Published online Sep 16, 2015. doi: 10.12998/wjcc.v3.i9.853
Peer-review started: March 24, 2015
First decision: May 13, 2015
Revised: May 30, 2015
Accepted: June 30, 2015
Article in press: July 2, 2015
Published online: September 16, 2015
Processing time: 178 Days and 19.3 Hours
Primary adrenal myelolipoma is a rare, non-functioning adrenal benign tumor that is composed of mature adipose tissue and a variable amount of haemopoietic elements. Clinically, it is difficult to get diagnosed with adrenal myelolipoma because the patient usually doesn’t have obvious symptoms and signs in early stage. In the present study, two cases of primary bilateral adrenal myelolipomas are reported. Clinical presentation, imaging diagnostic features, histopathological changes and surgical treatments of the two patients are discussed. Preoperative diagnostic imaging examinations (B-mode ultrasonography, computed tomography and magnetic resonance imaging sans) assisted getting a prediction diagnosis of bilateral adrenal myelolipomas. A two-stage surgery was used to successfully excise bilateral adrenal myelolipomas in the two patients. Conventional open adrenalectomy was applied to remove the adrenal myelolipomas greater than 6 cm, and laparoscopic adrenalectomy was performed to excise the adrenal tumors smaller than 6 cm. Bilateral adrenal myelolipomas of the two patients were finally confirmed by postoperative histopathological examinations. Understanding clinical, imaging diagnostic and histopathological features of bilateral adrenal myelolipomas will facilitate timely diagnosis and treatment of this condition. Surgical removal of bilateral adrenal myelolipomas is safe, curative and beneficial. The two-stage surgery appears to be the best treatment option for the patients with bilateral adrenal myelolipomas because it achieves optimal treatment effectiveness with minimized sequelae.
Core tip: Adrenal myelolipoma is a rare adrenal benign tumor. It is not easy to get diagnosed with the tumor due to lack of obvious clinical symptoms and signs in early stage. This report discusses clinical, imaging diagnostic and histopathological features in two patients with bilateral adrenal myelolipomas as well as a two-stage surgical strategy for removal of the adrenal tumors. Understanding clinical, imaging diagnostic and histopathological features of bilateral adrenal myelolipomas will facilitate timely diagnosis and treatment of this condition.
- Citation: Yang Y, Ye LY, Yu B, Guo JX, Liu Q, Chen Y. Two case reports of bilateral adrenal myelolipomas. World J Clin Cases 2015; 3(9): 853-860
- URL: https://www.wjgnet.com/2307-8960/full/v3/i9/853.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i9.853
Adrenal myelolipoma is a rare, benign, non-functional neoplasm of adrenal gland, which is composed of mature adipose tissue and a variable amount of haemopoietic elements. Myelolipoma is usually found to occur in unilateral adrenal gland, and rarely observed in bilateral adrenal glands[1-4]. Generally, bilateral adrenal myelolipomas are not easy to be diagnosed clinically because the patients have no obvious symptoms and don’t feel pain or discomfort in the early stages of the disease. Over the last few decades, a definite diagnosis of adrenal myelolipoma could be made only with certainty at autopsy. Overall diagnosis rate of adrenal myelolipoma, which was made with autopsy, was merely 0.08%-0.2%[3,5]. In recent years, the diagnosis rate of adrenal myelolipoma has been significantly improved due to the development of modern imaging technologies [such as ultrasound, computed tomography (CT) and magnetic resonance imaging (MRI)]. In the present study, two cases of bilateral adrenal myelolipomas that have been treated successfully in our hospital are reported. The clinical, diagnostic imaging and histopathohistological features of the two cases are retrospectively analyzed. A two-stage surgical strategy for removal of bilateral adrenal myelolipomas is discussed.
History and physical examination: Patient A is a 40-year-old male, without family history of genetic diseases and smoking or drinking habits. His adrenal masses were found by B-mode ultrasound scanning while he had a regular health check-up in our hospital. He was admitted to the hospital after diagnosed with “left adrenal mass (tumor)”. The patient had no other obvious symptoms. A thorough history and physical examination were indicated to rule out diabetes, hypertension, coronary heart disease, hepatitis and tuberculosis. Grade I hypertrophy of the prostate gland was found by prostate examination using rectal palpation technique. Patient’s prostate gland was soft and spongy, but the central sulcus became shallow. Neither abnormal prostatic nodules nor rectal bleeding were found by prostate examination.
