Published online Jun 6, 2019. doi: 10.12998/wjcc.v7.i11.1323
Peer-review started: October 31, 2018
First decision: December 5, 2018
Revised: April 20, 2019
Accepted: May 11, 2019
Article in press: May 11, 2019
Published online: June 6, 2019
Processing time: 219 Days and 12.8 Hours
Uncovered stents used for malignant obstructions in the biliary tree, especially in the hilar area, are prone to obstruction by tumor ingrowths. In comparison, however, covered stents may block bile duct branches and are at risk of migration. We have developed a multi-hole self-expandable metallic stent (MHSEMS), with a hole in each cell, to prevent the obstruction of bile duct branches. In addition, the holes may prevent migration due to small ingrowths by reducing the tension of the membrane.
MHSEMS were placed in five patients with a malignant obstruction and one with post-endoscopic sphincterotomy bleeding. Each MHSEMS was successfully deployed in all cases. Patients showed no complications. Two cases were reviewed. Case 1: A 74-year-old male presented with jaundice and was diagnosed with a sigmoid colon cancer and giant liver metastases in the right liver lobe. A MHSEMS was placed in the left bile duct. The jaundice improved and peroral cholangioscopy was performed. Case 2: A 90-year-old female was admitted to hospital for jaundice and diagnosed with cholangiocarcinoma. A MHSEMS was placed in the left bile duct but after 8 months the stent became obstructed by tumor ingrowth. We treated the patient by ablation therapy. A silicone cover separated the internal bile duct from the surrounding tissue, protecting the latter from thermal injury during treatment by endobiliary ablation of the re-obstruction.
A MHSEMS is a new choice of stent for biliary tract diseases.
Core tip: We have developed a multi-hole self-expandable metallic stent (MHSEMS), with a hole in each cell, to prevent the obstruction of bile duct branches. In addition, the holes prevent migration due to small ingrowths by reducing the tension of the membrane. MHSEMS were placed in six patients. Each MHSEMS was successfully deployed with no complications in all cases. An ingrowth case was treated by electrical ablation therapy. Two cases were reviewed. We concluded that a MHSEMS is a new choice of stent for biliary tract diseases.
- Citation: Kobayashi M. Development of a biliary multi-hole self-expandable metallic stent for bile tract diseases: A case report. World J Clin Cases 2019; 7(11): 1323-1329
- URL: https://www.wjgnet.com/2307-8960/full/v7/i11/1323.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i11.1323
In biliary stenting, an uncovered self-expandable metallic stent (UCSEMS) is prone to occlusion due to tumor ingrowth[1-4]. In comparison, when using a covered self-expandable metallic stent (CSEMS) the side branches of hepatic ducts may become blocked, preventing bile juice flow and making it difficult for a stent to be placed in the hilar area. A specific CSEMS, known as a fully CSEMS (FCSEMS), also has a risk of migration[1-4]. Another type of stent, known as a partially covered SEMS (PCSEMS), was developed with the aim of lowering migration rates compared to CSEMS; how-ever, this is also difficult to place in the hilar area.
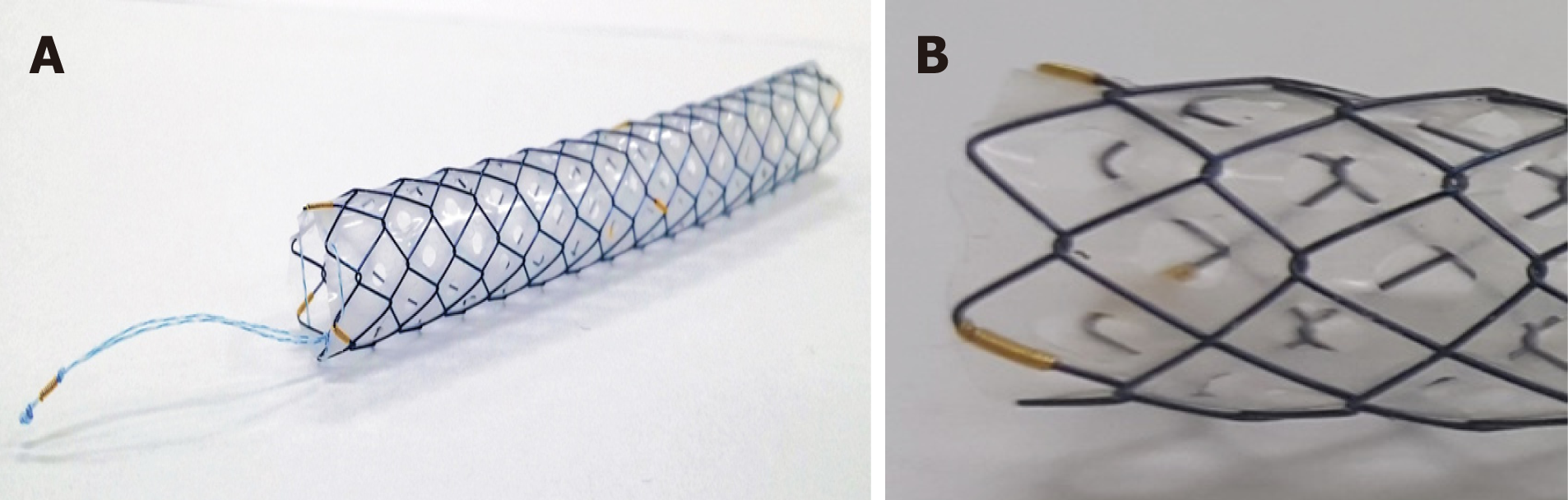
In order to resolve these problems, we, together with M.I.Tech Co., Ltd (Pyeong-taek, South Korea), have developed a multi-hole self-expandable metallic stent (MHSEMS; Figure 1) with numerous holes in its cover.
