Published online Jan 6, 2019. doi: 10.12998/wjcc.v7.i1.79
Peer-review started: November 1, 2018
First decision: November 16, 2018
Revised: November 26, 2018
Accepted: November 30, 2018
Article in press: December 1, 2018
Published online: January 6, 2019
Processing time: 64 Days and 17.9 Hours
The complex anatomy of the maxillary first molars has always been a major challenge for complete root canal treatment in endodontic therapy. Here, we present two cases of maxillary first molars, each with only two root canals, which have been rarely reported. We also perform a literature review of maxillary first molar anatomy.
The two patients were referred to the hospital after 1) finding a cavity in their tooth with a color change and, 2) a toothache during mastication, respectively. Both of these cases were diagnosed as apical periodontitis by X-ray imaging and cone beam computed tomography (CBCT). Non-surgical endodontic therapy was performed with the assistance of a dental operating microscope (DOM). CBCT showed rare but accurate images of both patients, each with two root canals and two roots in their maxillary first molars. Both roots were located in the buccal in the palatal direction, and each root had only one clear root canal. In addition, each maxillary first molar in both patients was symmetrical to that on the opposing side with only two separate root canals. Non-surgical endodontic therapy was performed with the assistance of a DOM. Finally, the teeth were restored using composite resin and the patients were satisfied with the results.
Making full use of CBCT and DOM would contribute to helping dentists make correct diagnoses and successfully treat teeth with rare root canal morphologies.
Core tip: We describe two rare cases of maxillary first molars with only two separate root canals. An additional impressive finding was that the left and right sides were symmetrical, which extend the range of knowledge on both roots and root canals in relation to permanent maxillary first molar anatomy. Advanced surgical facilities and diagnostic methods, such as cone beam computed tomography and dental operating microscopy, play an important role in the diagnosis and treatment of these endodontic diseases and facilitate a better understanding of complicated root canal treatment.
- Citation: Liu J, Que KH, Xiao ZH, Wen W. Endodontic management of the maxillary first molars with two root canals: A case report and review of the literature. World J Clin Cases 2019; 7(1): 79-88
- URL: https://www.wjgnet.com/2307-8960/full/v7/i1/79.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i1.79
In-depth knowledge of the internal anatomy of the root canal system is mandatory for successful endodontic therapy[1]. The anatomy and morphology of roots and root canals vary greatly. Among all of the permanent teeth, maxillary first molars have the highest rates of root canal therapy failure in clinical practice[2,3] because of associated complexities and anatomic variations[4,5]. The number of roots in maxillary first molars detected by endodontics and general dentists ranges from one to five, according to the literature[6-9]. The number of root canals has been reported to range between one to eight[7-9], and even a C-shaped root canal has been observed[6,10-13]. Over 95% of maxillary first molars have three roots[14] and most have three to four root canals[15]. However, attention should be paid to fewer roots and root canal variations to identify the root canal system in the case of clinical failure, such as perforations.
Contemporary root canal treatment requires accurate knowledge of root canal anatomy and highly specialized facilities and materials. Currently, advanced techniques including cone beam computed tomography (CBCT) are widely used in endodontic treatment to provide three-dimensional images of the tooth. This has become an important tool both for diagnosis and planning dental treatment, including endodontic treatments[16,17,18], as well as in the assessment of anatomic findings such as isthmus and lateral canals, leading to more predictable and effective treatments[19]. A dental operating microscope (DOM) also increases the success rate of difficult treatment, as it provides a better operating field. The patients described in this report were diagnosed and treated with the assistance of CBCT and DOM, and both of them had maxillary first molars with a special root canal anatomy of two roots and two root canals, which has seldom been reported. These cases were intended to reinforce clinician awareness of the rare morphology of root canals.
In case 1, the patient’s chief complaint was a cavity and color change in her maxillary molar on the left side for approximately 2 mo. In case 2, the patient’s chief complaint was a toothache during mastication in the maxillary right posterior region for more than 1 wk.
In case 1, the patient found a cavity in the maxillary molar on the left side that was accompanied with discoloration 2 mo prior. The tooth was insensitive to cold and heat, and had no spontaneous pain nor cold or heat stimulation pain. The patient sometimes felt uncomfortable when chewing. In case 2, the patient felt an obvious toothache during mastication in the maxillary right posterior region for more than 1 wk. The tooth was insensitive to cold and heat, had no spontaneous pain nor cold or heat stimulation pain, and was not loose. The tooth and its periodontal tissue had never before been swollen.
None in case 1. In case 2, the patient had undergone root canal treatment in the right posterior tooth several years prior. The patient had no tooth extraction or orthodontic history.
In case 1, clinical examination revealed a cavity due to deep caries in the left maxillary molar and an exposed pulp cavity without pain. The tooth was sensitive to percussion and the periodontal tissue was swollen, but the tooth was not loose. In case 2, clinical examination revealed a metal crown and pain on vertical percussion in tooth 16. A buccally periodontal pocket approximately 6 mm was detected in tooth 16, which suggested an unhealthy periodontal condition.
