Published online Jun 16, 2018. doi: 10.12998/wjcc.v6.i6.132
Peer-review started: February 8, 2018
First decision: April 13, 2018
Revised: April 27, 2018
Accepted: May 15, 2018
Article in press: May 15, 2018
Published online: June 16, 2018
Processing time: 133 Days and 6.1 Hours
Herpes zoster (HZ) infection occurs in approximately 10% to 30% of individuals. Visceral neuropathies secondary to HZ can cause cystitis and urinary retention. But colonic pseudo-obstruction can also occur. Peripheral neuropathy may reveal segmental motor paresis of either upper or lower limbs, the abdominal muscles or the diaphragm. We report the case of a 62-year-old male patient who presented with abdominal distention and cutaneous vesicular eruption on the left side of the abdominal wall. Plain X-rays and computed tomography scan showed distended small bowel. A diagnosis of intestinal pseudo-obstruction was made secondary to segmental paresis of the small intestine and visceral neuropathy. Conservative management was successful and the patient was discharged uneventfully. Intestinal pseudo-obstruction ought to be considered when dealing with non-obstructive (adynamic) conditions of the digestive tract associated with HZ infection; since early recognition may help to avoid unnecessary surgery.
Core tip: Ogylvie’s syndrome secondary to herpes zoster has been reported as a rare non-surgical complication; but paralytic ileus has received little attention after varicella-zoster reactivation. We report the case of intestinal pseudo-obstruction secondary to small bowel paresis. Possible mechanisms for small bowel involvement and pathophysiology are deeply analysed.
- Citation: Anaya-Prado R, Pérez-Navarro JV, Corona-Nakamura A, Anaya-Fernández MM, Anaya-Fernández R, Izaguirre-Pérez ME. Intestinal pseudo-obstruction caused by herpes zoster: Case report and pathophysiology. World J Clin Cases 2018; 6(6): 132-138
- URL: https://www.wjgnet.com/2307-8960/full/v6/i6/132.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i6.132
Herpes zoster (HZ) infection occurs in approximately 10% to 30% of individuals. And, it has been reported that 95% of the complications are sensory[1-3]. These include acute pain syndromes and post-herpetic neuralgia. Although motor injuries are less frequent, they have a more extensive presentation and can be either visceral or somatic. The somatic motor nerves can be divided into cranial and peripheral. Peripheral neuropathies develop in almost 12% of HZ cases that appear on the head with paralysis of either the fascial or oculomotor areas as the most common clinical features. Peripheral neuropathy can also reveal segmental motor paresis of either the upper and the lower limb muscles, the trunk, the bladder, the gut, or the diaphragm; depending upon the level at which the lesion is located[2]. The diaphragm becomes affected because of phrenic nerve damage. Visceral neuropathies may involve the bladder and cause cystitis and/or urinary retention. But they can also lead to acute colonic pseudo-obstruction; namely, Ogilvie’s syndrome[1-3]. Predisposing factors for varicela-zoster virus (VZV) reactivation from latency are old age, stress, malnutrition, menstruation, and immunosuppression such as malignancy, post-transplant, and chemotherapy[3-7].
Bowel obstruction is normally treated with surgery. However, non-mechanical causes of bowel obstruction need to be carefully investigated before considering surgical intervention. This will avoid unnecessary morbidity and mortality associated to the procedure[2-4]. The diagnosis of VZV-induced bowel pseudo-obstruction requires a high index of suspicion, because visceral symptomatology may appear before the characteristic skin eruption[8-12]. Though, the association of HZ and intestinal pseudo-obstruction is not common and has received insufficient attention in the literature[13-16]. In this paper we describe a patient with intestinal pseudo-obstruction caused by HZ. Its pathophysiology and possible mechanisms for bowel involvement are also addressed.
