Published online Dec 6, 2018. doi: 10.12998/wjcc.v6.i15.1053
Peer-review started: September 10, 2018
First decision: October 11, 2018
Revised: October 28, 2018
Accepted: October 31, 2018
Article in press: November 1, 2018
Published online: December 6, 2018
Processing time: 89 Days and 22 Hours
Since the acute fibrinous and organizing pneumonia (AFOP) was first described by Beasley in 2002, some case reports of patients aged from 38 d to 80 years have been published worldwide, but there is still no standard therapy for this disease and the treatment methods remain controversial. Both steroid and immunosuppressive agents, such as cyclophosphamide or mycophenolate mofetil, have been reported to be effective in some studies, but with many side effects, especially in patients of advanced age.
We herein report an 81-year-old female patient who was admitted to our hospital due to dry cough, and breathlessness for 1 mo. She was treated with broad-spectrum antibiotics and anti-fungal therapy, but without improvement in both symptoms and radiological findings, and her respiratory status worsened, and she required bed rest almost the whole day. Computed tomography-guided percutaneous needle lung biopsy was performed and histopathology examination confirmed the diagnosis of AFOP. She was then successfully treated with a steroid monotherapy, which resulted in a satisfactory clinical outcome without serious complications.
We conclude that complete remission of AFOP can be achieved by steroid monotherapy in patients of advanced age.
Core tip: Acute fibrinous and organizing pneumonia is a rare histological pattern of acute lung injury. The age of the patients was diverse from infant to elderly, and there is still no specific therapy. Although treatments with steroids combined with immunosuppressants have been reported, none of them showed particular benefit, and these treatments always induce serious side effects, especially in patients of advanced age. We herein report an 81-year-old female patient, who was successfully treated with low-dose steroids, and only experienced some minor side-effects. This case report can add a new treatment choice for this disease.
- Citation: Ning YJ, Ding PS, Ke ZY, Zhang YB, Liu RY. Successful steroid treatment for acute fibrinous and organizing pneumonia: A case report. World J Clin Cases 2018; 6(15): 1053-1058
- URL: https://www.wjgnet.com/2307-8960/full/v6/i15/1053.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i15.1053
Acute fibrinous and organizing pneumonia (AFOP) was first described by Beasley in a pathologic study of 17 patients with acute/subacute lung injury in 2002[1]. It was defined as a rare type of the idiopathic interstitial pneumonia in 2013[2]. A few studies have reported the characteristics of AFOP in recent years, but the etiology is still not fully understood. AFOP may occur at any age, but usually presents in the elderly people. The clinical presentation of AFOP is nonspecific and often similar to common pneumonia, so it is easily misdiagnosed. The confirmation of AFOP diagnosis depends on pathological biopsy.
To date, the pathogenesis of AFOP remains unclear, and there is still no standard treatment. Steroid treatment was reported to be effective, but the information on dosage, duration and long-term side-effects is not available. We herein report a case of an 81-year-old female patient with AFOP, who was successfully treated with steroid monotherapy. We also report our observations of the dosage, duration and side-effects. This report can provide a new choice of AFOP treatment in geriatric patients.
An 81-year-old retired female doctor was admitted to our hospital with dry cough, and breathlessness for 1 mo.
She had taken Azithromycin for 2 d, but there was no improvement.
She denied any history of disease.
On examination, her temperature was 36.5 °C, blood pressure was 108/72 mmHg, heart rate was 74 beats/min, oxygen saturation was 98% at room air, and respiratory rate was 19 breaths/min. Lung examination showed inspiratory crackles in the right lung base. The rest of her physical examinations were unremarkable.
Blood routine, liver function, renal function tests and serum sodium, potassium, creatinine, magnesium, calcium were all within normal limits. Blood tumor biomarker tests were negative. Serologic tests for antinuclear antibodies, rheumatoid factors and anti-neutrophil cytoplasmic antibodies were within normal limits. Tuberculin skin test, sputum stains for acid fast bacilli, and cultures of blood and sputum were all negative. Arterial blood gas analysis at room air revealed pH 7.4, PaO2 63 mmHg and PaCO2 35 mmHg. The pulmonary function test revealed moderate restrictive ventilatory impairment and a moderate decrease in diffusing capacity.