In case 1, a preoperative X-ray image showed obvious low density in the distal area of tooth decay. The CBCT images clearly showed that this maxillary first molar had only two roots and two root canals, and that the root canals were located in the buccal-palatal direction and were separated from one another within each root. In case 2, a preoperative intraoral periapical radiograph revealed a maxillary first molar with an unsatisfactory root canal filling, with two roots and an obvious low-density image around the periapical area, thus indicating severe inflammation. CBCT showed that both of the patient’s maxillary first molars had only two roots and root canals, buccal and palatal, as seen in case 1.
Case 1: A 63 year old woman was referred to the Endodontic Department of Stomatology Hospital of Tianjin Medical University. The patient’s chief complaint was a cavity and color change in her maxillary molar on the left side for approximately 2 mo. Her medical history was noncontributory and the patient denied any tooth extractions or orthodontic history. Clinical examination revealed a cavity due to deep caries in the left maxillary molar and exposed pulp cavity without pain. The tooth was sensitive to percussion and the periodontal tissue was swollen. The diagnosis was deep caries with apical periodontitis in tooth 26. Endodontic therapy was proposed and accepted. Written informed consent was obtained from the patient.
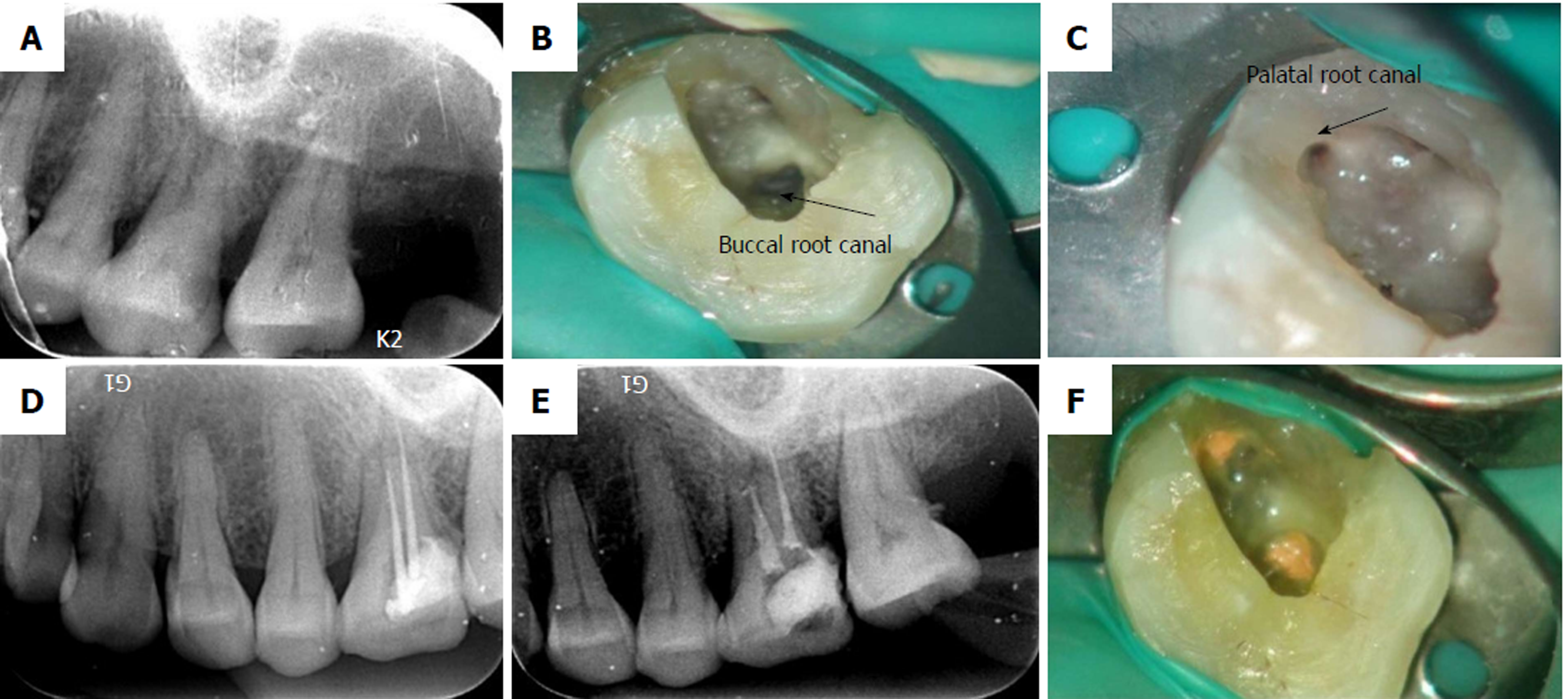
A preoperative X-ray image was obtained before surgery (Figure 1A). It showed obvious low density in the distal area of tooth decay. Isolation of the tooth using a rubber dam was carried out during the entire procedure. The pulp chamber was localized, and the access opening was expanded from the palate distally to the center of the tooth after removal of the decay. When the access opening was completed, an anatomic variation was seen on the pulp chamber floor (Figure 1B and C). Under the DOM visual field, only one buccal canal orifice and one palatal canal orifice were detected. Further inspection of the pulpal floor revealed the absence of other canal orifices. The pulp tissue in the chamber and two root canals were extirpated, and the canals were flooded with 3% sodium hypochlorite (Beyond Technology Corp., Beijing, China). The cavity was temporarily sealed with zinc oxide. As the X-ray did not reveal the condition of the root canal system, the patient underwent CBCT to acquire the three-dimensional (3D) morphology of the tooth.