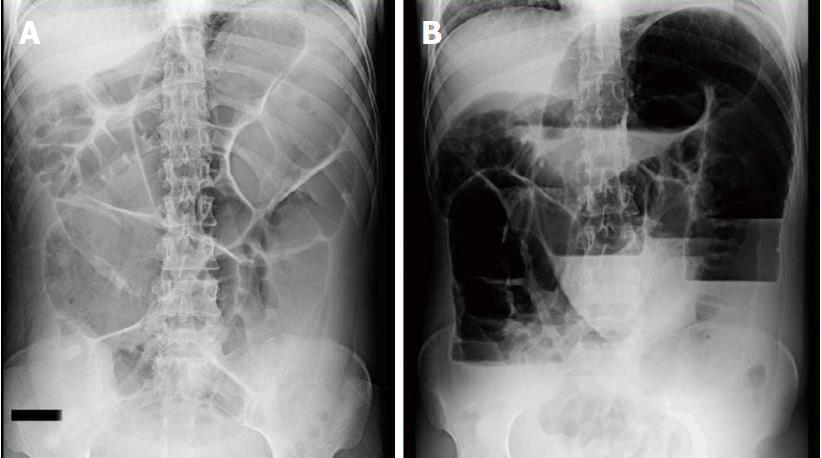
A 62-year-old male patient was admitted with a three-day history of abdominal distention along with abdominal pain, bloating, constipation and concomitant itching and burning skin eruption on the left side of the abdominal wall; which appeared 48 h before admission. Though, there were no complaints of nausea, vomiting or fever. The patient was not taking any medications. On admission, the patient was afebrile and hemodynamically stable. Physical examination revealed abdominal distention and cutaneous vesicular eruption on the left abdomen, extending to the back, not crossing the midline and involving the T7-T10 dermatomes (Figure 1). The abdomen was tense, with tympanitic percussion note all over, with decreased bowel sounds and no signs of peritoneal irritation.
Hamatologic and biochemical tests were all within normal range. Plain X-rays and abdominal computed tomography scan demonstrated distended small bowel loops and air-fluid levels (Figure 2). The diagnosis of intestinal pseudo-obstruction (paralytic Ileus) was made secondary to segmental paresis and visceral neuropathy caused by VZV infection (HZ). Conservative management was then established