Diagnostic imaging: In order to establish a diagnosis, the patient was scanned with B-mode ultrasound, CT and MRI scans. The B-mode ultrasound scanning was done on the patient who was placed in the lateral or supine position using a Nemio 30 scanner with a 3.5- to 5-MHz curved linear transducer. A Picker PQ 6000 Spiral CT scanner with a slice thickness of 3-6 mm was used to scan the entire kidney of the patient. The patient’s kidneys were also scanned using a Siemens Sensation 3.0T MRI scanner. Acquisitions included axial TSE/T2WI and FL/T1WI, and coronal TFI/T2WI sequences. The results of imaging scans (such as the density, signal strength, size, shape and location of a renal mass) were evaluated by two radiologists, respectively.
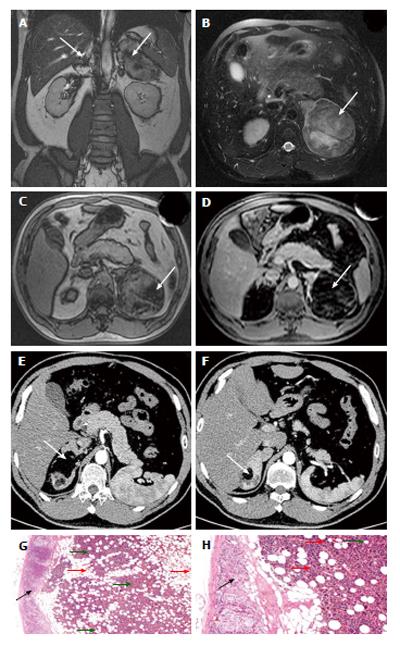
Both the left and right adrenal masses were simultaneously detected by diagnostic imaging examinations while the patient was hospitalized. Two hyper-echoic masses were observed by B-mode ultrasonography in the left and right adrenal glands. The sizes of the two hyperechoic masses were 9.7 cm × 9.5 cm in the left adrenal gland and 3.3 cm × 2.3 cm in the right adrenal gland, respectively. All masses had clear boundary and a regular shape. Color doppler flow imaging (CDFI) showed little scattered blood flow signals within the masses. CT showed a mixed density area of 9 cm × 10 cm with the absorption values ranging from 80-120 HU in the left adrenal gland, and a mixed density area of 3.5 cm × 5.5 cm with the absorption values ranging from 90-100 HU in the right adrenal gland, suggesting fat-density lesions in bilateral adrenal glands. MRI scan showed multiple round masses with unequal signals on both T1 and T2 in the left adrenal gland. The multiple round masses made the left kidney to shift downward. Among these masses, the biggest one was located in the posterior side of left adrenal gland and its size was about 8.69 cm × 7.82 cm. An enlargement of the medial limb of the right adrenal gland was also observed using MRI scan (Figure 1A-D).
After removal of the left adrenal myelolipoma, there were no obvious abnormalities found by B-mode ultrasonography in the left adrenal gland. However, B-mode ultrasonography showed a hyperechoic mass of 3.6 cm × 3.5 cm in the right adrenal gland. Both plain non-contrast and contrast-enhanced CT scans revealed that the multiple round masses had vanished from the left adrenal gland after surgery, but an irregular mass with clear boundary appeared in the right adrenal gland. The mass, which looked like a multilocular cystic lesion, had a mixed density area (mixed with fat-density and high-density shadows) with the average absorption values of 7-13 HU (Figure 1E and F).