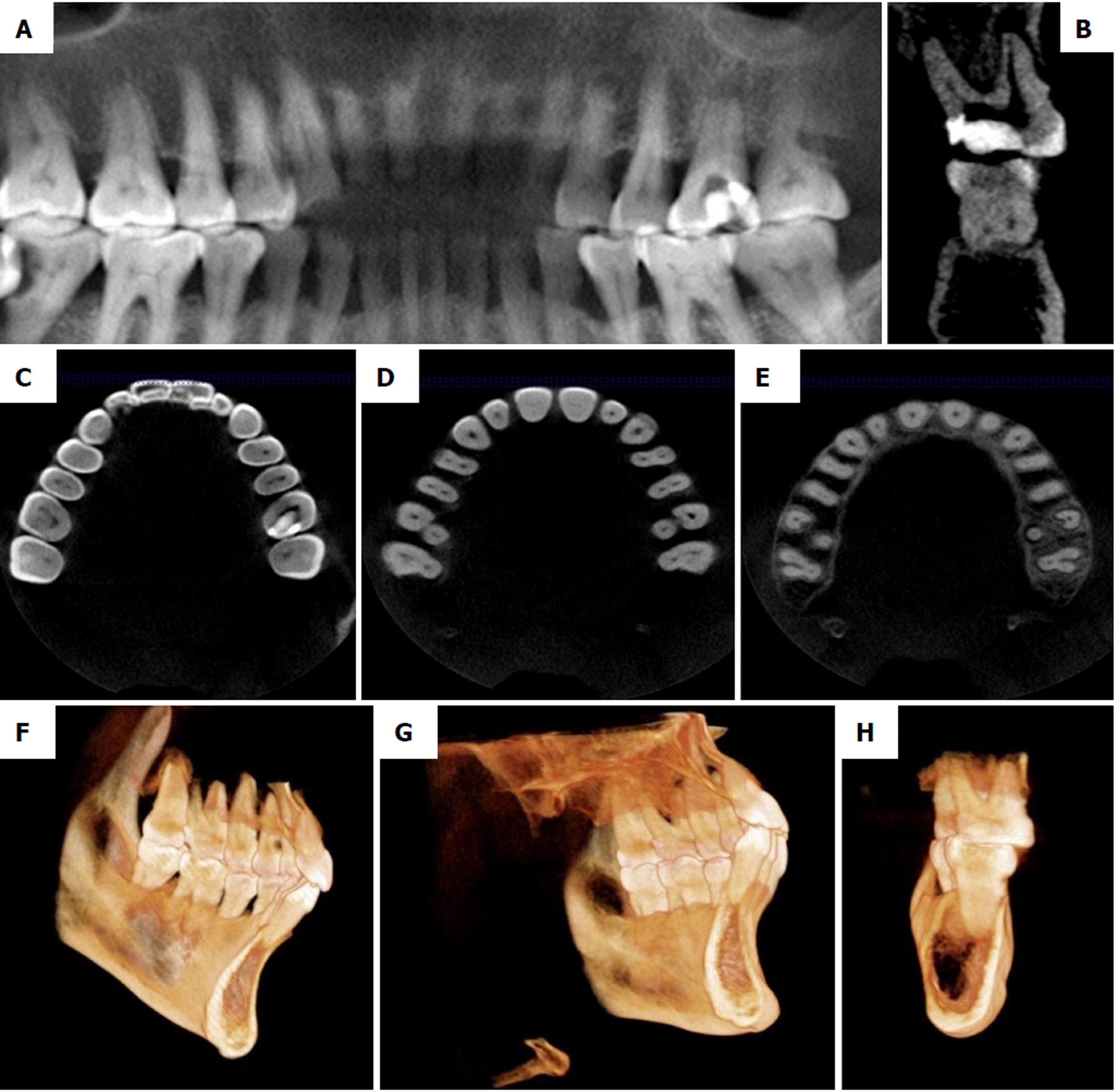
When the 3D images were obtained, longitudinal and cross-sections of 0.5 mm thickness were analyzed (Figure 2A-E). The CBCT images clearly showed the anatomical variation in the maxillary first molar of the patient with only two roots and two root canals. As seen from the 3D-reconstruction of the patient’s maxillary first molar, the root canals were located in the buccal-palatal direction and were separated from one another within each root (Figure 2F-H), which was in accordance with the DOM examination.
