Published online Jul 16, 2018. doi: 10.12998/wjcc.v6.i7.156
Peer-review started: February 19, 2018
First decision: March 12, 2018
Revised: May 2, 2018
Accepted: May 30, 2018
Article in press: May 30, 2018
Published online: July 16, 2018
Processing time: 148 Days and 7.6 Hours
According to Klein’s classification system, the symptomatology of eosinophilic gastroenteritis (EG), a rare disease, differs based on the affected tissue layer. Patients with subserosal EG often have peritoneal effusion. Hemorrhagic ascites due to EG is extremely rare and has not been reported in the literature. Here, we report a 57-year-old woman with EG and massive hemorrhagic ascites. Laboratory investigations showed elevated peripheral eosinophils with significant eosinophilia (65.6%). Ultrasonography showed massive abdominal ascites. Abdominal paracentesis revealed hemorrhagic peritoneal fluid and microscopy showed predominant eosinophils. Upper gastrointestinal endoscopy revealed erosions, exudates, and mucosal rings in the duodenal mucosa; histological examination indicated eosinophilic infiltration. EG presenting with hemorrhagic ascites was diagnosed by histologic examination of eosinophilic infiltration. She was empirically treated with ketotifen 1 mg bid po with rapid resolution of ascites and a remarkable decline in peripheral eosinophil counts. Clinicians should consider the differential diagnosis of unexplained hemorrhagic ascites.
Core tip: Eosinophilic gastroenteritis (EG) with ascites is extremely rare. We report a 57-year-old woman with EG and massive hemorrhagic ascites who underwent endoscopy and abdominal paracentesis. Differential diagnoses included other causes of tissue eosinophilia. The patient was in good condition 1 year after drug therapy with no recurrence of ascites and gastrointestinal symptoms. To our knowledge, this is the first report of a rare case of massive hemorrhagic ascites in EG. Clinicians should consider the differential diagnosis of unexplained hemorrhagic ascites, especially in patients with gastrointestinal mucosa lesion, peripheral eosinophilia, and ascites.
- Citation: Shi L, Jia QH, Liu FJ, Guan H, Jiang ZY. Massive hemorrhagic ascites: A rare presentation of eosinophilic gastroenteritis. World J Clin Cases 2018; 6(7): 156-160
- URL: https://www.wjgnet.com/2307-8960/full/v6/i7/156.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i7.156
Eosinophilic gastroenteritis (EG) is a rare gastrointestinal disorder characterized by eosinophilic infiltration of the gastrointestinal tract wall with various gastrointestinal manifestations[1]. Ascites due to EG is an exceedingly uncommon diagnosis in the medical literature[2]. Currently, there are no reports of massive hemorrhagic ascites due to EG in the literature. Here, we present a rare case of EG with hemorrhagic ascites and discuss the clinical characteristics and differential diagnosis.