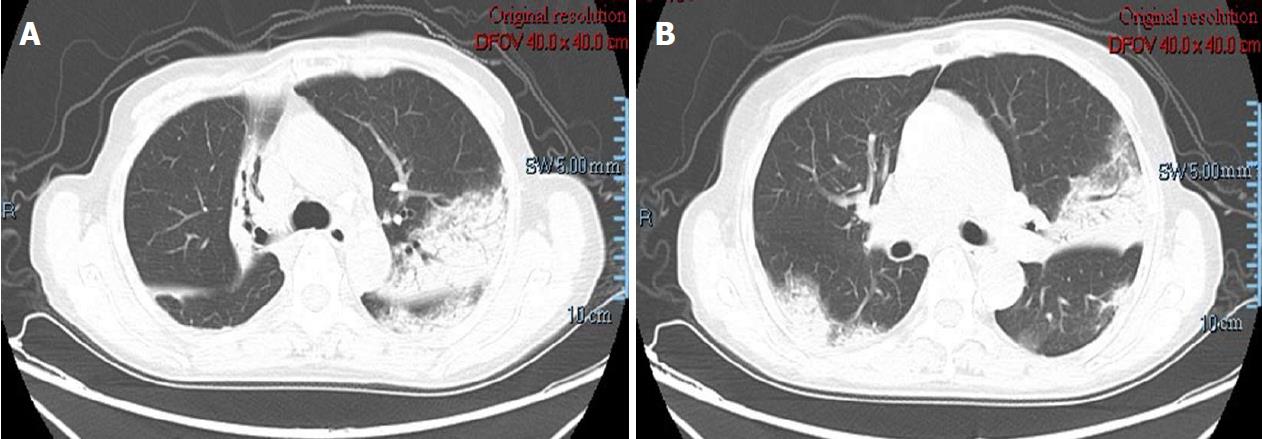
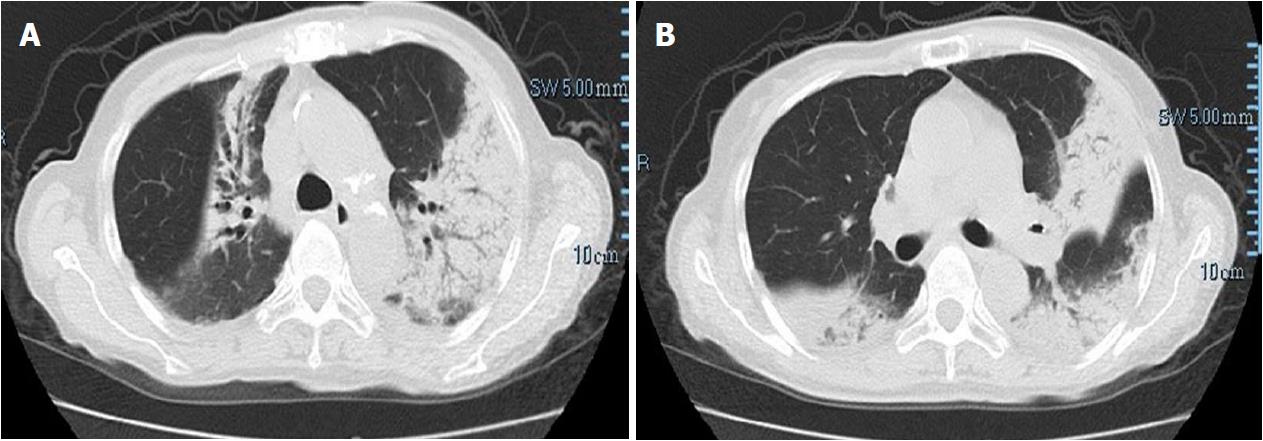
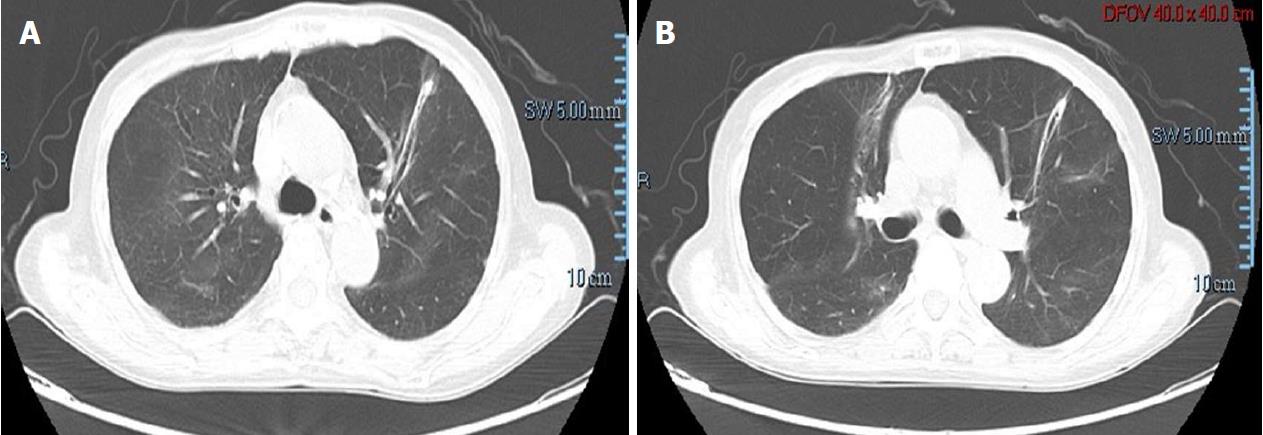
Computed tomography (CT) scan of the chest on admission showed bilateral lesions, multiple patchy, consolidation and ground-glass opacities, associated with air bronchogram (Figure 1), especially in the right lung and the upper lobe of the left lung. The patient was treated with broad-spectrum antibiotics and anti-fungal therapy in the following 2 wk. But her symptoms of cough and chest tightness, and shortness of breath were not relieved. The repeat CT scan of the