A MHSEMS has a hole in each stent cell on its covering membrane. When the stent is positioned in a junction connected by side branches, bile flows inside the stent through the holes in its covering membrane. Tumors may grow through these holes but may become suppressed due to the size of the ingrowth. As a result of low membrane tension caused by the holes, the placed stent becomes fixed to surrounding tissues and is prevented from migrating. Presently, the MHSEMS is available with two types of hole sizes: small (Figure 1A) and large (Figure 1B).
In addition, a lasso attached to the distal end of the MHSEMS (Figure 1A) is helpful for stent removal. Even if an obstruction by a tumor ingrowth does occur, the silicone cover will protect the surrounding tissue and enhance any ablation effect, such as during endobiliary radiofrequency ablation (RFA), allowing the patient to be a candidate for such treatment. We treated patients with malignant biliary obstruction using MHSEMS.
Chief complaints: A 74-year-old male presented to our hospilal with jaundice and liver function failure.
History of present illness: The patient had attended the outpatient department of another hospital, and liver dysfunction was identified in a regular check-up.
History of past illness: The patient had a medical history of diabetes and benign prostatic hypertrophy.
Personal and family history: A personal or family history of malignant tumors did not exist.
Physical examination upon admission: On physical examination, icterus of the patient’s conjunctiva was observed. An enlarged liver was palpable in the upper right quadrant. The skin and bulbar conjunctiva were icteric.
Laboratory examinations: The laboratory findings on admission were as follows: Aspartate trans-aminase (AST) 73 IU/L, alanine aminotransferase (ALT) 61 IU/L, alkaline phosphatase (ALP) 1962 IU/L, gamma-glutamyl transpeptidase (γ-GTP) 704 IU/L, total bilirubin (T-bil) 8.8 mg/dL, direct bilirubin (D-bil) 5.1 mg/dL, carci-noembryonic antigen (CEA) 1117.1 ng/mL and carbohydrate antigen 19-9 (CA19-9) 32 U/mL.