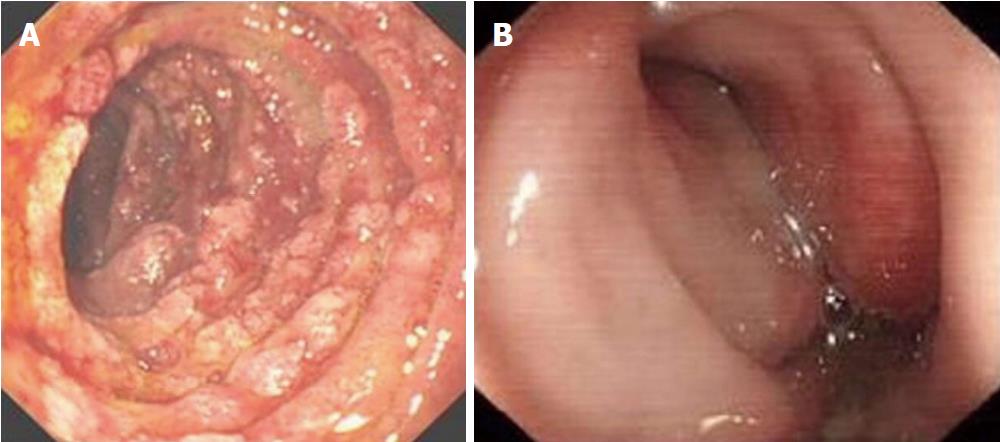
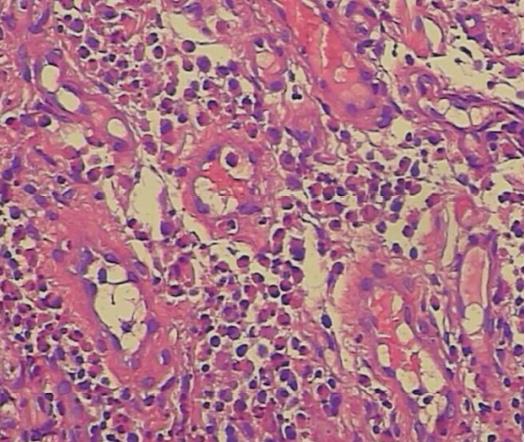
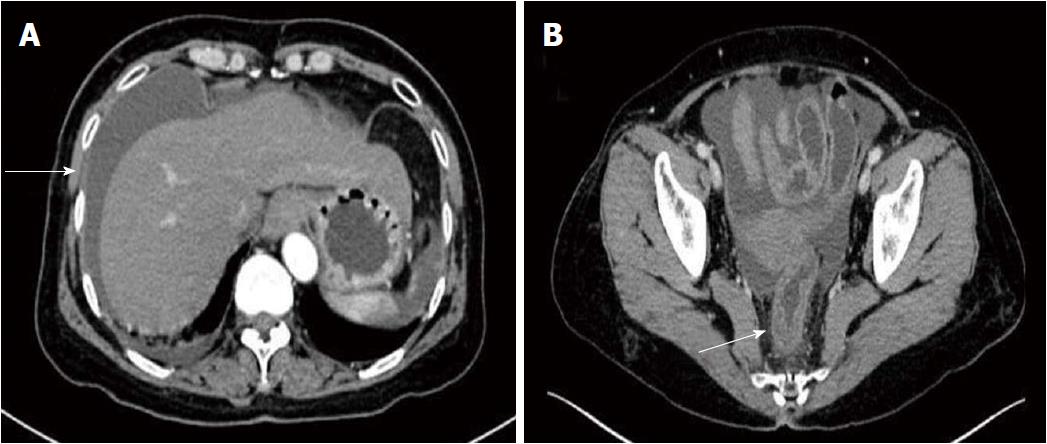
A 57-year-old woman presented with a history of upper abdominal pain and distention for 5 mo. She had no parasitic infestations, allergic diseases, signs and symptoms of eosinophil-mediated tissue injury, and personal or family history of gynecologic malignancy. Various treatment modalities including proton pump inhibitor, antibiotics, and antispasmodics could not relieve her symptoms. The patient was transferred to our hospital for further evaluation and treatment. On physical examination, the abdomen was distended and tender with diffusely shifting dullness present and slight upper abdominal tenderness; there was no sign of rebound tenderness. Laboratory investigations showed the following values: Hgb, 119 g/dL; PLT, 343 k/mL; WBC, 12.8 k/mL; differential: segmentonuclear neutrophils, 10.0%; lymphocytes, 21.2%; monocytes, 2.7%; eosinophils, 65.6%. Serum electrolytes, coagulation studies, and thyroid tests were normal. Parasitic infestation was excluded by repeated negative stool examinations. Chest X-ray examination and ECG were negative. Abdominal ultrasonography showed massive ascites without any organ abnormalities, including the uterus and ovaries. Abdominal paracentesis revealed 1.8 L of hemorrhagic peritoneal fluid with a low serum albumin-ascitic gradient. Microscopy showed abundant white cell counts in the fluid, which were predominantly eosinophils. The ascitic fluid cytology was negative for malignancy, and cultures were negative for acid-fast bacilli, and bacterial and fungal infections. For diagnostic purposes, endoscopy of the upper gastrointestinal tract was performed, which showed erosions, exudates, and mucosal rings in the duodenal mucosa (Figure 1A). Simultaneously, the rectal mucosal exhibited erosions, hyperemia, and swelling on colonoscopy (Figure 1B). Colonoscopy examination revealed no lesions in the proximal colon and the ileum. Biopsies were taken from the duodenal lesion. Histological examination demonstrated characteristic histological findings of eosinophilic infiltrate at approximately 25 eosinophils per high power field in the duodenal mucosa (Figure 2). The patient was negative for Helicobacter pylori determined using 13C-urea breath testing. Unfortunately, there was no pathological examination of the rectal lesions. Computed tomography (CT) imaging also showed peritoneal fluid, but, more importantly, an accompanying local mild thickening of the right rear rectum wall (Figure 3).