Surgery: A two-stage surgery was carried out in the patient to excise bilateral adrenal myelolipomas. Because the patient had a large myelolipoma in left adrenal gland and a small myelolipoma in right adrenal gland, a conventional open adrenalectomy was employed to remove the large myelolipoma in his left adrenal gland in first stage of surgery. During surgery, the patient was placed in supine position to make an abdominal incision after anesthesia. After excised the left adrenal myelolipoma, the resected myelolipoma with a total volume of 11 cm × 8.5 cm × 6 cm was sent to the pathology laboratory for histopathological examination. The right adrenal myelolipoma was removed through laparoscopic adrenalectomy in second stage of surgery (10 mo later). The myelolipoma removed from right adrenal gland had an intact capsule and its total volume was 4.0 cm × 4.0 cm × 3.3 cm. A tumor tissue of 2.5 cm × 2.0 cm × 2.5 cm with the color mixing gray and red was observed inside the removed myelolipoma. Following the surgery, as a regular procedure, the indwelling urinary catheters and nasogastric tubes were kept in until the patients’ urinary and gastrointestinal functions returned to normal. The patient was observed daily from the first postoperative day until discharge by the surgeon. Meanwhile, changes in the electrocardiogram (ECG), blood pressure, and blood oxygen saturation were continuously monitored. Anti-inflammatory drugs, symptomatic treatments and supportive care were provided to the patient.
Histopathology: All resection specimens of adrenal myelolipomas were examined by the pathologists using H and E staining (which was repeated twice on resection specimens). Tumor-like masses of extramedullary hematopoietic tissue were composed of adipose cells and hematopoietic cells. Fat vacuoles could be seen in adipose tissue. Among adipose cells, there were medullary cells, megakaryocytes, erythrocytes and lymphoid cells with different maturity levels among fat cells. The histopathological examination results confirmed the initial diagnosis of bilateral adrenal myelolipomas in this patient (Figure 1G and H).
Post-treatment follow-up: Follow-up data were unavailable because this patient did not schedule any post-hospital follow-up visits after he was discharged from the hospital.
History and physical examination: Patient B is a 73-year-old male with diabetes for 14 years, but without family history of genetic diseases and smoking or drinking habits. A thorough history and physical examination were indicated to rule out hypertension, coronary heart disease, hepatitis and tuberculosis. He underwent transurethral resection of the prostate years earlier. The patient was diagnosed with bilateral renal cysts in 2009 but didn’t receive further medical interventions after bilateral renal space-occupying lesions were observed during a routine physical examination. He was admitted to the hospital for further treatment after his bilateral renal space-occupying lesions were diagnosed again on B mode ultrasonography in 2011. The patients didn’t have either obvious clinical symptoms or any discomfort when he was admitted to the hospital. Grade II hypertrophy of his prostate gland was found by prostate examination using rectal palpation technique. Patient’s prostate gland felt hard, but didn’t have palpable nodules or shallow/disappeared central sulcus.
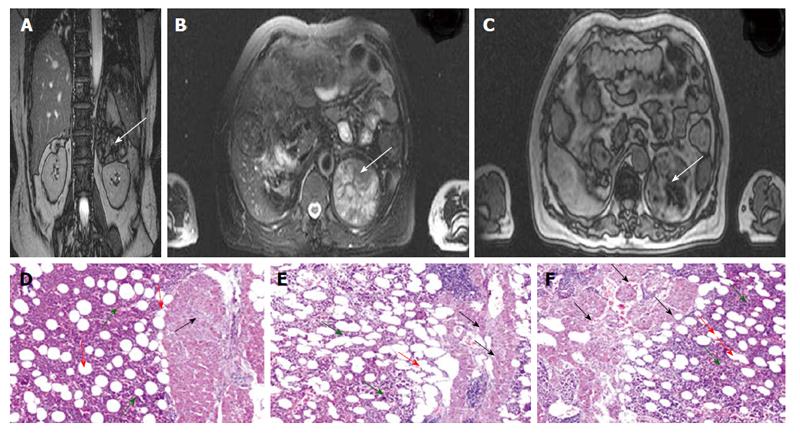
Diagnostic imaging: Patient B was examined with B-mode ultrasound, CT and MRI, respectively. The B-mode ultrasound scanning was done on using the Nemio 30 scanner with a 3.5- to 5-MHz curved linear transducer. The patient’s kidneys were scanned by both the Picker PQ 6000 Spiral CT scanner with a slice thickness of 3-6 mm and the Siemens Sensation 3.0T MRI scanner. The medium-to-hyper echo complex masses were observed by B-mode ultrasonography in bilateral adrenal glands of the patient. The masses, which had clear boundary and regular shapes, were 8.8 cm × 7.5 cm on the left side and 9.0 cm × 8.8 cm on the right side, respectively. CDFI showed no obvious blood flow signals within the masses. CT scan found two fat-density shadows in bilateral adrenal glands, which sizes were 10.1 cm × 7.2 cm and 