with nasogastric tube decompression, fasting, intravenous (IV) resuscitation and IV Acyclovir. The patient’s abdominal distention gradually resolved over the next 7 d and pain subsided. The patient was discharged on oral vancyclovir and gabapentin, 8 d after admission. On follow-up, fifteen days later, cutaneous vesicles dried up, changed to scabs and dropped off. The patient showed a full and uneventful recovery.
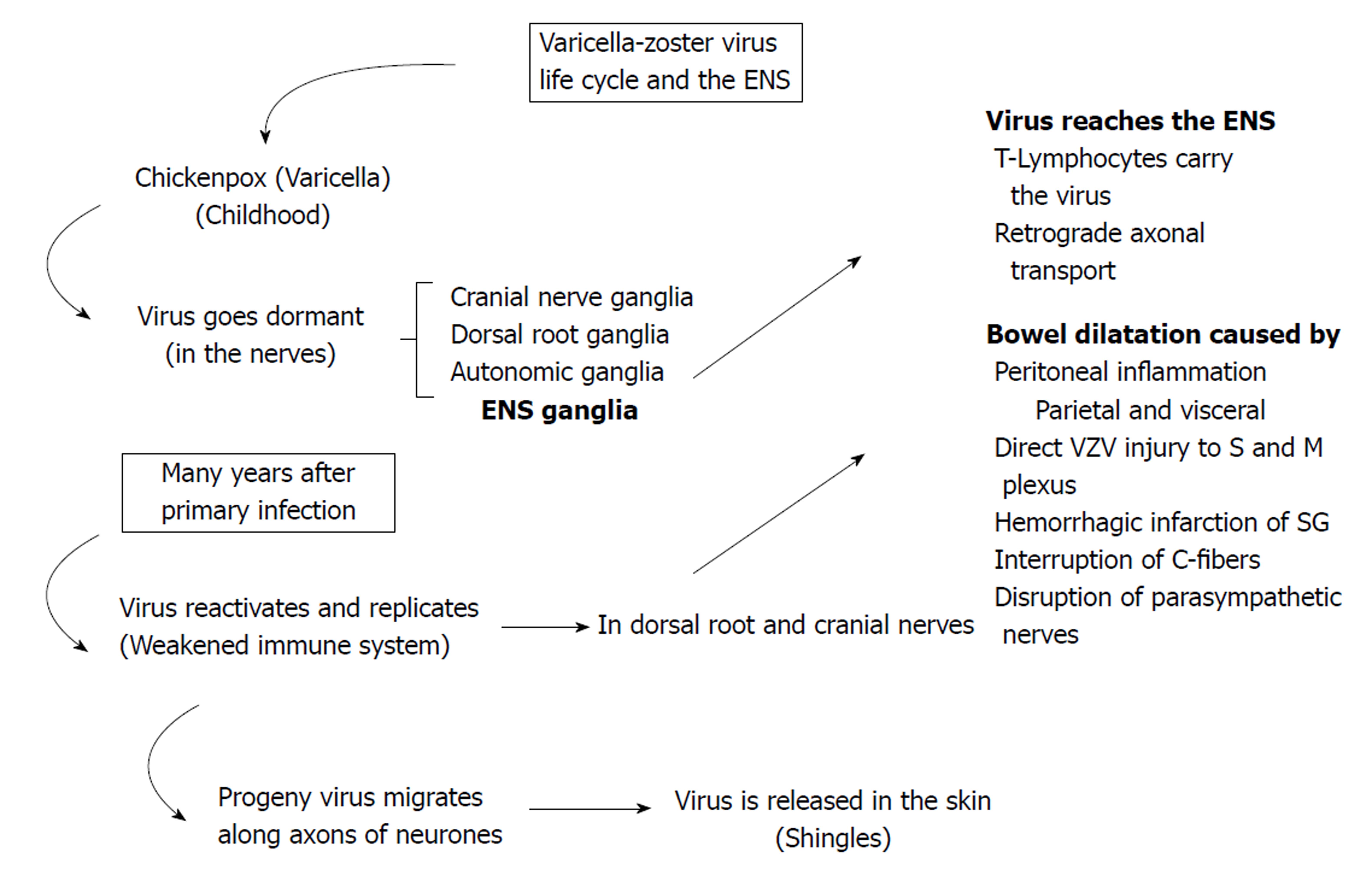
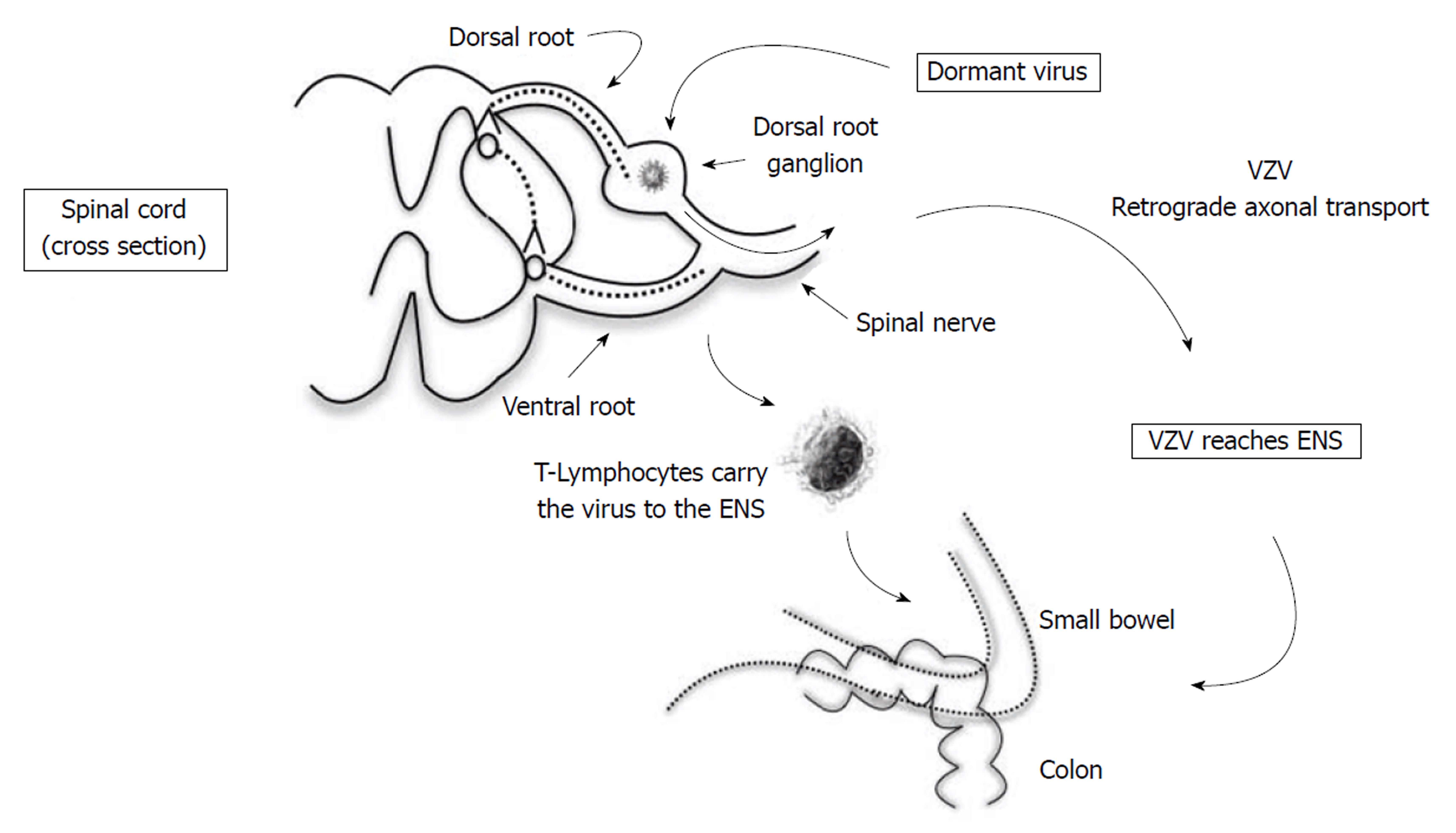
Primary infection with VZV usually takes place in early childhood with fever and diffuse maculopapular rash as common clinical features (chickenpox -varicella-). Then, the virus goes dormant (life-long latency period) in the nerves, including the cranial nerve ganglia, dorsal root ganglia, and autonomic ganglia (Figure 3)[3,6,9]. Of particular importance is the enteric nervous system (ENS) ganglia[13-17]. Many years after the symptomatic primary infection (chickenpox); endogenous viral reactivation may lead to viral replication and inflammation in the ganglion[6,7]. Thus, progeny virus migrates along the axons of neurones and is released in the skin, where it causes HZ (shingles)[6,7,16-18].