Based on our findings and taking into account possible differential diagnoses, we diagnosed the patient with EG characterized by simultaneous mucosal involvement of the duodenum and serosal involvement of the rectum, which rarely presents with massive hemorrhagic ascites. Since the patient refused steroid treatment, ketotifen 1 mg bid po was administered for 1 mo and the patients rapidly responded with a complete resolution of ascites after 2 wk. Moreover, there was a remarkable decline in peripheral eosinophil counts. The patient recovered well and was free from gastrointestinal symptoms and had no recurrence of ascites during the 1-year follow-up period.
EG is a rare gastrointestinal disorder that can present with varying abdominal symptoms such as protein-losing enteropathy, luminal obstruction, and eosinophilic ascites, depending on eosinophilic infiltration into one or more layers and the affected site of the gastrointestinal tract[3]. This disorder was originally described in 1937 by Kaijser[4]. The Klein classification is widely used to classify patients with EG into three clinical forms based on the affected tissue layer: mucosal, muscle, and subserosal[5]. The mucosal form is the most common and presents with abdominal pain, nausea, and protein-losing enteropathy. The muscle form is the second most common and presents with typical symptoms of obstruction. The serosal form is the rarest of the types. Eosinophilic ascites, a high peripheral eosinophil count, and prompt response to steroid therapy are the hallmarks of the serosal form[6]. Rarely, patients can be diagnosed simultaneously with mucosal and subserosal EG.
EG diagnosis is based on the following three clinical criteria: The presence of nonspecific gastrointestinal symptoms; the presence of gastrointestinal eosinophilic infiltrates; and the exclusion of other causes of tissue eosinophilia[7]. Endoscopic findings may also include various manifestations, such as mild erythema, thickened mucosal, and frank ulceration[8,9]. The definite diagnosis of EG is established by demonstrating eosinophilic infiltration on endoscopic, laparoscopic, or laparotomic biopsies. Laparoscopic or laparotomic biopsies are only required if the disease process is confined to the muscle or subserosal layer. Endoscopic ultrasound, abdominal CT, and barium studies documenting the presence of localized or general thickening of the gastrointestinal wall, and gastric outlet obstruction, or ascites can be significant clues to the differential diagnosis of EG[10]. In the present patient, EG was diagnosed after excluding the possibilities of malignancy, parasitic disease, and autoimmune disease.
To our knowledge, this is the first report of a rare case of massive hemorrhagic ascites in EG. We believed that our patient may have the type of EG characterized by simultaneous mucosal and serosal involvement, based on the following satisfied criteria: (1) presence of gastrointestinal symptoms, such as upper abdominal pain and distention; (2) biopsies demonstrating eosinophilic infiltration of the duodenum and ascites concurrently, and CT findings with ascites and mild thickening of the rectum; and (3) no evidence of parasitic or extra-intestinal disease. Our case is distinguished from other causes of hemorrhagic ascites, such as peritoneal tuberculosis, cirrhosis with ruptured hepatocellular carcinoma (HCC), or pancreatic ascites[11] for the following reasons. There were no symptoms or evidence of tuberculosis poisoning in this patient. The ascitic fluid cultures were negative for acid-fast bacilli. Thus, tuberculous peritonitis was excluded in this case. There was no evidence of chronic liver disease in this patient. Upper gastrointestinal endoscopy did not reveal varices. The ascitic fluid cytology was negative for malignancy. Ultrasonography and CT of the abdomen only showed massive ascites without any organ abnormalities, including the liver. Cirrhosis with ruptured HCC could therefore be excluded. Normal amylase and lipase were observed in this patient. Abdominal CT did not reveal peripancreatic inflammatory changes, necrosis, and pseudocyst bulging. Pancreatic ascites was thus excluded. Finally, the diagnosis of EG presenting with hemorrhagic ascites was confirmed. She was empirically treated with ketotifen 1 mg bid po with rapid resolution of ascites. Moreover, there was a remarkable decline in peripheral eosinophil counts.
The pathophysiology of hemorrhagic ascites of EG is unknown, but the widely held belief is that it is a consequence of EG. With the poor understanding of the etiology and pathogenesis of EG, there is currently no standard treatment. However, prednisone is usually selected for management[12]. While most studies have shown up to 90% response rate to prednisone[13], other recent reports have indicated much lower success, at only 50%[14]. EG is recognized as a chronic inflammatory disorder, and most patients require ongoing treatment. It is difficult to sustain therapy with such medications as there is a risk of serious side effects including growth retardation, diabetes, and osteoporosis[15].