When the canals had been confirmed, the working length was measured and confirmed by an electronic apex locator (Morita Corporation, Kyoto, Japan). The root canals were shaped by Ni-Ti rotary instrumentation (M3, United Dental, Shanghai, China), irrigated with 1% sodium hypochlorite (Beyond Technology Corp., Beijing, China) and 0.9% sodium chloride (China Otsuka Pharmaceutical Co., Ltd., China), obturated by gutta-percha using the thermafil obturation technique step by step with the assistance of DOM, and then confirmed by X-ray imaging (Figure 1D-F). The tooth was finally restored using composite resin and the patient was satisfied with the results.
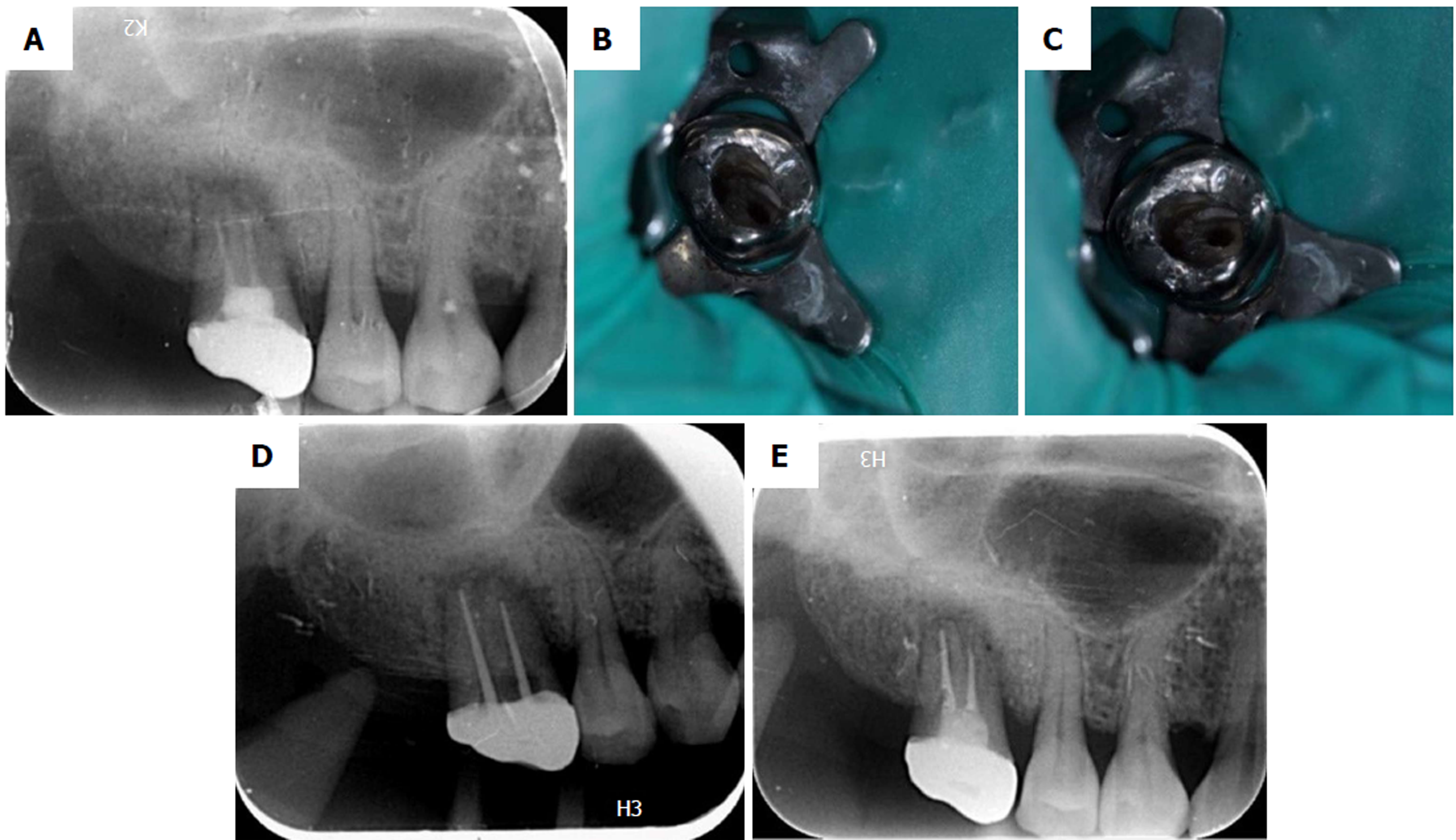
Case 2: A 45 year old female presented to the Endodontics Department of Stomatology Hospital of Tianjin Medical University with the complaint of a toothache during mastication in the maxillary right posterior region for more than 1 wk. Both second maxillary molars were missing and the patient denied tooth extraction or orthodontic history. However, she had undergone root canal treatment in the right posterior tooth several years previously. Clinical examination revealed a metal crown and pain on vertical percussion in tooth 16. A buccally periodontal pocket approximately 6 mm was detected in tooth 16, which suggested an unhealthy periodontal condition. The patient’s medical history was noncontributory. A preoperative intraoral periapical radiograph revealed a maxillary first molar with an unsatisfactory root canal filling, with two roots and an obvious low-density image around the periapical area that indicated severe inflammation (Figure 3A). From the clinical and radiographic findings, a diagnosis of apical periodontitis was made, and re-root canal treatment was planned and accepted. Written informed consent was obtained from the patient. Access to the pulp cavity and root canal was achieved through the crown using the DOM. The former core and gutta-percha were removed, and only two separate root canals were detected (Figure 3B and C). In order to ensure the efficacy of treatment, CBCT was suggested to determine the number of root canals.