chest 2 wk later (Figure 2) showed that her condition was significantly advanced, which means a previous misdiagnosis. CT-guided percutaneous needle lung biopsy was then performed after informed consent was obtained from the patient.
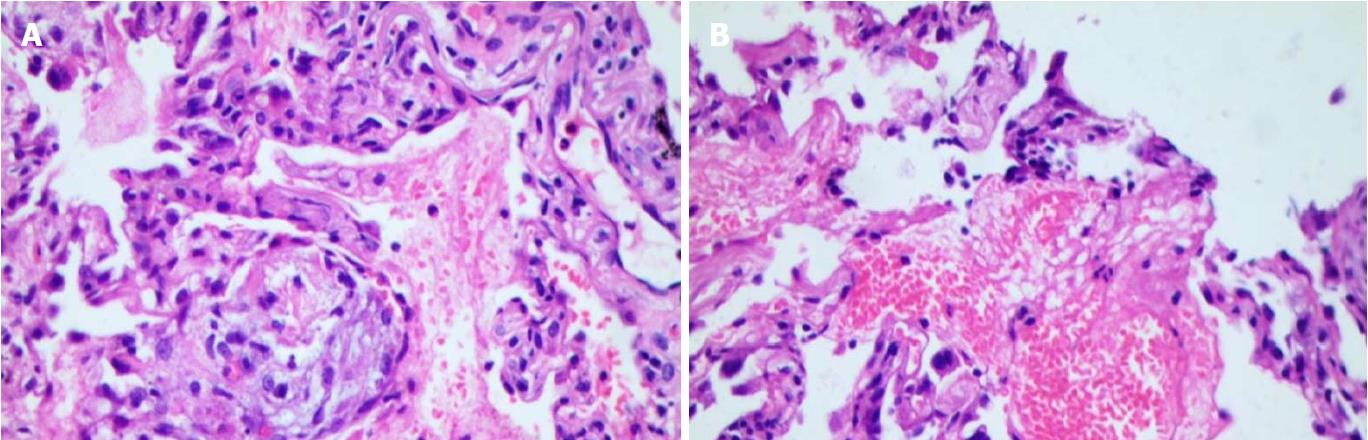
The pathologic consultation revealed prominent fibrinous exudation within most the alveolar spaces (Figure 3). No necrosis or granulomas were observed, neither any evidence of diffuse alveolar damage, alveolitis or eosinophilic infiltration. No evidence of special infections was found. A diagnosis of AFOP was established.