7.3 cm × 7.9 cm, respectively. Contrast-enhanced CT scanning made the two shadows become more inhomogeneous with a mild-to-moderate increasing density. MRI scan showed many masses in his bilateral adrenal glands. In the right adrenal gland, the largest volume of the masses was 8.7 cm × 9.97 cm × 4.92 cm and the smallest volume was 4.45 cm × 4.26 cm × 4.92 cm. In the left adrenal gland, the average volume of the masses was 7.74 cm × 7.52 cm × 4.58 cm. In MR images, the signals of these masses were non-uniform, which included a large number of signals generated by mature fat cells and intracellular lipid contents. After the right adrenal myelolipoma was removed in first stage, the MRI exam was performed again in this patient (Figure 2A-C). A round lesion with mixed signals on T1 and T2 (short T1 mixed with slightly longer T2) was found in the left adrenal gland. The lesion was characterized by decreased signal intensity in the antiphase (out-of-phase). Its size was about 7.46 cm × 7.82 cm. The upper pole region of the left kidney was found to be pressed by the lesion. The right adrenal gland still showed mixed signals on MRI (with both longer T1 and longer T2) and had unclear appearance of an anatomical structure. No lesion near the left retroperitoneal abdominal aorta was observed.
Surgery: The two-stage surgery was also carried out in patient B to excise his bilateral adrenal myelolipomas. Because the patient had large myelolipomas in both the left and right adrenal glands, a conventional open adrenalectomy was used to resect his bilateral myelolipomas. In contrast to patient A, the patients B’s right adrenal myelolipoma was removed first, and his left adrenal myelolipoma was resected 3 mo later. In the first surgical procedure, an adrenal myelolipoma measuring 4.5 cm × 3.5 cm × 3.0 cm was removed from the right adrenal gland. Another adrenal myelolipoma measuring 9.0 cm × 7.0 cm × 4.5 cm was excised from the left adrenal gland in the second surgical procedure. After surgery, changes in the ECG, blood pressure, and blood oxygen saturation were continuously monitored in the patient. Anti-inflammatory drugs, symptomatic treatments and supportive care were also given to the patient. The patient had a good outcome after surgery.
Histopathology: All resection specimens of adrenal myelolipomas were examined by the pathologists using H and E staining (which was repeated twice on resection specimens). The histopathological examination of surgical excised specimens showed large amounts of tumor-like adipose tissue existed in bilateral adrenal medullas, in which extramedullary hematopoietic tissues were found to present. In addition, a thin layer of adrenal cortical tissues was found to surround the myelolipoma. These morphological changes corresponded to the typical histopathological features of adrenal myelolipoma, and confirmed the initial diagnosis of adrenal myelolipoma (Figure 2D-F).
Post-treatment follow-up: Follow-up data were unavailable because this patient did not schedule any post-hospital follow-up visits after he was discharged from the hospital.
Adrenal myelolipoma is a rare, benign and hormonally inactive neoplasm of adrenal gland. It occurs generally in unilateral adrenal gland, but the left and the right affected equally. As a benign tumor, myelolipoma does not spread to other body parts. Sometimes, a larger myelolipoma may cause localized tissue death and bleeding. The well-recognized complication of adrenal myelolipoma is spontaneous retroperitoneal haemorrhage[6]. Adrenal myelolipoma, which is composed of large amounts of fat and myeloid tissues, is shaped like or nearly like a round and has clear boundary. Based on its tissue components, adrenal myelolipoma can be categorized into three types: adipose tissue, myeloid tissue and a combination of both[7,8]. Primary bilateral adrenal myelolipoma is rarely observed in clinical practice[3,9,10]. In histopathology of bilateral adrenal myelolipoma, the tissue type of the left adrenal myelolipoma is usually the same as that of the right adrenal myelolipoma but it can’t rule out the possibility that different tissue types of adrenal myelolipomas may exist in the left and right adrenal glands, respectively.