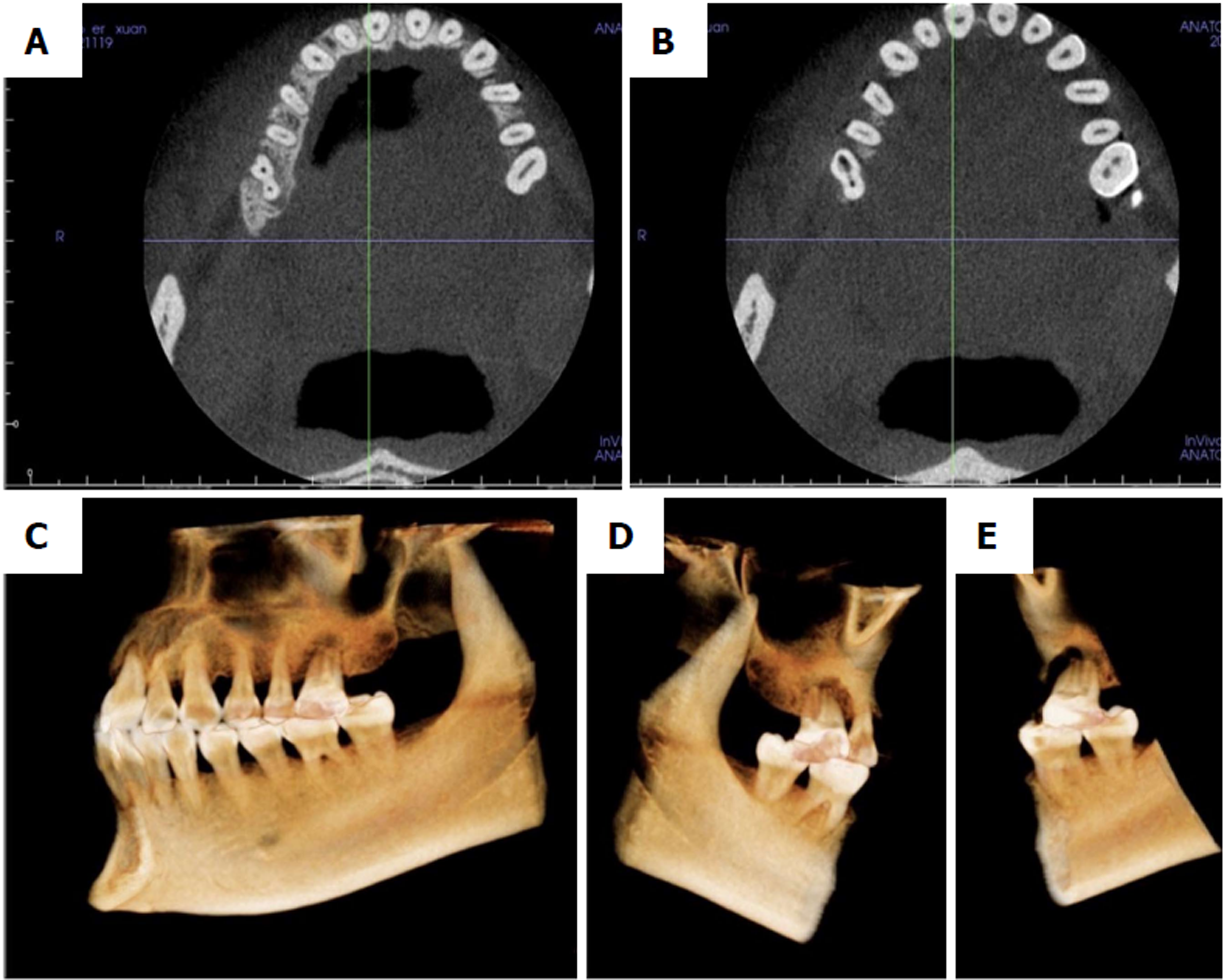
Based on the direct images as well as those reconstructed from CBCT, it was surprising to find that both of the patient’s maxillary first molars only had two roots and root canals, buccal and palatal, as seen in case 1 (Figure 4A-E). The re-root canal treatment was completed and confirmed by CBCT and DOM as in patient 1. Her pain was relieved after the first treatment, as shown by the patient’s subjective sensation. The root canals were filled with gutta-percha (Figure 3D-E) and the tooth was finally restored using composite resin.
