Published online Oct 16, 2017. doi: 10.12998/wjcc.v5.i10.384
Peer-review started: May 24, 2017
First decision: July 11, 2017
Revised: July 27, 2017
Accepted: August 2, 2017
Article in press: August 3, 2017
Published online: October 16, 2017
Processing time: 142 Days and 19.2 Hours
Surgical resection of mandible owing to benign, malignant neoplasm, osteoradionecrosis is common. The resection can be total or segmental depending on the lesion. Loss of mandibular continuity causes deviation of remaining mandibular segment towards the resected side and rotation inferiorly due to muscle pull and scar contracture affecting mastication and esthetics. Surgical reconstruction may not be always possible. Prosthetic rehabilitation plays a major role in these patients. This case series describes different types of guiding flange (GF) prosthesis with modifications for three hemimandibulectomy patients at different time interval after surgery. The article details GF prosthesis combined with physiotherapy to correct deviation of mandible thereby improving mastication, esthetics and speech and thus enhancing the quality of life.
Core tip: Mandible is a significant structure in lower third of face constituting to esthetics and functions like speech, swallowing and mastication. Surgical resection owing to various reasons disrupts these functions. Both form and function should be considered in rehabilitating hemimandibulectomy patients. This article describes prosthetic rehabilitation that comprises of different types of guiding flange prosthesis with modifications for three hemimandibulectomy patients at different time interval after surgery.
- Citation: Lingeshwar D, Appadurai R, Sswedheni U, Padmaja C. Prosthodontic management of hemimandibulectomy patients to restore form and function - A case series. World J Clin Cases 2017; 5(10): 384-389
- URL: https://www.wjgnet.com/2307-8960/full/v5/i10/384.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i10.384
Mandible is a significant structure in lower third of face constituting to function and esthetics. It is a single bone that creates peripheral boundaries of the floor of the mouth, facial form (lower third), speech, swallowing, mastication and respiration. Disruption of mandible due to trauma, surgical resection for benign and malignant neoplasm disrupts any of these functions. Both form and function should be considered in rehabilitating hemimandibulectomy patients. Loss of mandibular continuity causes deviation of the remaining mandibular segments towards the defect and rotation of the mandibular occlusal plane inferiorly due to muscle pull and scar contracture. Mandibulectomy with radical neck dissection increases this deviation. This results in facial disfigurement, loss of occlusal contact, in many cases, loss of lip competency for saliva control and to initiate the swallowing process[1]. Literature shows techniques to correct mandibular deviation that can vary from intermaxillary fixation with elastics, palatal or mandibular guiding flange (GF) prosthesis anchored on natural teeth or the dental flange[2]. The GF is probably the simplest and most useful in maintaining position of the remaining jaw[3]. This article describes different types of GF prosthesis with modifications for three hemimandibulectomy patients at different time interval after surgery.
A 36 years old male patient was referred to the hospital with the history of carcinoma left buccal mucosa for which he underwent hemimandibulectomy and modified radical neck dissection one month back and reconstructed with pectoralis major myocutaneous flap. Patient complained of difficulty in mastication and speech.
Extra oral examination revealed facial asymmetry and deviation of mandible towards the resected site and the deviation increased on opening the mouth. The mouth opening was reduced to 25 mm. Intra oral examination revealed partially edentulous mandible and loss of occlusal contact (Figure 1).The mandibular defect was classified as Cantor and Curtis Class II that is lateral resection of the mandible distal to cuspid[4]. It was noted that mandible can be guided to centric occlusion manually but the patient could not achieve this position consistently on his own. So the treatment objective was to correct the deviation of mandible and to restore proper occlusion for mastication.
