Published online Jan 6, 2019. doi: 10.12998/wjcc.v7.i1.69
Peer-review started: September 3, 2018
First decision: November 2, 2018
Revised: November 26, 2018
Accepted: December 12, 2018
Article in press: December 12, 2018
Published online: January 6, 2019
Processing time: 124 Days and 17.6 Hours
Diffuse fasciitis with psoriatic arthritis on magnetic resonance imaging (MRI) has not been previously described in childhood. Here we present the first case report of a pediatric patient developing fasciitis, beyond plantar fasciitis, with psoriatic arthritis.
An 11-year-old female was admitted with the complaints of psoriatic rash on the body associated with severe pain in the lower extremities and arthritis in the right knee. Psoriasis was confirmed by skin biopsy, she diagnosed with juvenile psoriatic arthritis. Diagnostic tests did not indicate any pathology except MRI. MRI of the femur and tibia revealed that high-signal inflammatory changes in the subdermal fascia. These findings led to a diagnosis of psoriatic fasciitis. Methotrexate was given for 3 mo but the patient showed no response to therapy; therefore, etanercept was added. However, there was no response to treatment. Etanercept was switched to adalimumab at the sixth month of therapy. Clinical improvement started with therapy of adalimumab within one month. Fasciitis finding in MRI disappeared at seventh months on adalimumab therapy. She has no complaint for two years with adalimumab.
The most effective imaging method is MRI and adalimumab may be the best choice of treatment for psoriatic fasciitis.
Core tip: Plantar fasciitis may be observed on magnetic resonance imaging (MRI) in patients with psoriatic arthritis. However, to our knowledge, MRI findings of diffuse fasciitis associated with psoriatic arthritis have not been previously described in a pediatric patient. Fasciitis should be considered in patients with psoriatic arthritis, especially with unresolved extremity pain. MRI seems to be the most effective imaging method and adalimumab may be the best choice of treatment for psoriatic fasciitis.
- Citation: Otar Yener G, Ekici Tekin Z, Yuksel S. Psoriatic fasciitis in a pediatric patient: A case report. World J Clin Cases 2019; 7(1): 69-72
- URL: https://www.wjgnet.com/2307-8960/full/v7/i1/69.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i1.69
Juvenile psoriatic arthritis (JPsA) is a rare disease characterized by psoriasis and arthritis in childhood. According to the International League of Associations for Rheumatology (ILAR) criteria, children with arthritis and psoriasis can be diagnosed with JPsA, as well as children presenting with arthritis and at least two of three features: dactylitis, nail changes, or psoriasis in a first-degree relative[1].
Plantar fasciitis may be observed on magnetic resonance imaging (MRI) in patients with psoriatic arthritis[2]. However, to our knowledge, MRI findings of diffuse fasciitis associated with psoriatic arthritis have not been previously described in a pediatric patient.
An 11-year-old female patient presented with psoriatic rash on the body associated with severe pain in the lower extremities and arthritis in the right knee.
She reported worsening pain in the legs for the past 6 mo that did not improve despite taking nonsteroidal anti-inflammatory drugs.
She had 1-year history of cutaneous rash on her extremities. Skin biopsy confirmed psoriasis and she was under treatment with topical steroids.
Her medical history was unremarkable except for psoriasis. There was no consanguineous marriage or family history of significant disease.
On physical examination, psoriatic rashes were observed on the extensor surfaces of the patient’s arms and legs. She had arthritis of the right knee and also, she reported myalgia associated with psoriatic rash in the lower extremities. Her vital signs were normal but weight was in the 90th-97th percentile range. Her vital signs were normal but weight was in the 90th-97th percentile range. Respiratory, cardiovascular, and gastrointestinal system examinations were normal. Eye examination performed by an ophthalmologist revealed no pathologies such as uveitis.