As early as 1905, Gierke et al[11] have begun to study adrenal myelolipoma. However, the etiology and pathogenesis of adrenal myelolipoma still remain unclear until now. Adrenal myelolipoma has been considered as a result of the differentiation of adrenal medullary or cortex cells into adipose tissue and extramedullary hematopoietic tissue in adrenal gland, which is caused by stimulation of some harmful factors such as stress, infection, ischemia, necrosis, etc.[12]. Some studies suggested that adrenal myelolipoma might result from ectopic proliferation of myeloid cells that started to occur during the embryonic period in adrenal gland[13,14]. Moreover, some researchers proposed that the tumor might be evolved from a nonfunctioning adrenal cortical adenoma[15]. As compared to unilateral adrenal myelolipoma, bilateral adrenal myelolipoma might involve more complicated pathogenic mechanism[16].
Generally, there are no specific clinical signs and symptoms observed in the patients with adrenal myelolipoma[3], and also no marked gender differences in the incidence rates of adrenal myelolipoma. It is difficult to predict the incidence of adrenal myelolipoma and to accurately identify the potential patients in the population, because so far there are not many cases to be reported worldwide. Currently, it is unavailable to obtain the authoritative statistical data about the incidence of adrenal myelolipoma. Adrenal myelolipoma is usually discovered by accident while a physical examination is performed in the patients who have suffered other types of diseases. These patients have almost no noticeable manifestations of adrenal gland disorders or endocrine disorders. A diagnosis of adrenal myelolipoma depends mainly on preoperative diagnostic imaging screening, localization and qualitative assessment[7,17,18].
B-mode ultrasonography can be employed to only screen adrenal myelolipoma, because it has limited application in the identification of the tumors that are smaller than 2 cm in diameter. CT scan, especially thin-section CT scan, could be a sensitive imaging technology to diagnose adrenal myelolipoma. However, CT signals of the adrenal masses may be doped with complicated and undesired signals from other biological components because fat tissue inside an adrenal mass is often mixed with other biological components such as calcified and hemorrhagic soft tissues. This may result in incorrect imaging information about the mass, thus leading to a wrong diagnosis.
As compared with CT scan, MRI scan is more sensitive and more accurate imaging diagnostic tool for adrenal tumors. MRI delineates soft tissue better than CT, promoting greater accuracy in preoperative assessment of adrenal myelolipoma. It can also help make a precise quantitative evaluation of adrenal masses through a comparison of unenhanced and contrast-enhanced scans. Under the unenhanced MRI scans, the masses with high proportion of fat tissue show high signal intensity on T1 and T2-weighted images. After contrast enhancement, the signal intensity of the adipose-rich masses will remain the same without any change on MRI. This will be most useful to distinguish adrenal myelolipoma from other adrenal lesions. In addition, MRI scan offers substantial advantages over CT scan for precisely locating a myelolipoma within the adrenal gland, because it uses a strong magnetic field to create high-resolution 3D images of the tumor.
Preoperative diagnostic imaging localization of an abdominal mass is most important in the differential diagnosis of adrenal myelolipoma. It will distinguish adrenal myelolipoma from renal angiomyolipoma, retroperitoneal liposarcoma and other types of abdominal masses. Therefore, MRI is very helpful to establish an accurate diagnosis of adrenal myelolipoma and to develop the surgical strategy for the treatment of this condition. Although diagnostic imaging examinations are generally effective in quantitative evaluation and diagnostic localization of adrenal myelolipoma, a final diagnosis can be made only after histopathological examinations reveal the existence of adrenal myelolipoma in the resection specimens.
Surgical removal of an adrenal myelolipoma is safe, curative and beneficial. However, surgical strategy may depend on the nature, grade, size and location of the myelolipoma[19,20]. When the patients have tumors larger than 3.5 cm in diameter or fast-growing tumors, surgical resection should be the best choice for treatment of adrenal myelolipoma. For an adrenal tumor smaller than 6 cm in diameter, laparoscopic adrenalectomy is generally recommended because this procedure provides patients with a faster recovery and less post-operative pain. However, if an adrenal tumor is greater than 6 cm in diameter or is very likely to grow quickly from its imaging characteristics, the appropriate surgical approach is a conventional open adrenalectomy.