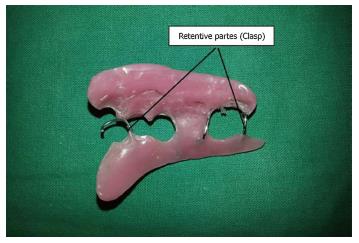
Impressions were made with modified stainless steel stock tray and irreversible hydrocolloid (Tropicalgin, IDS DENMED Pvt. Ltd.) followed by pouring cast with Type III Dental stone (Goldstone, mfg. by ASIAN CHEMICALS). Interocclusal record was made with modelling wax (the Hindustan dental products) by asking the patient to move the mandible away from resected site as far as possible and manually guiding the mandible to centric occlusion. This record was transferred to a mean value articulator. Three clasps were made using 21 gauge wire - “C” clasp on canine and premolar; adams clasp on molar for retention purpose. Considering the amount of deviation and reduced mouth opening, mandibular GF prosthesis was fabricated on the nondefect side using autopolymerising acrylic resin (DPI Cold Cure pink; Dental products of India). After applying sufficient separating medium, the resin was added on buccal and lingual aspect of nondefect side of mandible and on the buccal side the extension was till the maxillary buccal vestibule. The prosthesis was tried in patient mouth and checked for retention and stability. It was trimmed and adjusted so that the mandible is guided to centric occlusion without delivering excessive force to maxillary teeth. Acrylic resin was added little by little to the guide flange until there was smooth guidance of the mandible to proper occlusion without any interference. The prosthesis was finished and polished (Figure 2). After insertion of the prosthesis, midline coincided and occlusion was achieved (Figure 3). The patient was advised to use the GF throughout the day except at night and during meals. Physiotherapy exercises were also insisted. It included maximum mouth opening and grasping the chin to move the mandible away from surgical side. This will help in reducing trismus, minimize scar contracture and improve occlusion[1]. Review after a month, there was trivial reduction in the deviation. Hence, palatal GF prosthesis was made which wouldn’t affect esthetics.
A 49 years old male patient presented to the hospital with the complaint of difficulty in mastication and facial disfigurement for the past three years owing to carcinoma left buccal mucosa for which he underwent composite resection of mandible and reconstructed with Pectoralis major myocutaneous flap following preoperative chemotherapy and radiotherapy. On clinical examination, there was deviation of remaining mandible towards the resected site and also downward rotation of mandible. It was noted that intermaxillary fixation was not done at the time of surgery. The mandibular defect was classified as Cantor and Curtis type III[4]. Since it was resected till the midline the deviation and downward rotation of mandible was more due to loss of muscular support. The mouth opening was 35 mm. Intra oral examination revealed generalized attrition, supraeruption and partially edentulous mandible. Patient was able to bring remaining mandible to centric occlusion with guidance and he was not able to achieve this position consistently. Since mouth opening was normal compared to previous case, an acrylic GF on maxilla was planned as interim prosthesis.
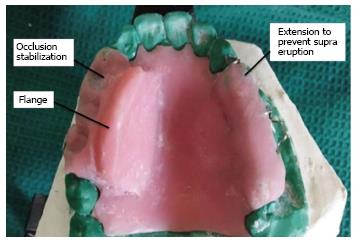
Impression, cast, interocclusal record and articulation were made following the same procedure as in case report 1. Palatal GF prosthesis was planned for this case considering the stability of prosthesis, esthetics, occlusion and downward rotation of mandible. The guide flange extended till the lingual sulcus on the nondefect side. The prosthesis was tried in patient mouth. The inclination of the guide flange was adjusted until it guided the mandible to centric occlusion (Figure 4). But as both maxillary and mandibular teeth were attrited, functional cusps were worn out. The mandibular teeth glided beyond centric occlusion. To prevent this and to train the patient in centric occlusion, the acrylic resin was extended on the palatal cusps of maxillary teeth. A functionally generated path was recorded and an occlusal table was fabricated accordingly so as to stabilize the occlusion. The occlusal table was also extended on the maxillary teeth of defect side to prevent supraeruption as there were no opposing teeth (Figures 5 and 6). The patient was recalled after a month for review.
A 35 years old male patient came to the hospital with the history of hemimandibulectomy and left maxillary alveolectomy reconstructed with masseter flap done two weeks ago owing to carcinoma left buccal mucosa. Mouth opening was noted as 30 mm. It was noted that the deviation of mandible towards the resected side was minimum as the surgery was done only two weeks ago. If intervention with the GF was not done at this time, the deviation would worsen on healing process and scar formation. The procedure of impression making, cast, interocclusal record and articulation as in case report 1 was done. As the deviation was minimum, palatal GF prosthesis was planned for this case. As opposing teeth were present in the mandibular arch, the risk of supraeruption is nil. The prosthesis extended till the lingual sulcus on palatal non resected side. The prosthesis was tried in patient mouth and trimmed accordingly (Figure 7). The patient was able to guide the mandible into pre-existing occlusion (Figure 8). The patient was advised to wear the flange at all times except while eating and during nights and was asked to review after one week.