It is significant that in both of these cases, the right maxillary first molars were symmetrical to the left maxillary first molars in their anatomical details. This has seldom been reported before and illustrates the condition of two root canals and two roots in both maxillary sides in these two patients.
Clinical examination revealed apical periodontitis in both patients.
Non-surgical endodontic therapy was performed with the assistance of a DOM.
The teeth were both finally restored using composite resin. The inflammation was controlled and the patients’ discomfort disappeared. The patients were both satisfied with the results.
The most common anatomy in maxillary first molars is three roots (96.2%) and three to four root canals (98.32%)[14,20,21]. Hence, the reports of variation in maxillary first molars mainly focus on the morphology of MB2 and the detection of multiple canals, while the two-rooted form of the maxillary first molar is rarely reported. Several previous studies in vitro, such as clearing, sectioning, or radiographic examination with radiopaque gel infusion of canals, have shown that the incidence of maxillary first molar with only two roots varies from 0 to 6.3%[14,22-23]. To date, there is only one report in the literature of one single buccal root and one single palatal root, which should be emphasized to avoid treatment errors[24]. In the present report, the patients’ CBCT images showed that the two roots were isolated from one another. One was the buccal root and the other was the palatal root. The two root canals opened from the same chamber and had their own apex.
In our cases, the buccal root was more likely to be C-shaped, while the root canal was straight without morphological changes. When a tooth shows only one buccal root, it is possible that the tooth indeed has only one buccal root or that two buccal roots have fused into a stronger root[25]. This may be caused by non-fused or non-divided roots that were established during the root’s embryologic stages[26]. The Hertwig horizontal root sheath is supposed to retain the shape of the root. When the epithelium is inadequately developed, the inadequate Hertwig sheath may promote the C-shaped canals seen in our patients.
In maxillary first molars, fusion may be divided into three types: fusion of the distobuccal (DB) root with the palatal (P) root (Type A), fusion of the mesiobuccal (MB) root and the distobuccal root (Type B), and fusion of two palatal roots (Type C)[6]. We performed an extensive review of available reports about maxillary first molars with fewer root canals and C-shaped root canals (Table 1). As the table showed, the majority of fusion occurred between DB and P roots (Type A), and MB and DB roots (Type B), with a lower incidence of the fusion of two P roots, which is referred to as Type C.
| Ref. | Country | Gender | Ethnicity | No. of canals | Features of the root canals | Type | Symmetry or not |
| Newton et al[13] | United States | Male | White | 2 | Fusion between P and DB canals, and a single MB canal | Type A | N/A |
| Dankner et al[27] | Israel | Female | White | 3 | Fusion between P and DB canals, and a single MP canal | Type A | Yes |
| Fava et al[8] | Brazil | Female | N/A | 3 | Fusion between MB and DB, but with 2 root canal apexes, and a single C-shaped P canal | Type B | N/A |
| De Moor et al[33] | Belgium | Female | White | 3 | Fusion between P and DB canals, and single MB, MP canals | Type A | N/A |
| De Moor et al[33] | Belgium | Male | White | 2 | Fusion between P and DB canals, and a single MB canal | Type A | No |
| Gopikrishna et al[7] | India | N/A | 1 | A single root with 1 root canal | / | N/A | |
| Yilmaz et al[28] | Turkey | Female | White | 2 | Fusion between MB and DB canals, but with 3 foramina, and a single P canal | Type B | N/A |
| Ma et al[24] | China | Female | Yellow | 2 | Fusion between MB and DB canals, and a single P canal | Type B | Yes |
| Kottoor et al[11] | India | Male | N/A | 4 | Fusion between 2 P canals, and single MB, DB canals | Type C | No |
| Martins et al[6] | Portugal | Male | White | 2 | Fusion between P and DB canals, and a single MB canal | Type A | Yes |
| Martins et al[6] | Portugal | Female | White | 2 | Fusion between MB and DB canals, and a single P canal | Type B | N/A |
| Shin et al[29] | Korea | Male | Yellow | 1 | All the roots fuse together into one O-shaped root, but 5–6 root canals with connecting fins at the apical 3mm | O-shaped | Yes |
| Joshi et al[30] | India | female | N/A | 1 | A single fused root with a single canal | / | Yes |
| Paksefat et al[31] | Iran | female | N/A | 3 | Fusion between MB and DB canals, and single separate P and MB2 canals | Type B | No |
| Present study (case 1) | China | Female | Yellow | 2 | Fusion between MB and DB canals, and a single P canal | Type B | Yes |
| Present study (case 2) | China | Female | Yellow | 2 | Fusion between MB and DB canals, and a single P canal | Type B | Yes |
In this study, according to the location of the root canals, fusion may have occurred between the MB and DB roots (Type B). The cases reported here may be the special condition of the C-shaped maxillary. Some studies have shown that C-shaped roots occur differently due to ethnic variation. In the white population, the incidence of C-shaped roots is reported to be 2.7%-7.6%[26], while the incidence in the Chinese population may be as high as 31.5%[32], which is very common and widely accepted in mandibular second molars. However, in maxillary first molars, it is still very rare to see a C-shaped root and root canal (approximately 0.12%)[2,33]. In the Chinese population with a high risk of C-shaped roots, it was reported that only 0.3% of extracted maxillary first molars had C-shaped roots[34]. In Europeans, the incidence is only 0.09%[33].