With a 5% incidence, peripheral motor neuropathies are the most common neurological complications caused by HZ. They can be either somatic or visceral[8,18,19]. As far as the abdomen is concerned, VZV has been detected in only four locations: Dorsal root ganglion, spinal cord, adrenal gland and the small bowel[5-7]. Our case demonstrated clear involvement of the small intestine; as revealed by distended small bowel. Although vesicular eruption and paralytic ileus were both present on admission; we are aware that this is rather an uncommon presentation for patients with HZ and concomitant intestinal pseudo-obstruction. Because dermal eruption has been reported to appear days to weeks after bowel involvement[3,9,20].
Herpes zoster occurring in the abdomen can lead to paralysis of either the diaphragm or the bladder[3,9,20-22]. But, gastrointestinal symptomatology is extremely rare. Although the coexistence of HZ and Ogilvie’s syndrome has been reported in 30 patients; this presentation is still considered very uncommon[23-27]. In most of these cases, colonic pseudo-obstruction started days to weeks before skin eruptions appeared. This type of presentation poses a significant diagnostic challenge that may result in unnecessary surgery[28-32]. On the other hand, diaphragmatic paralysis has also been reported in 30 patients since 1940[33-37]. These cases were mostly women (60%) aged 32 to 83 years, with skin vesicles and ipsilateral paralysis[38-42]. Nevertheless, colonic pseudo-obstruction due to herpes zoster is still considered the most common gastrointestinal complication since the first case reported back in 1950[43-47]. Interestingly enough, in a letter sent to the editor, an anonymous author already reported HZ involvement of the spinal nerves along with the sympathetic innervation of the transverse colon[48,49]. So far, this association has been published in 22 studies that include 30 patients[3,9]. These reports cover 23 men and 7 women aged 32 to 87 years, with significant comorbidities and neoplasms in 45% and 28% of the cases, respectively. Conservative management was therapeutic in most of the cases (83%). Although 2 patients died[3,9,50-52].
Paralytic ileus (PI) is a less frequently reported gastrointestinal complication following HZ infection. Actually, PI was first described in 1959 by Cane and later by Johnson in 1977[8,11,53,54]. These authors acknowledged a temporary involvement of the sympathetic innervation of the large intestine as the cause of PI. Actually, these are the only two cases published in the western literature with a satisfactory response to conservative management[53,54]. This therapy has been demonstrated to be effective for bowel symptoms to subside in an average of 8 d[11,55,56]. Our case was not the exception and intestinal pseudo-obstruction had an adequate response to conservative measures. That is, surgery was not necessary[57].
Many theories have been proposed as possible causes for bowel motor injuries after VZV infection. First, VZV reaches the ENS by means of two possible mechanisms (Figure 4). Either T Lymphocytes carry the virus which gets lodged in the enteric ganglia; or there is a retrograde axonal transport from dorsal-root ganglion neurones infected through their epidermal projections[2-6]. The fact of the matter is that whatever prompts VZV reactivation is likely to result in the same effect in the ENS neurones[7-9]. Therefore, bowel dilatation (paralysis) has been suggested to be caused by a series of different actions: (1) parietal and visceral peritoneal inflammation; (2) extrinsic autonomic nervous system viral involvement; (3) direct VZV injury of both the enteric submucosal and myenteric plexus, as well as the muscularis propria; (4) possible hemorrhagic infarction of the abdominal sympathetic ganglia; (5) viral interruption of afferent C-fibers that cause intestinal hypomotility and subsequent pseudo-obstruction; and (6) viral injury of the thoracolumbar or sacral lateral columns resulting in disruption of parasympathetic nerves and subsequent intestinal hypomotility[3,5-7,9]. Enteric Nervous System involvement was recently demonstrated in two immunocompromised patients. Small intestine biopsies tested positive for VZV DNA. Thus, myenteric plexus and muscularis propria injury were considered responsible for the paralytic Ileus developing in these two patients[3,9].