Segmental resection of mandible results in deviation of remaining segment towards the resected side due to uncompensated influence of contralateral musculature, particularly the internal pterygoid muscle. If this influence is uncompensated, the contraction of cicatricial tissue will fix the residual fragment in its deviated position[5]. The rotation of residual mandible in an inferior direction is caused by the pull of suprahyoid musculature and gravity due to loss of anchorage of elevator muscles[1]. The pathway of closure in a lateral resection of mandible starts from its medial, retruded position and closes in an upward diagonal manner into an occlusion which may or may not correspond with the patient’s preoperative occlusion[6]. The amount of deviation and downward rotation depends on the extent of tissue loss. The more the mandible remaining, the better is the prosthetic prognosis. Retention of mandibular cuspids is especially beneficial[4].
The basic objective in rehabilitation is retraining the remaining mandibular muscles to provide an acceptable maxillo-mandibular relationship of the remaining portion of the mandible[7]. This would permit occlusion of remaining natural teeth or control of residual edentulous segments to provide for the reasonable placement and acceptable occlusion of the artificial teeth[7]. There are four significant factors that affect rehabilitation: The location and extent of surgery, the effect of radiation therapy, the presence or absence of teeth and the psychological aspect[6].
The time of initiation of the treatment is the key to success for restoring the form and function. The deviation after hemimandibulectomy will be difficult to correct after the healing phase of 6 to 8 wk due to scar contracture and the muscles adapting to this cicatricial tissue[1]. Patients usually have trismus following the surgery which will be a challenge for making an impression of maxilla and mandible. Hence preoperative casts should be advocated for all patients so that exact maxillo-mandibular relationship can be obtained postoperatively. Intermaxillary fixation can be advocated at time of surgery but for dressings and irrigation, it would be more advantageous to enable the patient to open and close the mouth. Temporary retainers can be made preoperatively so that it can immediately placed after surgery[8]. Robinson stated that temporary acrylic GF can be inserted on the third postoperative day[5]. In the above cases intermaxillary fixation was not done at the time of surgery and preoperative impressions were not made as they were referred only after surgery.
Physiotherapy is recommended to reduce trismus and to loosen scar contracture. Without this, masticatory ability may decrease and lateral movement toward the nonresected side may not be possible[9]. It must be started two weeks postoperatively. Patient is asked to gently push the mandible away from the defect toward more normal position. While holding mandible in position, the patient should open the mouth as wide as possible to stretch the musculature at the resection site[1,4]. In all the three cases, physiotherapy was insisted.
Various literature shows different techniques for managing the deviation that include cast metal guidance prosthesis which is more technique sensitive, time consuming, expensive and require more number of patient visits. Acrylic GF is comparatively simple in design, cost effective, less patient visit and more importantly the ease of adjustability[10].
A common complaint without such an appliance is pain in the remaining temperomandibular joint which results from the abnormal position of the condyle[8]. Definitive treatment of these patients takes at least a year from the date of surgery as definitive treatment requires complete healing and no recurrence of cancer. Till then the acrylic GF prosthesis can be used as a training device for mandibular movements and to avoid further compilations.
In the cases presented above, acrylic GF was used as a training prosthesis. Out of three patients, one patient was referred immediately after surgery, one patient five years after surgery and other patient one month after surgery. In the first and third case report, resection was distal to canine. The amount of deviation was more in the first patient as the patient reported one month after surgery, mandibular GF was given for a period of three weeks later replaced with maxillary GF. The amount of deviation was trivial in the third patient as he reported one week following surgery, maxillary GF was given. In the second case report, the downward rotation of mandible was significant as the resection involved mandibular canine. For this case, maxillary GF was given with functionally generated occlusal table on non-defect side. For all the three patients, physiotherapy was insisted along with the insertion of GF. The patients had pain only due to scar contractures and deviation leading to pain on mandibular movements. This was addressed by correcting the deviation, and trying to maintain a stable occlusion. Guideline for GF is listed in Table 1.