Plotino has reported that the percentage of symmetry in root and canal anatomy between left and right sides varied from 70%-81%[35]. Therefore, it was also interesting to find that the morphology of each maxillary first molar was symmetrical to that of the opposite side in our two cases. This symmetry is rare in the literature. In most patients, it is meaningful to check the tooth on the opposite side, which may have an essential guiding value for treatment of the opposite tooth.
It is extremely important that clinicians use all of the armamentarium at their disposal to locate and treat the entire root canal system[36]. The routine use of preoperative CBCT imaging with small fields of view could be recommended for both initial endodontic treatment and nonsurgical retreatment of maxillary molars[37]. On the other hand, DOM usage in daily clinical practice could also potentiate and facilitate the localization and handling of additional canals as a result of lighter and significantly higher magnification of the field of view[38,39]. Therefore, clinicians should be more aware of the morphological variations in permanent teeth to complete satisfactory root canal treatment with the help of techniques such as CBCT and DOM.
In conclusion, the permanent maxillary first molars with two root canals and two roots are rare and unusual clinical cases. In our patients with this rare condition, the left and right sides were symmetrical. Attention should be paid to patients with fewer root canals and root anatomical variations to overcome the fixed idea regarding the morphology of molars. Advanced surgical facilities and diagnostic methods such as DOM and CBCT can assist in diagnosis and modern root canal treatment.
| 1. | Estrela C, Holland R, Estrela CR, Alencar AH, Sousa-Neto MD, Pécora JD. Characterization of successful root canal treatment. Braz Dent J. 2014;25:3-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 164] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 2. | Christie WH, Peikoff MD, Fogel HM. Maxillary molars with two palatal roots: a retrospective clinical study. J Endod. 1991;17:80-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 87] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 3. | Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1000] [Cited by in RCA: 1144] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 4. | Lee KW, Kim Y, Perinpanayagam H, Lee JK, Yoo YJ, Lim SM, Chang SW, Ha BH, Zhu Q, Kum KY. Comparison of alternative image reformatting techniques in micro-computed tomography and tooth clearing for detailed canal morphology. J Endod. 2014;40:417-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (1)] |
| 5. | Briseño-Marroquín B, Paqué F, Maier K, Willershausen B, Wolf TG. Root Canal Morphology and Configuration of 179 Maxillary First Molars by Means of Micro-computed Tomography: An Ex Vivo Study. J Endod. 2015;41:2008-2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (1)] |
| 6. | Martins JN, Quaresma S, Quaresma MC, Frisbie-Teel J. C-shaped maxillary permanent first molar: a case report and literature review. J Endod. 2013;39:1649-1653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Gopikrishna V, Bhargavi N, Kandaswamy D. Endodontic management of a maxillary first molar with a single root and a single canal diagnosed with the aid of spiral CT: a case report. J Endod. 2006;32:687-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 65] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Fava LR. Root canal treatment in an unusual maxillary first molar: a case report. Int Endod J. 2001;34:649-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Barbizam JV, Ribeiro RG, Tanomaru Filho M. Unusual anatomy of permanent maxillary molars. J Endod. 2004;30:668-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Kottoor J, Velmurugan N, Sudha R, Hemamalathi S. Maxillary first molar with seven root canals diagnosed with cone-beam computed tomography scanning: a case report. J Endod. 2010;36:915-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 11. | Kottoor J, Velmurugan N, Surendran S. Endodontic management of a maxillary first molar with eight root canal systems evaluated using cone-beam computed tomography scanning: a case report. J Endod. 2011;37:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 12. | Martins JN, Anderson C. Endodontic treatment of the maxillary first molar with five root canals-three case reports. Rev Port Estomatol Cir Maxilofac. 2013;54:37-42. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Newton CW, McDonald S. A C-shaped canal configuration in a maxillary first molar. J Endod. 1984;10:397-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 14. | Cleghorn BM, Christie WH, Dong CC. Root and root canal morphology of the human permanent maxillary first molar: a literature review. J Endod. 2006;32:813-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 211] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 15. | Pécora JD, Woelfel JB, Sousa Neto MD, Issa EP. Morphologic study of the maxillary molars. Part II: Internal anatomy. Braz Dent J. 1992;3:53-57. [PubMed] |