Laboratory results for complete blood account, complete urinalysis, acute-phase reactants, liver and renal function tests, serum complement (C3, C4), muscle enzymes (creatine kinase, lactate dehydrogenase, aspartate amino transferase), and antistreptolysin O were normal. All viral serological (Epstein-Barr virus, cytomegalovirus, hepatitis B and C, Toxoplasmosis, rubella, human immunodeficiency virus) and bacterial (Brucella, syphilis, Borrelia burgdorferi) tests were negative. Rheumatologic serological investigations investigations (ANA, HLA B27, Anti CCP and rheumatoid factor) were also negative. Genetic testing for autoinflammatory diseases revealed no pathology (MEFV, MVK, NLRP3, NLRC4, CASP10, CASP3, PSMB8, SLC29A3, CASP1, TNFRSF1A, PSTPIP1, PYCARD, NOD2, PLCG2, NLRP1, CARD8, NLRP12 genes were tested). Chest X-ray, echocardiography, abdominal ultrasound, and electroneuromyography were normal. A muscle biopsy revealed normal findings. In the absence of signs of other conditions included in the differential diagnosis, such as infection, malignancy, and autoinflammatory diseases, a diagnosis of JPsA was considered.
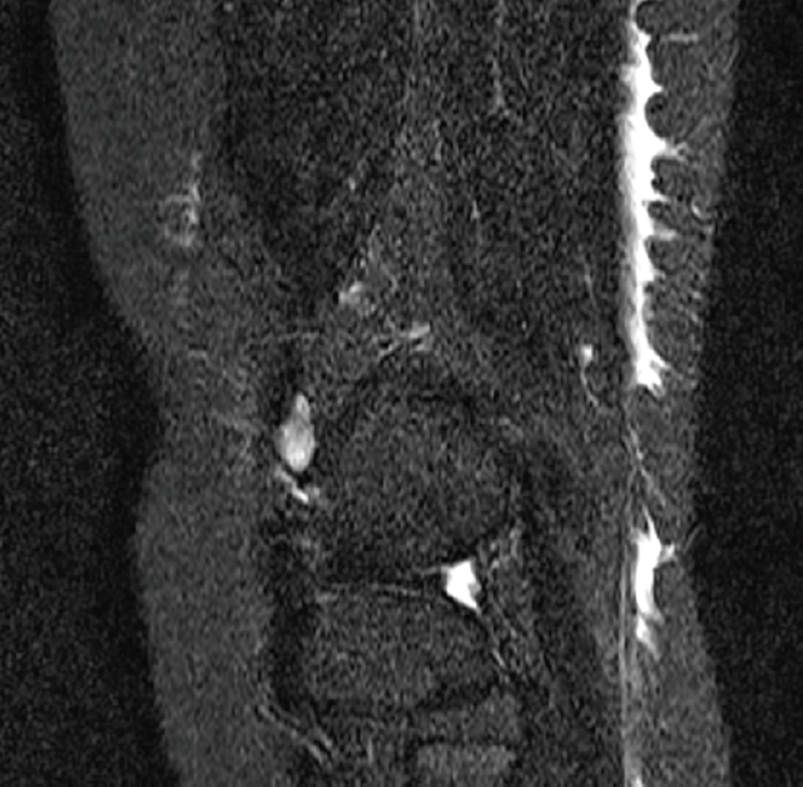
MRI was performed due to the patient’s severe lower extremity pain. T2-weighted images of the femur and tibia revealed high-signal inflammatory changes in the subdermal fascia (Figure 1).
The patient with arthritis and psoriasis was diagnosed with JPsA. All of these findings led to a final diagnosis of psoriatic fasciitis.
For treatment methotrexate (15 mg/wk) was given for 3 mo but the patient showed no response to therapy; therefore, etanercept (0.8 mg/kg per week) was added. However, there was no response to treatment. After 3 mo of etanercept treatment, the patient’s pain and skin eruptions persisted, so treatment was switched to adalimumab (40 mg every second week).
Clinical improvement started with therapy of adalimumab within one month. Significant clinical improvement was seen, with regression of the cutaneous lesions and resolution of the MRI findings after 7 months of the adalimumab treatment. After the therapy, she had no pain or rash in any of her extremities during the 2-year follow-up period.