We believe that our case followed a similar pattern after HZ infection; that is, paralytic Ileus secondary to myenteric plexus and muscularis propria injury. Lessons learned from postoperative ileus studies support a role for an enhanced release of nitric oxide (NO) after mechanical stimulation of the gut[41,58]. Though, the exact source of increased NO production is not clear. However, NO is generally accepted as one of the main neurotransmitters of the inhibitory non-adrenergic non-cholinergic (NANC) nerves in different organ systems, including the gastrointestinal tract. In general, evidence has shown that, by releasing NO, adrenergic and non-adrenergic nerves are involved in the pathogenesis of ileus. The proposed mechanism is that hyperactivity of adrenergic pathways leads to the activation of α2-adrenoceptors on the intrinsic cholinergic neurones and to a decreased release of acetylcholine; thereby inhibiting gastrointestinal motility. Furthermore, since NO is an important inhibitory neurotransmitter in the gut; it has been proposed that, in addition to adrenergic pathways, an inhibitory nitrergic NANC pathway is activated, contributing to the genesis of ileus. It has also been proposed that NO release triggers vasoactive intestinal polypeptides as well as the mu or kappa-opioid receptors[58-60]. These mediators, in turn, trigger macrophages that release proinflammatory cytokines. It has been suggested that activation of the muscularis macrophages is an initial step in the post-surgical inflammatory cascade. These inflammatory reactions depend largely on the expression of Interleukins (IL), especially IL-6; which are known to be prototypic proinflammatory cytokines. And, they have been shown to be involved in the local inflammatory reaction within the intestinal muscularis after surgical insult[61]. The issue is that the activated inflammatory cascade results in leukocyte and mast cell extravasation into the intestinal muscle. Subsequent to this local muscularis inflammatory response, gastrointestinal motility is diminished, resulting in paralytic ileus[56,58-61].
Since the number of published studies reporting the combination of HZ and paralytic ileus is very limited; study subjects tend to be both insufficient and heterogeneous. In fact, only two studies have reported the presence of VZV in the intestinal muscle (see above)[3,9]. Additionally, most reported cases involve colonic pseudo-obstruction; that is, Ogilvie’s syndrome and HZ. In our case, VZV reactivation took place in the small bowel; thus, paralytic ileus ensued[11]. Although we have discussed the proposed pathophysiology of postoperative paralytic ileus as well as the possible causes for bowel motor injuries after VZV infection; the bimolecular basis of ENS injury is yet to be clarified[11,53-56]. However, we believe that VZV triggers an inflammatory cascade similar to that reported in postoperative paralytic ileus[57-61].
Clinical presentation of paralytic ileus secondary to HZ infection is difficult to differentiate from other causes of mechanical bowel obstruction; abdominal distention included. Furthermore, HZ cutaneous vesicles may or may not appear; which makes diagnosis even more difficult. Although skin lesions have been reported to appear days after acute colonic pseudo-obstruction (Ogilvie’s syndrome), therefore, a definitive diagnosis is usually made after non-mechanical conditions (as well as electrolyte disturbances) have been considered and discarded; otherwise, unnecessary surgery will be performed[11,53-56]. Once diagnosis has been established, conservative management is the treatment of choice of paralytic ileus caused by HZ infection. Thus, supportive measures are initiated with fasting, nasogastric tube decompression (if necessary), intravenous rehydration, correction of electrolyte abnormalities (if any) and treatment of other contributing disorders. On the other hand, antivirals are usually indicated for herpes zoster conditions. However, there is very limited evidence evaluating their role in the atypical gastrointestinal complications secondary to HZ. So, their efficacy, under these circumstances, is yet to be determined[11,53,56,62]. In our case, other than the supportive measures, IV Acyclovir was indicated as treatment for the basic contributing disorder (HZ). Evidently, skin rash and intestinal pseudo-obstruction (abdominal distention) improved in a matter of days; however, we cannot conclude that antiviral therapy had a role in intestinal improvement. Still, conservative measures along with antiviral therapy have proven to be effective when dealing with cases of intestinal pseudo-obstruction secondary to HZ infection[63]. From the surgical perspective, intestinal pseudo-obstruction ought to be considered when dealing with non-obstructive (adynamic) conditions of the digestive tract associated with HZ infection; since early recognition may help to avoid unnecessary surgery.
A 62-year-old male patient presented with abdominal distention and cutaneous vesicular eruption on the left side of the abdominal wall.