Many therapeutic modalities with better safety profiles have been proposed. Therapeutic options include dietary modification and steroid-sparing agents, such as leukotrienes inhibitors, mast cells stabilizers, and anti-histamines. If specific food allergens are suspected or confirmed based on allergic evaluations, dietary therapy should be considered. Dietary measures were predominantly considered in the setting of mucosal disease. The efficacy of dietary therapy in muscular and serosal EG types showed weaker linkage to food allergy[16]. The efficacy of montelukast is controversial for EG; it has shown success as an alternative therapy for minor diseases and as a long-term maintenance treatment[17], while it showed no efficacy in cases with severe, long-standing complicated EG[18]. The effectiveness of sodium cromoglycate in treating EG is not well established. Some patients with EG have obtained significant benefits from sodium cromoglycate[19]. However, individual reports have shown no efficacy for unknown reasons[20]. Ketotifen is a second-generation H1 class of antihistamine agent that is known to modulate the release of mast cell mediators and possibly impair eosinophil migration to target organs. There are limited evidence-based studies on ketotifen treatment in patients with EG. The few reports in the literature concerning its use in EG have shown significant clinical response in patients[21], but it showed no efficacy in some cases[22]. Individual reports of success with sodium cromoglycate and ketotifen therapy have been published[23]. Surgical treatment should only be considered in patients refractory to medical management, or stenotic lesions[24].
After the diagnosis of EG, we initially recommended steroid therapy. However, the patient refused this therapy. Thus, we chose ketotifen, a safe alternative therapy. Our patient responded satisfactorily to ketotifen. There was a marked improvement with normalization of eosinophil count and rapid decrease in ascitic fluid production. During the follow-up period of 1 year, the patient remained asymptomatic, without ascites or hypereosinophilia. We successfully treated our patient with ketotifen initially. However, the effectiveness of ketotifen in treating EG requires further validation.
In conclusion, despite the rarity of EG with massive hemorrhagic ascites, clinicians should consider the differential diagnosis of unexplained hemorrhagic ascites, especially in patients with gastrointestinal mucosa lesion, peripheral eosinophilia, and ascites.
A 57-year-old woman was admitted for upper abdominal pain and distention.
Physical examination revealed the abdomen was distended and tender diffusely with shifting dullness present and slight upper abdominal tenderness.
Peritoneal tuberculosis, cirrhosis with ruptured hepatocellular carcinoma, or pancreatic ascites were considered.
Laboratory investigations showed elevated peripheral eosinophil with significant eosinophilia (65.6%).
Ultrasonography showed massive abdominal ascites. Computed tomography imaging also showed peritoneal fluid, but, more importantly, an accompanied local mild thickening of the right rear rectum wall.
Histological examination demonstrated characteristic histological findings of mild eosinophilic infiltration into the duodenal mucosa.
She was empirically treated with ketotifen 1 mg bid po.
This is the first report of a rare case of massive hemorrhagic ascites in EG.
Eosinophilic gastroenteritis is a rare gastrointestinal disorder characterized by eosinophilic infiltration of the gastrointestinal tract wall with various gastrointestinal manifestations.
Clinicians should consider the differential diagnosis of unexplained hemorrhagic ascites.