Psoriasis is a common chronic inflammatory skin disease characterized by the development of erythematous skin and scar plaques. Children presenting with both arthritis and psoriasis or other psoriatic criteria may be diagnosed with JPsA[1]. Inflammation may involve a single joint or multiple joints, with or without involvement of the sacroiliac joints, the spinal column, or peripheral entheses. Dactylitis is a common manifestation in younger children, whereas axial arthritis and enthesitis are more common in older children[3]. And also, a current a report from GRAPPA emphasized that JPsA was usually presented with peripheral arthritis in early childhood, and late-onset JPsA was usually presented with enthesitis and axial arthritis features. Identification of these differences in classification is important to provide that late onset JPsA are successfully transferred from pediatric to adult care[4].
To our knowledge, this is the first report of a pediatric patient developing diffuse fasciitis with psoriatic arthritis. Bains et al[5] reported a 26-year-old adult patient with psoriatic arthritis who underwent fluorodeoxyglucose positron emission tomography-computed tomography imaging, which showed an uncommon imaging pattern with muscle and fascial involvement. In addition, two patients with psoriatic arthritis who had biopsy-proven eosinophilic fasciitis have been reported[6,7]. However, there was no peripheral eosinophilia in our patient and her muscle biopsy was normal.
Autoinflammatory disease with fasciitis, such as tumor necrosis factor receptor-associated periodic syndrome (TRAPS), has also been reported. Hull et al[8] presented a case of TRAPS associated with monocytic fasciitis in MRI examinations performed due to diffuse skin sensitivity and localized myalgia, similar to the clinical presentation of our case. They detected edematous changes in the muscle compartments and surrounding soft tissues of the left femur on MRI. Their pathologic examination revealed inflammation of the fascia and tendon comprising lymphocytes and macrophages along with tissue destruction, dissolution, and necrosis, while myofibers and endomysium were normal. The authors attributed their patient’s myalgia and rash to the distribution of inflammation throughout the fascial planes. Similarly, in our patient MRI revealed fasciitis corresponding to the region of arthralgia and muscle pain in the right knee. Our patient’s myalgia was due to fasciitis, but the biopsy showed no alterations in the muscle tissue.
In conclusion, psoriatic fasciitis presents its exceptionally unusual occurrence in a patient with JPsA. Fasciitis should be considered in patients with psoriatic arthritis, especially those with unresolved extremity pain. MRI seems to be the most effective imaging method and adalimumab may be the best choice of treatment.
| 1. | Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur AM, Suarez-Almazor ME, Woo P. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390-392. [PubMed] |
| 2. | Erdem CZ, Tekin NS, Sarikaya S, Erdem LO, Gulec S. MR imaging features of foot involvement in patients with psoriasis. Eur J Radiol. 2008;67:521-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Stoll ML, Zurakowski D, Nigrovic LE, Nichols DP, Sundel RP, Nigrovic PA. Patients with juvenile psoriatic arthritis comprise two distinct populations. Arthritis Rheum. 2006;54:3564-3572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Zisman D, Stoll ML, Butbul Aviel Y, Mellins ED. Juvenile Psoriatic Arthritis: A Report from the GRAPPA 2017 Annual Meeting. J Rheumatol Suppl. 2018;94:11-16. [PubMed] |
| 5. | Bains S, Reimert M, Win AZ, Khan S, Aparici CM. A Patient with Psoriatic Arthritis Imaged with FDG-PET/CT Demonstrated an Unusual Imaging Pattern with Muscle and Fascia Involvement: A Case Report. Nucl Med Mol Imaging. 2012;46:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Hariman R, Patel P, Strouse J, Collins MP, Rosenthal A. Development of Eosinophilic Fasciitis during Infliximab Therapy for Psoriatic Arthritis. Case Rep Rheumatol. 2016;2016:7906013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Wright GD, Thornton C, Keegan DA, Bell AL. Eosinophilic fasciitis presenting as psoriatic arthropathy. Ulster Med J. 1992;61:112-115. [PubMed] |
| 8. | Hull KM, Wong K, Wood GM, Chu WS, Kastner DL. Monocytic fasciitis: a newly recognized clinical feature of tumor necrosis factor receptor dysfunction. Arthritis Rheum. 2002;46:2189-2194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 57] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
P- Reviewer: Palmirotta R S- Editor: Ma RY L- Editor: A E- Editor: Bian YN