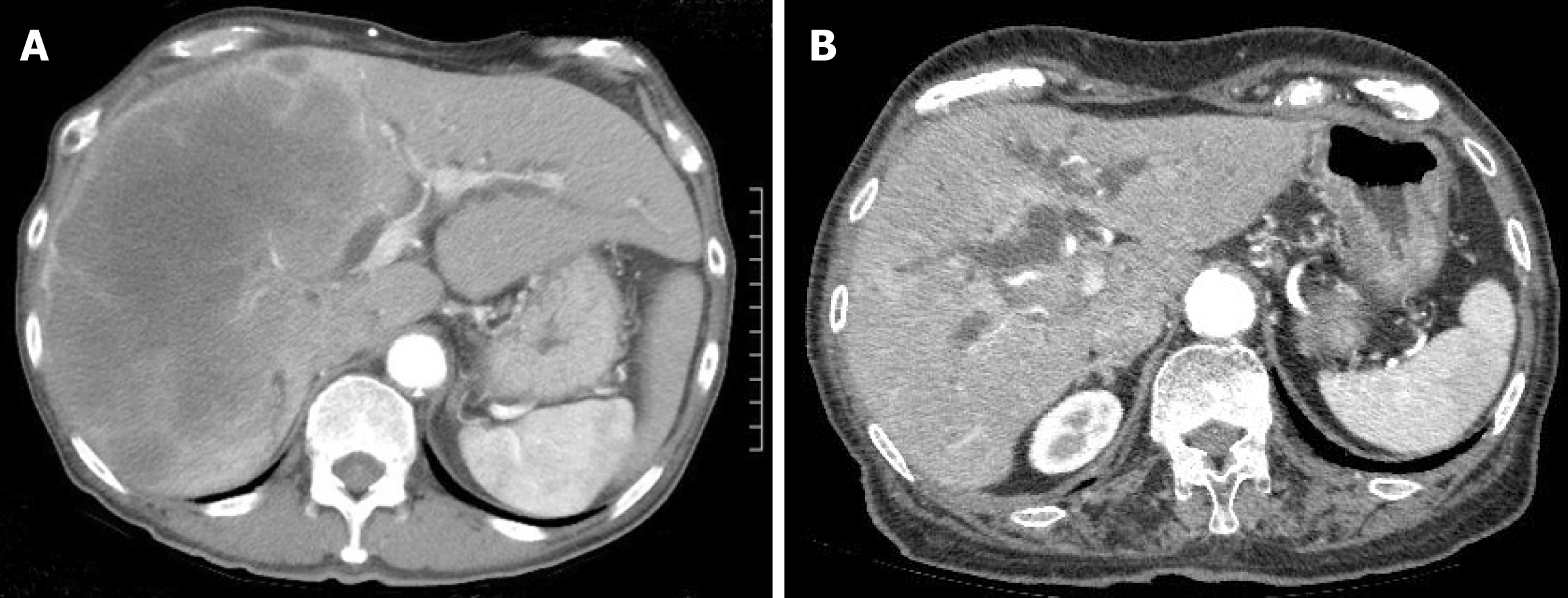
Imaging examinations: Computed tomography (CT) of the abdomen revealed a sigmoid colon tumor and multiple liver metastases, including a right liver lobe that was almost totally occupied by tumors; the left intrahepatic bile duct was remarkably dilated (Figure 2A).
Chief complaints: A 90-year-old female was referred to our hospital by the family doctor because of jaundice.
History of present illness: The patient did not have a history of jaundice.
History of past illness: The patient had a past history of hypertension.
Personal and family history: But she had no personal or family history of malignant tumors.
Physical examination upon admission: On physical examination, the patient’s skin was icteric. A large gall bladder was palpable in the upper right quadrant.
Laboratory examinations: AST 371 IU/L, ALT 418 IU/L, ALP 4273 IU/L, γ-GTP 1367 IU/L, T-bil 9.6 mg/dL, D-bil 6.3 mg/dL, CEA 1.5 ng/mL and CA19-9 39 U/mL.
Imaging examinations: An intrahepatic biliary dilation was detected by compu-terized tomography (Figure 2B).
The patient was diagnosed with obstructive jaundice caused by a sigmoid colon cancer and multiple liver metastases.
The patient was diagnosed with obstructive jaundice caused by hilar cholangio-carcinoma.
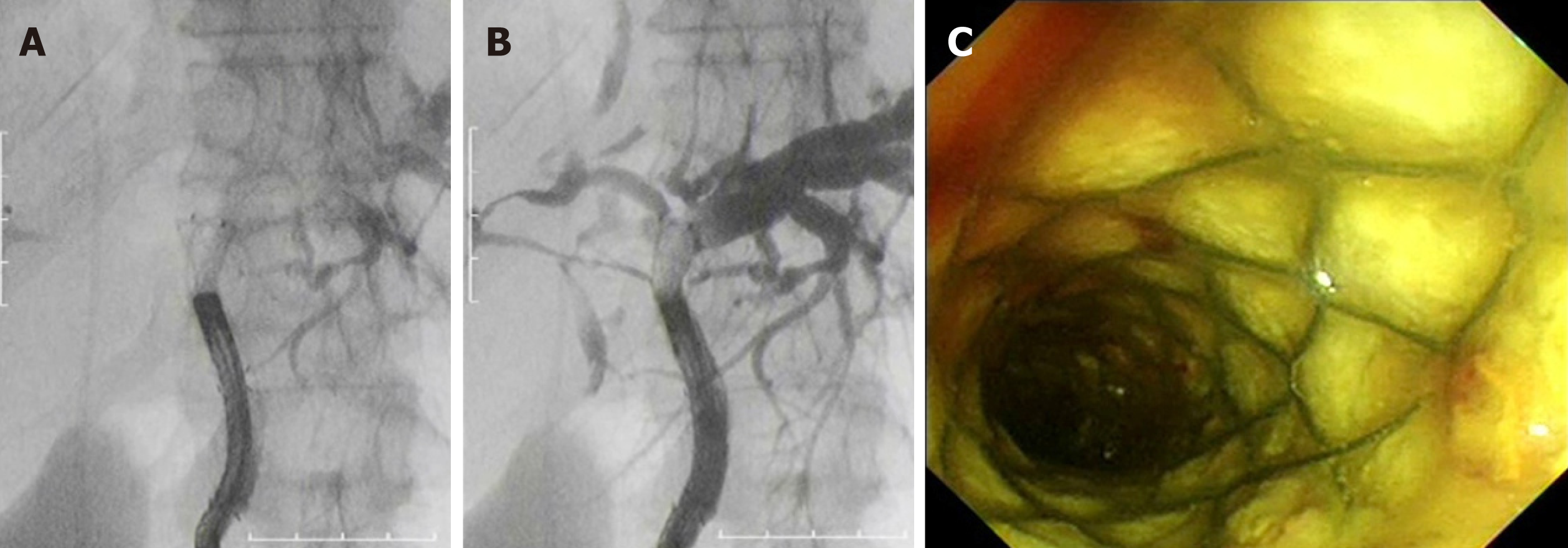
We selected MHSEMS to keep the left bile duct free from invasion by the right lobe tumor, the presence of the latter meaning the right liver lobe was not functioning (Figure 2A). A MHSEMS was placed from the left bile duct to the common bile duct (CBD; Figure 3A and B).
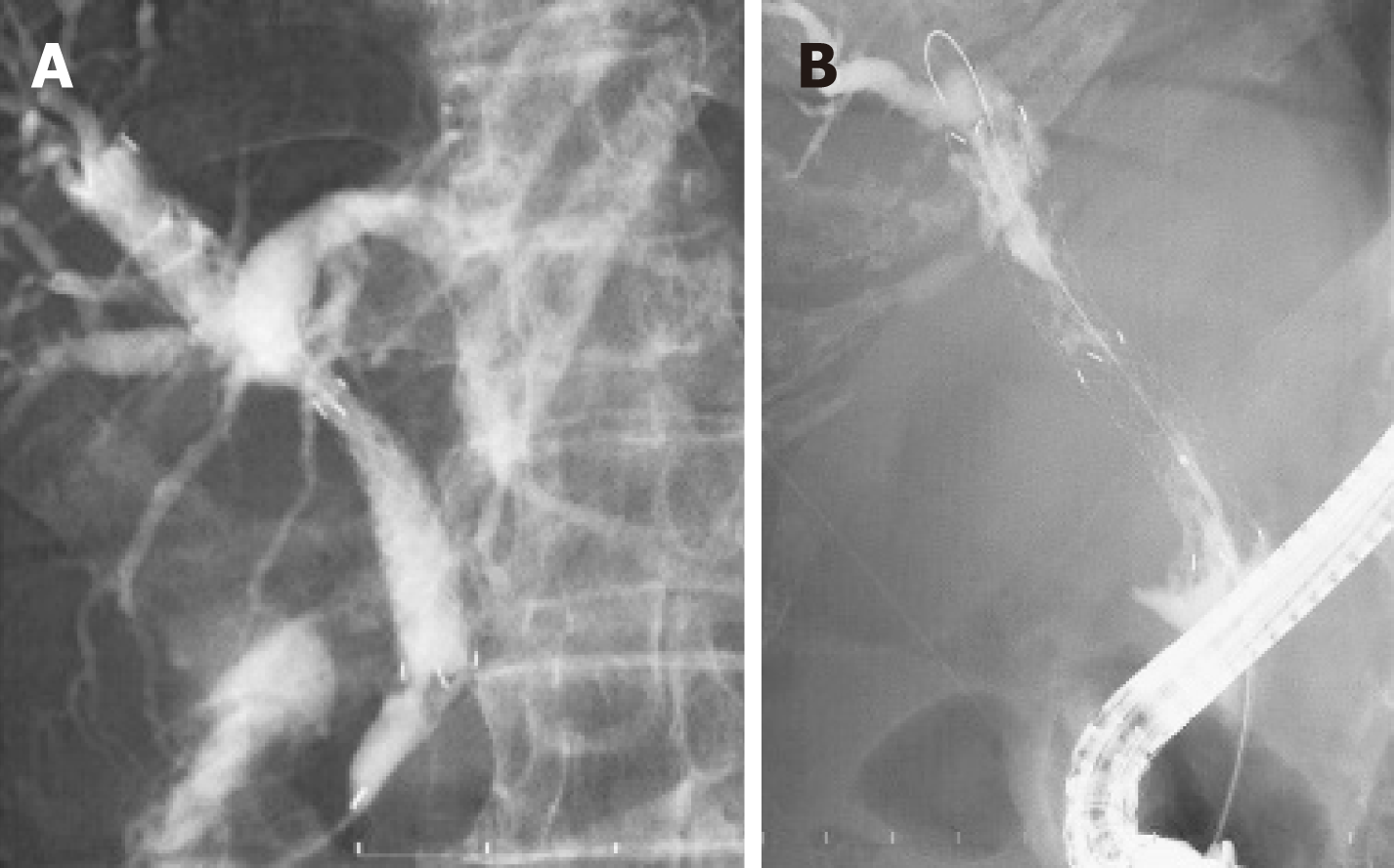
We selected a MHSEMS because of an expectation of reduced tumor ingrowth. The patient had a MHSEMS placed from the right hepatic duct to the common bile duct to protect the duct from ingrowth and to keep the bile duct patent from left and posterior branches (Figure 4A).