| 16. | Special Committee to Revise the Joint AAE/AAOMR Position Statement on use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement: Use of Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:508-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 228] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 17. | Neelakantan P, Subbarao C, Subbarao CV. Comparative evaluation of modified canal staining and clearing technique, cone-beam computed tomography, peripheral quantitative computed tomography, spiral computed tomography, and plain and contrast medium-enhanced digital radiography in studying root canal morphology. J Endod. 2010;36:1547-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 191] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 18. | Jeger FB, Lussi A, Bornstein MM, Jacobs R, Janner SF. [Cone beam computed tomography in endodontics: a review for daily clinical practice]. Schweiz Monatsschr Zahnmed. 2013;123:661-668. [PubMed] |
| 19. | Venskutonis T, Plotino G, Juodzbalys G, Mickevičienė L. The importance of cone-beam computed tomography in the management of endodontic problems: a review of the literature. J Endod. 2014;40:1895-1901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Badole GP, Warhadpande MM, Shenoi PR, Lachure C, Badole SG. A rare root canal configuration of bilateral maxillary first molar with 7 root canals diagnosed using cone-beam computed tomographic scanning: a case report. J Endod. 2014;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Ghobashy AM, Nagy MM, Bayoumi AA. Evaluation of Root and Canal Morphology of Maxillary Permanent Molars in an Egyptian Population by Cone-beam Computed Tomography. J Endod. 2017;43:1089-1092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 22. | al Shalabi RM, Omer OE, Glennon J, Jennings M, Claffey NM. Root canal anatomy of maxillary first and second permanent molars. Int Endod J. 2000;33:405-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Thomas RP, Moule AJ, Bryant R. Root canal morphology of maxillary permanent first molar teeth at various ages. Int Endod J. 1993;26:257-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 91] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Ma L, Chen J, Wang H. Root canal treatment in an unusual maxillary first molar diagnosed with the aid of spiral computerized tomography and in vitro sectioning: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e68-e73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Jin GC, Lee SJ, Roh BD. Anatomical study of C-shaped canals in mandibular second molars by analysis of computed tomography. J Endod. 2006;32:10-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Marzioni D, Capparuccia L, Todros T, Giovannelli A, Castellucci M. Growth factors and their receptors: fundamental molecules for human placental development. Ital J Anat Embryol. 2005;110:183-187. [PubMed] |
| 27. | Dankner E, Friedman S, Stabholz A. Bilateral C shape configuration in maxillary first molars. J Endod. 1990;16:601-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 41] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Yilmaz Z, Tuncel B, Serper A, Calt S. C-shaped root canal in a maxillary first molar: a case report. Int Endod J. 2006;39:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Shin Y, Kim Y, Roh BD. Maxillary first molar with an O-shaped root morphology: report of a case. Int J Oral Sci. 2013;5:242-244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Joshi C, Joshi S. C-shaped canal in maxillary first molars: a case report. J Dent (Tehran). 2014;11:111-117. [PubMed] |
| 31. | Paksefat S, Rahimi S. Root canal treatment of a two-rooted C-shaped maxillary first molar: a case report. Iran Endod J. 2014;9:301-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Yang ZP, Yang SF, Lin YC, Shay JC, Chi CY. C-shaped root canals in mandibular second molars in a Chinese population. Endod Dent Traumatol. 1988;4:160-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 82] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | De Moor RJ. C-shaped root canal configuration in maxillary first molars. Int Endod J. 2002;35:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Yang ZP, Yang SF, Lee G. The root and root canal anatomy of maxillary molars in a Chinese population. Endod Dent Traumatol. 1988;4:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Plotino G, Tocci L, Grande NM, Testarelli L, Messineo D, Ciotti M, Glassman G, D’ambrosio F, Gambarini G. Symmetry of root and root canal morphology of maxillary and mandibular molars in a white population: a cone-beam computed tomography study in vivo. J Endod. 2013;39:1545-1548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 36. | Patel B. Anatomy and Root Canal Morphology. Endodontic Diagnosis, Pathology, and Treatment Planning. Springer International Publishing. 2015;. |
| 37. | Studebaker B, Hollender L, Mancl L, Johnson JD, Paranjpe A. The Incidence of Second Mesiobuccal Canals Located in Maxillary Molars with the Aid of Cone-beam Computed Tomography. J Endod. 2018;44:565-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 38. | Sempira HN, Hartwell GR. Frequency of second mesiobuccal canals in maxillary molars as determined by use of an operating microscope: a clinical study. J Endod. 2000;26:673-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 71] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Görduysus MO, Görduysus M, Friedman S. Operating microscope improves negotiation of second mesiobuccal canals in maxillary molars. J Endod. 2001;27:683-686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 92] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
P- Reviewer: Zhou M, Maric I, Vieyra JP S- Editor: Dou Y L- Editor: Filipodia E- Editor: Bian YN