AFOP.
The patient was therefore started with intravenous methylprednisolone 40 mg/d for 1 wk. Considering the old age of the patient, and the considerable side effects of the drug, we then reduced the dosage to 12 mg twice daily taken orally for 1 wk. The patient discharged on a tapering schedule of methylprednisolone 20 mg/d for 10 d, then 16 mg/d for 10 d, 12 mg/d for 10 d, and 8 mg/d for 1 mo.
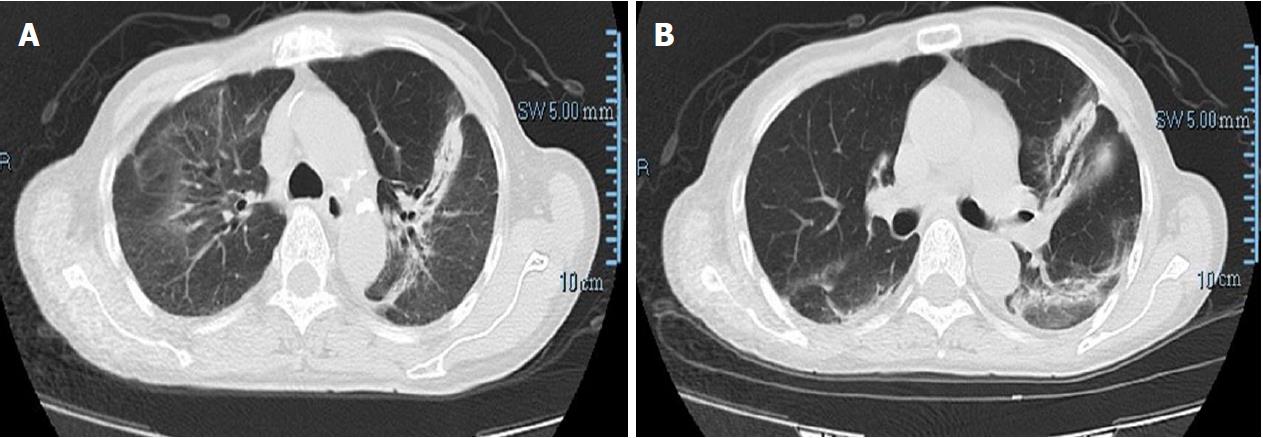
After 1 wk treatmengt of methylprednisolone 40 mg/d, her symptom of cough was improved. CT scan also showed significant improvement (Figure 4), and bilateral lesions resolved gradually. During the treatment with steroids, the main side-effects were hypertension and hyperglycaemia, which were resolved by antihypertensives and dietary and lifestyle modifications. No significant adverse side-effects were noticed. The repeat chest CT scan revealed almost normal findings after 3 wk (Figure 5).
In 2002, Beasley[1] described a new histological pattern of lung injury named AFOP, which is characterized by intra-alveolar fibrin balls and organizing pneumonia with a patchy distribution. Sporadic case reports have been published on this newly recognized clinicopathological entity that is still underdiagnosed. In 2013, it was finally defined as a rare type of the idiopathic interstitial pneumonia by the American Thoracic Society/European Respiratory Society[2]. AFOP is rarely reported worldwide. We searched the PubMed using the keywords “AFOP” or “acute fibrinous and organizing pneumonia”, and identified 74 relevant articles. The age of the patients was diverse from infant to elderly[3-5]. It is more common in males than in females[1]. Our patient was an 81-year-old female, who was the oldest one according to the literature.
Although the histopathological features are well described, the clinical manifestations, course, and treatment of AFOP are not characterized. Because the clinical manifestations are nonspecific, the pathogenesis of AFOP is not fully understood. It can be idiopathic or associated with a wide spectrum of clinical conditions, such as connective tissue diseases[4,6,7], bacterial infections or viral infections[3,8], specific etiologic agent like Chlamydophila pneumoniae[9], chronic renal insufficiency[10], drug reaction or drug-induced toxicity[11], hematologic disease[12,13], hematopoietic stem cell transplantation[14], and occupational or environmental exposures[1].