| 1. | Baig MA, Qadir A, Rasheed J. A review of eosinophilic gastroenteritis. J Natl Med Assoc. 2006;98:1616-1619. [PubMed] |
| 2. | Liu L, Liang XY, He H, Huang H, Jia LP. Clinical features of eosinophilic gastroenteritis with ascites. Z Gastroenterol. 2013;51:638-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Ingle SB, Hinge Ingle CR. Eosinophilic gastroenteritis: an unusual type of gastroenteritis. World J Gastroenterol. 2013;19:5061-5066. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 69] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (1)] |
| 4. | Kaijser R. Zur Kenntnis der allergischen Affektionen des Verdauugskanals vom Standpunkt des Chirurgen aus. Arch Klin Chir. 1937;188:36-64. |
| 5. | Klein NC, Hargrove RL, Sleisenger MH, Jeffries GH. Eosinophilic gastroenteritis. Medicine (Baltimore). 1970;49:299-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 410] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 6. | Yan BM, Shaffer EA. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58:721-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 121] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 7. | Straumann A. Idiopathic eosinophilic gastrointestinal diseases in adults. Best Pract Res Clin Gastroenterol. 2008;22:481-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 2.2] [Reference Citation Analysis (2)] |
| 8. | Fahey LM, Liacouras CA. Eosinophilic Gastrointestinal Disorders. Pediatr Clin North Am. 2017;64:475-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Abassa KK, Lin XY, Xuan JY, Zhou HX, Guo YW. Diagnosis of eosinophilic gastroenteritis is easily missed. World J Gastroenterol. 2017;23:3556-3564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Abou Rached A, El Hajj W. Eosinophilic gastroenteritis: Approach to diagnosis and management. World J Gastrointest Pharmacol Ther. 2016;7:513-523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 88] [Article Influence: 8.8] [Reference Citation Analysis (5)] |
| 11. | Shabeerali TU, Rajan R, Kuruvilla AP, Noronha S, Krishnadas D, Shenoy KT, Manjula M, Shenoy S, Raji NL. Hemorrhagic ascites: are we missing endometriosis? Indian J Gastroenterol. 2012;31:195-197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Maroto Arce N, Ponce M. [Tuberculosis and the digestive tract]. Gastroenterol Hepatol. 2003;26:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (7)] |
| 13. | Khan S. Eosinophilic gastroenteritis. Best Pract Res Clin Gastroenterol. 2005;19:177-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 110] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 14. | Reed C, Woosley JT, Dellon ES. Clinical characteristics, treatment outcomes, and resource utilization in children and adults with eosinophilic gastroenteritis. Dig Liver Dis. 2015;47:197-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 15. | Kelly HW, Van Natta ML, Covar RA, Tonascia J, Green RP, Strunk RC; CAMP Research Group. Effect of long-term corticosteroid use on bone mineral density in children: a prospective longitudinal assessment in the childhood Asthma Management Program (CAMP) study. Pediatrics. 2008;122:e53-e61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 133] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 16. | Talley NJ, Shorter RG, Phillips SF, Zinsmeister AR. Eosinophilic gastroenteritis: a clinicopathological study of patients with disease of the mucosa, muscle layer, and subserosal tissues. Gut. 1990;31:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 525] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 17. | Tien FM, Wu JF, Jeng YM, Hsu HY, Ni YH, Chang MH, Lin DT, Chen HL. Clinical features and treatment responses of children with eosinophilic gastroenteritis. Pediatr Neonatol. 2011;52:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 18. | Schwartz DA, Pardi DS, Murray JA. Use of montelukast as steroid-sparing agent for recurrent eosinophilic gastroenteritis. Dig Dis Sci. 2001;46:1787-1790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Shih HM, Bair MJ, Chen HL, Lin IT. Eosinophilic Gastroenteritis: Brief Review. Acta Gastroenterol Belg. 2016;79:239-244. [PubMed] |
| 20. | Liacouras CA, Spergel JM, Ruchelli E, Verma R, Mascarenhas M, Semeao E, Flick J, Kelly J, Brown-Whitehorn T, Mamula P. Eosinophilic esophagitis: a 10-year experience in 381 children. Clin Gastroenterol Hepatol. 2005;3:1198-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 659] [Cited by in RCA: 601] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 21. | Bolukbas FF, Bolukbas C, Uzunkoy A, Baba F, Horoz M, Ozturk E. A dramatic response to ketotifen in a case of eosinophilic gastroenteritis mimicking abdominal emergency. Dig Dis Sci. 2004;49:1782-1785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Freeman HJ. Longstanding eosinophilic gastroenteritis of more than 20 years. Can J Gastroenterol. 2009;23:632-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Suzuki J, Kawasaki Y, Nozawa R, Isome M, Suzuki S, Takahashi A, Suzuki H. Oral disodium cromoglycate and ketotifen for a patient with eosinophilic gastroenteritis, food allergy and protein-losing enteropathy. Asian Pac J Allergy Immunol. 2003;21:193-197. [PubMed] |
| 24. | Lucendo AJ, Arias A. Eosinophilic gastroenteritis: an update. Expert Rev Gastroenterol Hepatol. 2012;6:591-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Imaeda H, Rached AA S- Editor: Ji FF L- Editor: A E- Editor: Tan WW