otorhinolaryngol Ital. 2011;31:118-120. [PubMed] |
| 34. | Kerner M, Ziv M, Abu-Raya F, Horowitz E, Rozenman D. Subcutaneous sarcoidosis with neurological involvement: an unusual combination. Isr Med Assoc J. 2008;10:428-430. [PubMed] |
| 35. | Kim MH, Lee K, Kim KU, Park HK, Lee MK, Suh DS. Sarcoidosis mimicking cancer metastasis following chemotherapy for ovarian cancer. Cancer Res Treat. 2013;45:354-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 36. | Guccione JP, Holloway B, Guccione JL. Coalescing Subcutaneous Nodules. JAMA Dermatol. 2017;153:1319-1320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 37. | Meyer-Gonzalez T, Suarez-Perez JA, Lopez-Navarro N, Hidalgo A, Herrera-Ceballos E. Subcutaneous sarcoidosis: a predictor of systemic disease? Eur J Intern Med. 2011;22:e162-e163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Moscatelli S, Simonetti S, Bartoloni Bocci E, Gerli R. Unusual subcutaneous swellings on the hand as primary presenting feature of sarcoidosis. J Rheumatol. 2011;38:519-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Shigemitsu H, Yarbrough CA, Prakash S, Sharma OP. A 65-year-old woman with subcutaneous nodule and hilar adenopathy. Chest. 2008;134:1080-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 40. | Celik G, Ciledag A, Akin P, Simsek Y, Kaya A, Numanoglu N, Saglik YY, Boyvat A, Erekul S. Subcutaneous sarcoidosis with plantar involvement. Ann Dermatol. 2010;22:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Razek AA S-Editor: Cui LJ L-Editor: A E-Editor: Xing YX