There is still no standard treatment for AFOP. Therapy with steroids alone or combined with immunosuppressants was attempted, but the dosage and duration of steroid treatment are still unclear. Usually 0.5-1 mg/kg daily of prednisone (or equivalent) are prescribed initially. A maximal dose of methylprednisolone was reported to be up to 1000 mg/d[4]. A pulse therapy of steroids was also administered in some fulminant patients[7,10,15,16]. Besides steroids, immunosuppressive agents such as cyclophosphamide, mycophenolate mofetil, cyclosporine and azathioprine have been tried in AFOP patients complicated with connective tissue diseases[4,6,7,17]. In addition, Zhou et al[18] reported that low-dose indomethacin combined with methylprednisolone was a new choice of treatment. The role of anti-infective agents is not acknowledged, but in fact, most patients had been treated with sufficient anti-infective agents before a definite diagnosis could be established. We suggest that appropriate anti-infective agents should be given according to patient’s condition.
There is no consensus on treatment duration, and relapse may occur during the period when the dosage of steroids is reduced. Sauter et al[17] reported a long duration of steroid treatment of nearly 24 mo. The major side-effects of steroids include hypertension, hyperglycaemia, immune suppression, electrolyte imbalance, and femoral head necrosis, especially in geriatric patients. The dosage and duration of steroids should be individualized according to the patient’s condition, radiological evolution and the side-effects, and more studies on treatment of AFOP are required in order to reduce the complication and improve the survival rate and the patient’s life quality.
In the present case, steroid was prescribed as soon as the diagnosis was established. Considering the old age of the patient, and to avoid potential severe side effects of high-dose steroids, an initial dose of methylprednisolone 40 mg/d was used. Fortunately, her symptoms were soon controlled. And when the dose of methylprednisolone was decreased to 24 mg/d, the improvement continued in patient’s condition and radiological evolution, and the main side-effects included hypertension and hyperglycaemia, which were resolved by antihypertensives and dietary and lifestyle modifications.
AFOP is a rare lung disease with varying morbidity and mortality, and no definitive therapy is available. The successful use of steroids in this case indicates that the pulse therapy of steroids may not be necessary. This case report adds to the literature a new choice of treatment in terms of dosage of steroids for AFOP.
This case may serve as a reminder to respiratory physicians who encounter a suspected pulmonary infection case but unresponsive to optimum antibiotic therapy in their clinical practice. Although AFOP is a rare entity, it should be considered in the differential diagnosis of pulmonary infection unresponsive to optimum antibiotic therapy. On the other hand, AFOP might be under diagnosed and under reported especially in the developing countries due to the complicated means of obtaining a tissue diagnosis which are not routinely performed in the community and secondary hospitals. Our case is distinct. The patient was an 81-year-old woman and she had a good response to short-term steroid treatment. The last follow-up showed that no relapse occurred during tapering steroids. This case will contribute to a better understanding of the treatment of AFOP in geriatric patients, and provide a new choice of dosage and duration of it. Further more studies are needed to describe various clinical aspects of this rare disease.