After MHSEMS placement, T-bil decreased from 11.9 mg/dL to 1.3 mg/dL. Nine days after stent placement, cholangiography was undertaken using a direct peroral cholangioscope with a slim endoscope. An intrahepatic bile duct branch was successfully filled with contrast material from a slim endoscope through the stent’s holes. The metallic mesh was found not to be buried in tissue but was fixed to the wall because of the low tension of the covering membrane (Figure 3C). Thirty-six days after MHSEMS placement, the patient died due to cancer. However, the total bilirubin level had been kept almost within normal range after stent placement.
After MHSEMS placement, T-bil decreased from 9.6 mg/dL to 1.1 mg/dL. However, after 8 mo, the stent became obstructed by tumor ingrowth. We treated the patient by ablation therapy and a monopolar catheter (Figure 4B). After ablation therapy, a tube stent was placed and liver function improved. The patient was transferred to another hospital in order to receive palliative medicine.
Most biliary stents may be broadly classified into two types: UCSEMS and CSEMS. An UCSEMS can be placed in a hilar lesion, but has a risk of ingrowth. In contrast, the use of a CSEMS has the disadvantage of the chance of branch obstruction occurring. Another type of stent, a PCSEMS, may reduce the risk of migration; however, it is also unusable in the hilar region. To date, these have been the main types of stents avai-lable for the treatment of biliary strictures.
In various meta-analyses undertaken, little difference was observed between the use of UCSEMS and CSEMS in terms of stent failure and patient mortality. However, stent ingrowth and migration rates differed for these two types of biliary stents. The rate of tumor ingrowth for UCSEMS was significantly higher than the rate for CSEMS. In contrast, the stent migration rate was higher for CSEMS compared with UCSEMS. In