Unlike that for unilateral adrenal myelolipoma, surgical strategy for bilateral adrenal myelolipoma needs to consider how to maximize both the preservation of the adrenal glands and the restoration of the adrenal function. If bilateral adrenal myelolipomas are removed at the same time, it will be inevitable that some of normal adrenal tissues are excised from both the left and right adrenal glands. This will cause bilateral adrenal insufficiency and serious postoperative complications. Therefore, the two-stage surgery should be the best treatment option for bilateral adrenal myelolipoma. Bilateral adrenal myelolipomas can be removed separately in two different stages of surgery at different times[19,21,22]. The reason for performing the two-stage surgery in the patients with bilateral adrenal myelolipoma is that the surgery can be done in a short time and causes less damage to the patients, thus reducing the risk of surgery and enhancing rapid surgical recovery. Most importantly, the two-stage surgical strategy can minimize the chance of adrenal crisis and postoperative complications.
In the present study, the two-stage surgery was successfully performed in the two patients with bilateral primary adrenal myelolipoma. Because patient A had both a large left adrenal myelolipoma and a small right adrenal myelolipoma, a conventional open adrenalectomy was employed to remove his left adrenal myelolipoma in first stage of surgery, and a laparoscopic adrenalectomy was used to excise his right adrenal myelolipoma in second stage of surgery (10 mo later). The conventional open adrenalectomy was employed to resect the patients B’s myelolipomas in both left and right adrenal glands because this patient had large myelolipomas in both left and right sides. In contrast to patient A, the patients B’s right adrenal myelolipoma was removed first, and his left adrenal myelolipoma was resected 3 mo later. There was no adrenal crisis or other complication to be observed in the patients after surgery. The two-stage surgical strategy has been proven to achieve optimal treatment effectiveness with minimized sequelae.
A combination of B-mode ultrasonography, CT and MRI sans is the effective diagnostic approach to detect bilateral adrenal myelolipoma. However, before surgery, the quantitative evaluation and diagnostic localization of an adrenal myelolipoma may depend on not only the diagnostic imaging examinations, but also medical histories, clinical symptoms and signs, physical exams and laboratory tests. Surgical strategy for removal of bilateral adrenal myelolipoma should be created based on the nature, grade, size and location of the tumor. Two-stage surgical removal of bilateral adrenal myelolipoma could be the best treatment scheme to achieve optimal treatment effectiveness with minimized sequelae.
Rare bilateral adrenal masses were found in two patients.
Bilateral adrenal myelolipomas, without obvious clinical symptoms and signs.
Retroperitoneal liposarcoma, renal angiomyolipoma, fat containing adrenocortical carcinoma and adrenal teratoma.
Laboratory examinations revealed normal results.
B-mode ultrasonography, computed tomography and magnetic resonance imaging revealed the presence of bilateral adrenal myelolipomas.
Postoperative histopathological examinations confirmed finally the diagnosis of bilateral adrenal myelolipomas in the two patients.
Bilateral adrenal myelolipomas were successfully resected using a two-stage surgical treatment scheme.
Few cases of bilateral adrenal myelolipomas were reported with similar clinical presentation, imaging diagnostic features and surgical treatment.
A two-stage surgery is an operative procedure in which bilateral myelolipomas are resected separately from the left and right adrenal glands in two different stages of surgery at different times. One myelolipoma in unilateral (the left or right) adrenal gland is excised in first stage of surgery, and another myelolipoma in the contralateral adrenal gland will be removed in second stage of surgery (a couple of months later). It is a satisfying treatment scheme to achieve optimal treatment effectiveness with minimized sequelae.
Understanding clinical, imaging diagnostic and histopathological features of bilateral adrenal myelolipomas will facilitate timely diagnosis and treatment of this condition. Two-stage surgical removal of bilateral adrenal myelolipomas appears to be the best treatment option for the patients.
At the outset, the authors are requested to rectify certain typographical errors which are present in the manuscript. The authors are requested to incorporate literature data concerning other reported cases of bilateral adrenal myelolipoma in respect to investigative and surgical methods. This will be helpful in determining the appropriate diagnostic and treatment modalities.