| Based on time of referral | ||
| 1 | Before surgery - 1 wk post-surgery | Intermaxillary fixation done with elastics |
| 2 | 1 wk post-surgery - 1 mo | GF prosthesis and Physiotherapy |
| 3 | 1 mo - 1 yr | Active physiotherapy, Counseling followed by GF prosthesis |
| 4 | > 1 yr | Surgical intervention |
| Based on amount of tissue resected | ||
| 1 | Amount of hard and soft tissue | Directly influences success and difficulty in rehabilitation |
| 2 | Segmental resection of mandible distal to cuspid | Maxillary or Mandibular GF |
| 2 | Segmental resection of mandible that involves canine | Maxillary GF is the choice as the loss of mandibular canine results in more downward rotation of mandible and the mandibular GF might not be stable |
| Types of prosthesis | ||
| 1 | Acrylic GF | Immediately after surgery and as training prosthesis |
| 2 | Definitive Cast metal GF | One year after training prosthesis |
| Modifications | ||
| 1 | To prevent supraeruption | Occlusal table on Maxillary teeth on defect side |
| 2 | To stabilize occlusion | Functionally generated occlusal table on Maxillary teeth on nondefect side |
| Intervention | Prognosis | |
| 1 | From the time of planning and surgery | Better |
| 2 | Long time interval after surgery | Guarded |
Rehabilitation is an essential phase of cancer care and should be considered from the time of diagnosis in a complete and comprehensive treatment plan. The primary objective is restoration of function and appearance. GF prosthesis serves both the purpose. This article gives a comprehensive explanation about rehabilitation procedures carried out for three patients who were surgically treated for carcinoma with hemimandibulectomy and neck dissection.
All three cases complained of difficulty in mastication and facial disfigurement following hemimandibulectomy reconstructed with flap.
All three cases showed deviation of mandible towards the resected site, los of lip competency and occlusal contact and reduced mouth opening.
Guiding flange (GF) prosthesis to correct deviation of mandible and to stablise occlusion enhancing mastication and esthetics.
GF prosthesis guides the remaining mandible to proper and stable occlusion and trains the mandibular movements after hemimandibulectomy.
The time of initiation of treatment is the key to success. A common complaint without such prosthesis is pain in temperomandibular joint. This GF prosthesis alleviates pain and can be used as training device for mandibular movements after surgery.
This is a well written manuscript exposing the experience of the authors in such particular field.
We thank the Department of surgical oncology, Government Royapettah hospital, Chennai, India and the Department of Plastic surgery, Rajiv Gandhi Government General hospital, Chennai, India for their valuable support.
| 1. | Taylor TD. Diagnostic considerations for Prosthodontic rehabilitation of the mandibulectomy patient. In: Clinical Maxillofacial Prosthetics, Chicago: Quintessence publishing 2000; 155-170. |
| 2. | Schneider RL, Taylor TD. Mandibular resection guidance prostheses: a literature review. J Prosthet Dent. 1986;55:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Edgerton M, Pyott J. Surgery and prosthesis in Jaw reconstruction. J Prosthet Dent. 1954;4:257-262. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Robinson JE, Rubright WC. Use of guide plane for maintain the residual fragment in partial or hemimandibulectomy. J Prosthet Dent. 1964;14:992-999. [RCA] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Curtis TA, Cantor R. The forgotten patient in maxillofacial prosthetics. J Prosthet Dent. 1974;31:662-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Desjardins RP. Occlusal considerations for the partial mandibulectomy patient. J Prosthet Dent. 1979;41:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ackerman AJ. The prosthetic management of oral and facial defects following cancer surgery. J Prosthet Dent. 1955;5:413-432. [RCA] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 43] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Sahin N, Hekimoğlu C, Aslan Y. The fabrication of cast metal guidance flange prostheses for a patient with segmental mandibulectomy: a clinical report. J Prosthet Dent. 2005;93:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Kar S, Tripathi A, Madhok R. Treatment outcome with guiding flange prosthesis in hemimandibulectomy patients: Case series of three patients. Ann Maxillofac Surg. 2015;5:266-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: India
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Alimehmeti RH, Fourtounas C, Wang F S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