addition, meta-analyses revealed a lack of difference in the overall complication rate[1-4]. Overall estimates by meta-analyses also revealed a lack of substantial difference between FCSEMS and PCSEMS[1]. Compared to UCSEMS, PCSEMS did not prolong stent patency in unresectable malignant distal biliary obstructions[5]. Identifying a need for a new type of stent, we therefore collaborated with M.I.Tech to develop a MHSEMS. This stent has many holes in its cover designed to prevent not only blockage of bile duct branches, but also stent migration.
We treated six cases showing bile duct obstructions with MHSEMS, and had a 100% success rate for stent deployment (Table 1). Stent patency was also 100% successful (Table 1). In addition, jaundice improved in all patients with a malignant stricture, while complications such as pancreatitis, bleeding and cholangitis did not occur. The mean patency duration was found to be 274 d.
| Case No. | Age (yr)/sex | Diagnosis | Obstruction region | Migration | Occlusion | Ingrowth | Removal | Pancreatitis |
| 1 | 74/M | Liver metastasis of colon carcinoma | Hilar bile duct | No | No | Not clear | N/A | No |
| 2 | 89/F | Cholangiocarcinoma | Hilar bile duct | No | 249 d | Yes | N/A | No |
| 3 | 86/M | Cholangiocarcinoma | Hilar bile duct | No | 329 d | Yes | N/A | No |
| 4 | 48/M | Gall bladder carcinoma | Hilar bile duct | No | 295 d | Yes | N/A | No |
| 5 | 82/M | Pancreas head carcinoma | Distal bile duct | No | 223 d | Slight | Successful | No |
| 6 | 74/M | Post-endoscopic sphincterotomy bleeding | Distal bile duct | No | No | Slight | Successful (2 wk later) | No |
The MHSEMS has been designed with a lasso at its distal end for removability. In the event of the stent obstructing a bile duct branch and causing cholangitis, it can be removed very early after placement because the cover prevents the stent from becoming buried in tumor tissue.