| 1. | Alvarez JF, Goldstein L, Samreen N, Beegle R, Carter C, Shaw A, Ben-David K. Giant adrenal myelolipoma. J Gastrointest Surg. 2014;18:1716-1718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Daneshmand S, Quek ML. Adrenal myelolipoma: diagnosis and management. Urol J. 2006;3:71-74. [PubMed] |
| 3. | Gershuni VM, Bittner JG, Moley JF, Brunt LM. Adrenal myelolipoma: operative indications and outcomes. J Laparoendosc Adv Surg Tech A. 2014;24:8-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Zhang Z, Kong CZ, Guo KF. Diagnosis and treatment of bilateral adrenal tumor. J Hebei Med Pharm. 2014;36:222-225. |
| 5. | Musante F, Derchi LE, Zappasodi F, Bazzocchi M, Riviezzo GC, Banderali A, Cicio GR. Myelolipoma of the adrenal gland: sonographic and CT features. AJR Am J Roentgenol. 1988;151:961-964. [PubMed] |
| 6. | Lawler LP, Pickhardt PJ. Giant adrenal myelolipoma presenting with spontaneous hemorrhage. CT, MR and pathology correlation. Ir Med J. 2001;94:231-233. [PubMed] |
| 7. | Liu T, Ping JL, Wang WG. Imaging and pathological basis of adrenal myelolipoma. J Pract Radiol. 2004;20:1093-1096. |
| 8. | Zheng MW, Ge YL, Huan Y, Shi MG, Zhang JS. CT imaging diagnosis of adrenal myelolipoma. J Pract Radiol. 2002;18:966-967. |
| 9. | Ketelsen D, von Weyhern CH, Horger M. Diagnosis of bilateral giant adrenal myelolipoma. J Clin Oncol. 2010;28:e678-e679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Wrightson WR, Hahm TX, Hutchinson JR, Cheadle W. Bilateral giant adrenal myelolipomas: a case report. Am Surg. 2002;68:588-589. [PubMed] |
| 11. | Gierke E. Ueber Knochenmarksgewebe in der Nebenniere Beitr. Pathol Anat. 1905;37:311-325. |
| 12. | Wagner JR, Kleiner DE, Walther MM, Linehan WM. Perirenal myelolipoma. Urology. 1997;49:128-130. [PubMed] |
| 13. | El-Mekresh MM, Abdel-Gawad M, El-Diasty T, El-Baz M, Ghoneim MA. Clinical, radiological and histological features of adrenal myelolipoma: review and experience with a further eight cases. Br J Urol. 1996;78:345-350. [PubMed] |
| 14. | O’Malley DP. Benign extramedullary myeloid proliferations. Mod Pathol. 2007;20:405-415. [PubMed] |
| 15. | Ong K, Tan KB, Putti TC. Myelolipoma within a non-functional adrenal cortical adenoma. Singapore Med J. 2007;48:e200-e202. [PubMed] |
| 16. | Zattoni D, Balzarotti R, Rosso R. The management of bilateral myelolipoma: Case report and review of the literature. Int J Surg Case Rep. 2015;12:31-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Mo XB, Wang XD, Fan SF, Ye J, Wang H. CT imaging diagnosis of adrenal myelolipoma. Chin J Med Imaging Technol. 2004;20:734-736. |
| 18. | Wang ZY, Qu JN, Dong DD. Sonographic analysis of adrenal myelolipoma. J Clin Psychol Med. 2008;10:190-192. |
| 19. | Jung SI, Kim SO, Kang TW, Kwon DD, Park K, Ryu SB. Bilateral adrenal myelolipoma associated with hyperaldosteronism: report of a case and review of the literature. Urology. 2007;70:1223.e11-1223.e13. [PubMed] |
| 20. | Sakaki M, Izaki H, Fukumori T, Taue R, Kishimoto T, Kanayama HO. Bilateral adrenal myelolipoma associated with adrenogenital syndrome. Int J Urol. 2006;13:801-802. [PubMed] |
| 21. | Amendolara M, Barbarino C, Bucca D, Guarnieri F, Novello GB, Romano FM, Stevanato G, Ranzato R. [Giant and bilateral adrenal myelolipoma. Case report]. G Chir. 2008;29:85-88. [PubMed] |
| 22. | Inuzuka M, Tamura N, Sone M, Taura D, Sonoyama T, Honda K, Kojima K, Fukuda Y, Ueda Y, Yamashita Y. A case of myelolipoma with bilateral adrenal hyperaldosteronism cured after unilateral adrenalectomy. Intern Med. 2012;51:479-485. [PubMed] |
P- Reviewer: Gokul S, Neri V S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/