| 1. | Beasley MB, Franks TJ, Galvin JR, Gochuico B, Travis WD. Acute fibrinous and organizing pneumonia: a histological pattern of lung injury and possible variant of diffuse alveolar damage. Arch Pathol Lab Med. 2002;126:1064-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 2. | Travis WD, Costabel U, Hansell DM, King TE Jr, Lynch DA, Nicholson AG, Ryerson CJ, Ryu JH, Selman M, Wells AU, Behr J, Bouros D, Brown KK, Colby TV, Collard HR, Cordeiro CR, Cottin V, Crestani B, Drent M, Dudden RF, Egan J, Flaherty K, Hogaboam C, Inoue Y, Johkoh T, Kim DS, Kitaichi M, Loyd J, Martinez FJ, Myers J, Protzko S, Raghu G, Richeldi L, Sverzellati N, Swigris J, Valeyre D; ATS/ERS Committee on Idiopathic Interstitial Pneumonias. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2232] [Cited by in RCA: 3117] [Article Influence: 239.8] [Reference Citation Analysis (0)] |
| 3. | Cincotta DR, Sebire NJ, Lim E, Peters MJ. Fatal acute fibrinous and organizing pneumonia in an infant: The histopathologic variability of acute respiratory distress syndrome. Pediatr Crit Care Med. 2007;8:378-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Prahalad S, Bohnsack JF, Maloney CG, Leslie KO. Fatal acute fibrinous and organizing pneumonia in a child with juvenile dermatomyositis. J Pediatr. 2005;146:289-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | López-Cuenca S, Morales-García S, Martín-Hita A, Frutos-Vivar F, Fernández-Segoviano P, Esteban A. Severe acute respiratory failure secondary to acute fibrinous and organizing pneumonia requiring mechanical ventilation: a case report and literature review. Respir Care. 2012;57:1337-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Hariri LP, Unizony S, Stone J, Mino-Kenudson M, Sharma A, Matsubara O, Mark EJ. Acute fibrinous and organizing pneumonia in systemic lupus erythematosus: a case report and review of the literature. Pathol Int. 2010;60:755-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Valim V, Rocha RH, Couto RB, Paixão TS, Serrano EV. Acute fibrinous and organizing pneumonia and undifferentiated connective tissue disease: a case report. Case Rep Rheumatol. 2012;2012:549298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Hwang DM, Chamberlain DW, Poutanen SM, Low DE, Asa SL, Butany J. Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol. 2005;18:1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 251] [Cited by in RCA: 248] [Article Influence: 11.8] [Reference Citation Analysis (1)] |
| 9. | Ribera A, Llatjós R, Casanova A, Santin M. Chlamydia pneumoniae infection associated to acute fibrinous and organizing pneumonia. Enferm Infecc Microbiol Clin. 2011;29:632-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kobayashi H, Sugimoto C, Kanoh S, Motoyoshi K, Aida S. Acute fibrinous and organizing pneumonia: initial presentation as a solitary nodule. J Thorac Imaging. 2005;20:291-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Vasu TS, Cavallazzi R, Hirani A, Marik PE. A 64-year-old male with fever and persistent lung infiltrate. Respir Care. 2009;54:1263-1265. [PubMed] |
| 12. | Merrill AL, Smith H. Myelodysplastic syndrome and autoimmunity: a case report of an unusual presentation of myelodysplastic syndrome. Case Rep Hematol. 2011;2011:560106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Sverzellati N, Poletti V, Chilosi M, Casoni G, Hansell D, Zompatori AM. The crazy-paving pattern in granulomatous mycosis fungoides: high-resolution computed tomography-pathological correlation. J Comput Assist Tomogr. 2006;30:843-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Lee SM, Park JJ, Sung SH, Kim Y, Lee KE, Mun YC, Lee SN, Seong CM. Acute fibrinous and organizing pneumonia following hematopoietic stem cell transplantation. Korean J Intern Med. 2009;24:156-159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Alici IO, Yekeler E, Yazicioglu A, Turan S, Tezer-Tekce Y, Demirag F, Karaoglanoglu N. A case of acute fibrinous and organizing pneumonia during early postoperative period after lung transplantation. Transplant Proc. 2015;47:836-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 16. | Hara Y, Shinkai M, Kanoh S, Kawana A, Rubin BK, Matsubara O, Kaneko T. Clinico-pathological analysis referring hemeoxygenase-1 in acute fibrinous and organizing pneumonia patients. Respir Med Case Rep. 2015;14:53-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Sauter JL, Butnor KJ. Expanding the spectrum of pulmonary histopathological manifestations of anti-synthetase syndrome: anti-EJ-associated acute fibrinous and organizing pneumonia. Histopathology. 2014;65:581-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Zhou CX, Tang TT, Huang LJ, Lin XL, Chen M, Bian LJ, Chen QK, Jiang SP. Methylprednisolone combined with low-dose indomethacin treating acute fibrinous and organizing pneumonia after a surgical resection of rectal adenocarcinoma: a case report and literature review. Eur Rev Med Pharmacol Sci. 2016;20:2077-2089. [PubMed] |
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared and revised according to the CARE Checklist (2013).
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Porfyridis I S- Editor: Dou Y L- Editor: Filipodia E- Editor: Wu YXJ