The diagnosis of intestinal pseudo-obstruction (paralytic Ileus) was made secondary to segmental paresis and visceral neuropathy caused by varicela-zoster virus (VZV) infection [herpes zoster (HZ)].
Mechanical bowel obstruction ought to be discarded.
Plain X-rays and computed tomography imaging demonstrated distended small bowel loops suggestive of paralytic Ileus.
Conservative management was established with nasogastric tube decompression, fasting, intravenous (IV) resuscitation and IV Acyclovir.
Most reported cases of intestinal pseudo-obstruction caused by HZ involve the colon. In our case, VZV reactivation took place in the small bowel; which is still considered a very rare gastrointestinal complication.
VZV causes chickenpox (varicella) and HZ.
Intestinal pseudo-obstruction ought to be considered when dealing with non-obstructive (adynamic) conditions of the digestive tract associated with HZ infection; since early recognition may help to avoid unnecessary surgery.
| 1. | Tribble DR, Church P, Frame JN. Gastrointestinal visceral motor complications of dermatomal herpes zoster: report of two cases and review. Clin Infect Dis. 1993;17:431-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 2. | Masood I, Majid Z, Rind W, Zia A, Riaz H, Raza S. Herpes Zoster-Induced Ogilvie's Syndrome. Case Rep Surg. 2015;2015:563659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Carrascosa MF, Salcines-Caviedes JR, Román JG, Cano-Hoz M, Fernández-Ayala M, Casuso-Sáenz E, Abascal-Carrera I, Campo-Ruiz A, Martín MC, Díaz-Pérez A. Varicella-zoster virus (VZV) infection as a possible cause of Ogilvie's syndrome in an immunocompromised host. J Clin Microbiol. 2014;52:2718-2721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Tanida E, Izumi M, Abe T, Tsuchiya I, Okuma K, Uchida E, Hidaka A, Hayashi E, Noguchi M, Masui Y. [Disseminated varicella-zoster virus infection complicated with severe abdominal pain and colonic pseudo-obstruction]. Nihon Shokakibyo Gakkai Zasshi. 2013;110:839-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Cohen JI. The varicella-zoster virus genome. Curr Top Microbiol Immunol. 2010;342:1-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Chen T, Hudnall SD. Anatomical mapping of human herpesvirus reservoirs of infection. Mod Pathol. 2006;19:726-737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Nikkels AF, Delvenne P, Sadzot-Delvaux C, Debrus S, Piette J, Rentier B, Lipcsei G, Quatresooz P, Piérard GE. Distribution of varicella zoster virus and herpes simplex virus in disseminated fatal infections. J Clin Pathol. 1996;49:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Jucgla A, Badell A, Ballesta C, Arbizu T. Colonic pseudo-obstruction: a complication of herpes zoster. Br J Dermatol. 1996;134:788-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Pui JC, Furth EE, Minda J, Montone KT. Demonstration of varicella-zoster virus infection in the muscularis propria and myenteric plexi of the colon in an HIV-positive patient with herpes zoster and small bowel pseudo-obstruction (Ogilvie's syndrome). Am J Gastroenterol. 2001;96:1627-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Rexinger EL. Herpes zoster presenting as soft abdominal mass with obstipation. Cutis. 1983;31:489. [PubMed] |
| 11. | Johnson JN, Sells RA. Herpes zoster and paralytic ileus: a case report. Br J Surg. 1977;64:143-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Batke M, Cappell MS. Adynamic ileus and acute colonic pseudo-obstruction. Med Clin North Am. 2008;92:649-670, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Wyburn-Mason R. Visceral lesions in herpes zoster. Br Med J. 1957;1:678-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Menuck LS, Brahme F, Amberg J, Sherr HP. Colonic changes of herpes zoster. AJR Am J Roentgenol. 1976;127:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Kesner KM, Bar-Maor JA. Herpes zoster causing apparent low colonic obstruction. Dis Colon Rectum. 1979;22:503-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Walsh TN, Lane D. Pseudo obstruction of the colon associated with varicella-zoster infection. Ir J Med Sci. 1982;151:318-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Zhou SR, Liu CY. A case report of abdominal distention caused by herpes zoster. World J Gastroenterol. 2012;18:4627-4628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 18. | Maeda K, Furukawa K, Sanada M, Kawai H, Yasuda H. Constipation and segmental abdominal paresis followed by herpes zoster. Intern Med. 2007;46:1487-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Zell R, Taudien S, Pfaff F, Wutzler P, Platzer M, Sauerbrei A. Sequencing of 21 varicella-zoster virus genomes reveals two novel genotypes and evidence of recombination. J Virol. 