In cases of benign strictures, the MHSEMS can also be easily removed. For example, MHSEMS were inserted in six mini pigs with artificial hilar biliary strictures; after 4 wk, all stents were easily and safely taken out[6]. For one of our studied cases, a MHSEMS was used for uncontrolled post-endoscopic sphincterotomy bleeding and was safely removed after 2 wk.
It is thought that endobiliary RFA is safe and has efficacy for unresectable malignant bile duct obstructions[7,8]. Pertinently, the successful and safe use of UCSEMS for occlusive endobiliary RFA has been reported[9,10]. With the use of MHSEMS, endobiliary RFA may become an even more effective and secure treatment since the insulated silicone cover can protect surrounding tissue from thermal injury.
The larger hole size of the MHSEMS is characteristic of an UCSEMS, but the smaller hole size and number is more typical of a CSEMS. With regard to preventing migration and ingrowth in a distal bile duct malignant stricture, it may be that the hole size and number need to be reduced. It would be ideal if hole size and number are adapted to the condition of each stricture.
In summary, MHSEMS may be considered a hybrid-type stent, with characteristics that fall between those of UCSEMS and CSEMS. Thus, MHSEMS may be regarded as a promising new treatment option for benign and malignant bile duct strictures.
| 1. | Tringali A, Hassan C, Rota M, Rossi M, Mutignani M, Aabakken L. Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: a systematic review and meta-analysis. Endoscopy. 2018;50:631-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 95] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 2. | Moole H, Bechtold ML, Cashman M, Volmar FH, Dhillon S, Forcione D, Taneja D, Puli SR. Covered versus uncovered self-expandable metal stents for malignant biliary strictures: A meta-analysis and systematic review. Indian J Gastroenterol. 2016;35:323-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Almadi MA, Barkun AN, Martel M. No benefit of covered vs uncovered self-expandable metal stents in patients with malignant distal biliary obstruction: a meta-analysis. Clin Gastroenterol Hepatol. 2013;11:27-37.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 148] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 4. | Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011;74:321-327.e1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 195] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 5. | Kim JY, Ko GB, Lee TH, Park SH, Lee YN, Cho YS, Jung Y, Chung IK, Choi HJ, Cha SW, Moon JH, Cho YD, Kim SJ. Partially Covered Metal Stents May Not Prolong Stent Patency Compared to Uncovered Stents in Unresectable Malignant Distal Biliary Obstruction. Gut Liver. 2017;11:440-446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Park JS, Jeong S, Kobayashi M, Sung W, Don HL. Efficacy, and removability of a fully covered multi-hole metal stent in a swine model of hilar biliary stricture: A feasibility study. Endosc Int Open. 2019;7:e498-e503. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Steel AW, Postgate AJ, Khorsandi S, Nicholls J, Jiao L, Vlavianos P, Habib N, Westaby D. Endoscopically applied radiofrequency ablation appears to be safe in the treatment of malignant biliary obstruction. Gastrointest Endosc. 2011;73:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 230] [Article Influence: 15.3] [Reference Citation Analysis (1)] |
| 8. | Alvarez-Sánchez MV, Napoléon B. Review of endoscopic radiofrequency in biliopancreatic tumours with emphasis on clinical benefits, controversies and safety. World J Gastroenterol. 2016;22:8257-8270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Yoon WJ, Kim YT, Daglilar ES, Mino-Kenudson M, Brugge WR. Evaluation of bipolar radiofrequency ablation for occluded self-expandable metal stents in the bile duct: in vivo and in vitro study. Endoscopy. 2015;47:1167-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Betgeri S, Rajesh S, Arora A, Panda D, Bhadoria AS, Mukund A. Percutaneous endobiliary RFA combined with balloon-sweep for re-opening occluded metallic biliary stents. Minim Invasive Ther Allied Technol. 2017;26:124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kwon CI, Yan SL S-Editor: Ma RY L-Editor: A E-Editor: Wang J