2012;86:1608-1622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Edelman DA, Antaki F, Basson MD, Salwen WA, Gruber SA, Losanoff JE. Ogilvie syndrome and herpes zoster: case report and review of the literature. J Emerg Med. 2010;39:696-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 21. | Ingraham IE Jr, Estes NA, Bern MM, DeGirolami PC. Disseminated varicella-zoster virus infection with the syndrome of inappropriate antidiuretic hormone. Arch Intern Med. 1983;143:1270-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Caccese WJ, Bronzo RL, Wadler G, McKinley MJ. Ogilvie's syndrome associated with herpes zoster infection. J Clin Gastroenterol. 1985;7:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Pai NB, Murthy RS, Kumar HT, Gerst PH. Association of acute colonic pseudo-obstruction (Ogilvie's syndrome) with herpes zoster. Am Surg. 1990;56:691-694. [PubMed] |
| 24. | Alpay K, Yandt M. Herpes zoster and Ogilvie's syndrome. Dermatology. 1994;189:312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Nomdedéu JF, Nomdedéu J, Martino R, Bordes R, Portorreal R, Sureda A, Domingo-Albós A, Rutllant M, Soler J. Ogilvie's syndrome from disseminated varicella-zoster infection and infarcted celiac ganglia. J Clin Gastroenterol. 1995;20:157-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 28] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 26. | Halpern SL, Covner AH. Motor manifestations of herpes zoster; report of a case of associated permanent paralysis of the phrenic nerve. Arch Intern Med (Chic). 1949;84:907-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Cervia T. [Paralysis of hemidiaphragm by herpes zoster]. Rev Clin Esp. 1953;49:397-399. [PubMed] |
| 28. | Parker GW, Ramos ED. Paralysis of the phrenic nerve following herpes zoster. J Am Med Assoc. 1962;180:408-410. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 29. | Spiers AS. Herpes zoster and its motor lesions, with a report of a case of phrenic nerve paralysis. Med J Aust. 1963;50:850-853. [PubMed] |
| 30. | Beard HW. Phrenic paralysis due to herpes zoster. A case report. Med Bull US Army Eur. 1963;20:106. [PubMed] |
| 31. | Donald TC. Paralysis of the diaphragm secondary to herpes zoster. J Med Assoc State Ala. 1964;33:306-308. [PubMed] |
| 32. | Brostoff J. Diaphragmatic paralysis after herpes zoster. Br Med J. 1966;2:1571-1572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Pratt JH. Diaphragmatic paralysis after herpes. Br Med J. 1967;1:234-235. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 34. | Anderson JP, Keal EE. Cervical herpes zoster and diaphragmatic paralysis. Br J Dis Chest. 1969;63:222-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 35. | Dutt AK. Diaphragmatic paralysis caused by herpes zoster. Am Rev Respir Dis. 1970;101:755-758. [PubMed] |
| 36. | Shivalingappa G. Diaphragmatic paralysis following herpes zoster. Gerontol Clin (Basel). 1970;12:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 37. | Derveaux L, Lacquet LM. Hemidiaphragmatic paresis after cervical herpes zoster. Thorax. 1982;37:870-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Hayashi S, Ichikawa Y, Shoji H, Kaji M. A case of diaphragmatic paralysis and neuralgic amyotrophy-like symptoms following cervical zoster. Shinkeinaika. 1984;21:484-487. |
| 39. | Stowasser M, Cameron J, Oliver WA. Diaphragmatic paralysis following cervical herpes zoster. Med J Aust. 1990;153:555-556. [PubMed] |
| 40. | Melcher WL, Dietrich RA, Whitlock WL. Herpes zoster phrenic neuritis with respiratory failure. West J Med. 1990;152:192-194. [PubMed] |
| 41. | Soler JJ, Perpiña M, Alfaro A. Hemidiaphragmatic paralysis caused by cervical herpes zoster. Respiration. 1996;63:403-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 42. | Fujimoto S, Matsuno O, Matsumoto T, Kumamoto T, Tsuda T. [A case of diaphragmatic paralysis following herpes zoster]. Rinsho Shinkeigaku. 1996;36:345-347. [PubMed] |
| 43. | Paudyal BP, Karki A, Zimmerman M, Kayastha G, Acharya P. Hemidiaphragmatic paralysis: a rare complication of cervical herpes zoster. Kathmandu Univ Med J (KUMJ). 2006;4:246-248. [PubMed] |
| 44. | Manabe Y, Higa K, Kawamura M, Hirata K, Hirota K. Ipsilateral diaphragmatic paralysis after cervical herpes zoster. Pain Clinic. 2007;53:1036-1039. |
| 45. | Morinaga R, Matsunaga N, Iwata A, Kishi K, Tokimatsu I, Nagai H, Kadota J. [A case of diaphragmatic paralysis caused by herpes zoster after anticancer chemotherapy]. Nihon Kokyuki Gakkai Zasshi. 2007;45:166-169. [PubMed] |
| 46. | Hoque R, Schwendimann RN, Liendo C, Chesson AL Jr. Brachial neuritis with bilateral diaphragmatic paralysis following herpes zoster: a case report. J Clin Neuromuscul Dis. 2008;9:402-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 47. | Bahadir C, Kalpakcioglu AB, Kurtulus D. Unilateral diaphragmatic paralysis and segmental motor paresis following herpes zoster. Muscle Nerve. 2008;38:1070-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 48. | Oike M, Naito T, Tsukada M, Kikuchi Y, Sakamoto N, Otsuki Y, Ohshima H, Yokokawa H, Isonuma H, Dambara T. A case of diaphragmatic paralysis complicated by herpes-zoster virus infection. Intern Med. 2012;51:1259-1263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 49. | Herpes zoster and varicella complicated by paralysis of the transverse colon. Lancet. 1950;2:822. [DOI] [Full Text] |
| 50. | Herath P, Gunawardana SA. Acute colonic pseudo-obstruction associated with varicella zoster infection and acyclovir therapy. Ceylon Med J. 1997;42:36-37. [PubMed] |
| 51. | Healy C, McGreal G, Lenehan B, McDermott EW, Murphy JJ. Self-limiting abdominal wall herniation and constipation following herpes zoster infection. QJM. 1998;91:788-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 52. | Giunta R, Marfella MA, Maffei A, Lucivero G. Herpes zoster infection and Ogilvie's syndrome in non-Hodgkin's lymphoma with hypogammaglobulinemia. Ann Ital Med Int. 2001;16:50-53. [PubMed] |
| 53. | Cane H. Herpes Zoster and Paralytic Ileus. Br Med J. 1959;2:887. [RCA] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 54. | Hiramatsu S, Nebiki H, Ueno A, Wakahara Y, Maruyama H, Suekane T, Yamasaki T, Sasaki E, Sano K, Sato H. [A case of paralytic ileus associated with varicella zoster virus infection]. Nihon Shokakibyo Gakkai Zasshi. 2013;110:1007-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 55. | FIGIEL SJ, FIGIEL LS. Herpes zoster with ileus simulating intestinal obstruction. Am J Med. 1957;23:999-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 56. | Bauer AJ, Schwarz NT, Moore BA, Türler A, Kalff JC. Ileus in critical illness: mechanisms and management. Curr Opin Crit Care. 2002;8:152-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 83] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 57. | Braude MR, Trubiano JA, Heriot A, Dickinson M, Carney D, Seymour JF, Tam CS. Disseminated visceral varicella zoster virus presenting with the constellation of colonic pseudo-obstruction, acalculous cholecystitis and syndrome of inappropriate ADH secretion. Intern Med J. 2016;46:238-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 58. | De Winter BY, Boeckxstaens GE, De Man JG, Moreels TG, Herman AG, Pelckmans PA. Effect of adrenergic and nitrergic blockade on experimental ileus in rats. Br J Pharmacol. 1997;120:464-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 117] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 59. | Schwarz NT, Kalff JC, Türler A, Speidel N, Grandis JR, Billiar TR, Bauer AJ. Selective jejunal manipulation causes postoperative pan-enteric inflammation and dysmotility. Gastroenterology. 2004;126:159-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 123] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 60. | De Winter BY, Boeckxstaens GE, De Man JG, Moreels TG, Herman AG, Pelckmans PA. Effects of mu- and kappa-opioid receptors on postoperative ileus in rats. Eur J Pharmacol. 1997;339:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 61. | Wehner S, Behrendt FF, Lyutenski BN, Lysson M, Bauer AJ, Hirner A, Kalff JC. Inhibition of macrophage function prevents intestinal inflammation and postoperative ileus in rodents. Gut. 2007;56:176-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 191] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 62. | Hong JJ, Elgart ML. Gastrointestinal complications of dermatomal herpes zoster successfully treated with famciclovir and lactulose. J Am Acad Dermatol. 1998;38:279-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 63. | Rodrigues G, Kannaiyan L, Gopasetty M, Rao S, Shenoy R. Colonic pseudo-obstruction due to herpes zoster. Indian J Gastroenterol. 2002;21:203-204. [PubMed] |
CARE Checklist (2013) statement: Guidelines of the CARE Checklist (2013) have been adopted.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Mexico
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sugimoto M, Surani S S- Editor: Ji FF L- Editor: Filipodia E- Editor: Tan WW