Published online Mar 16, 2015. doi: 10.12998/wjcc.v3.i3.327
Peer-review started: August 21, 2014
First decision: November 18, 2014
Revised: November 29, 2014
Accepted: January 9, 2015
Article in press: January 15, 2015
Published online: March 16, 2015
Processing time: 204 Days and 17.6 Hours
Achalasia is a prototypic esophageal motility disorder with complications including aspiration-pneumonia, esophagitis, esophageal-tracheal fistula, spontaneous rupture of the esophagus, and squamous cell carcinoma. However, achalasia is rarely associated with esophageal stones and ulcer formation that lead to upper gastrointestinal bleeding. Here, we report the case of a 61-year-old woman who was admitted to our department after vomiting blood for six hours. Physical examination revealed that the patient had severe anemia and mild palpitation in the upper abdomen. CT revealed lower esophageal dilatation and esophageal wall thickening, and an emergency upper endoscopy showed that the esophagus was substantially expanded by a dark round stone, with multiple ulcers on the esophageal wall and a slit in the cardiac mucosa with a large clot attached. The patient’s history included ingestion of 1 kg hawthorn three days prior. The acute upper gastrointestinal bleeding was caused by Mallory-Weiss syndrome associated with achalasia and an esophageal stone. For patients with achalasia, preventing excessive ingestion of tannins is crucial to avoid complications such as bleeding and rupture.
Core tip: Achalasia is the prototypic esophageal motility disorder that leaves patients at risk for various complications. This is a rare report of long-term achalasia associated with esophageal stone and ulcer formation leading to upper gastrointestinal bleeding caused by Mallory-Weiss syndrome. This paper highlights the importance of avoiding excess tannin ingestion for patients with achalasia to prevent the development of complications such as bleeding and rupture.
- Citation: Zhang WW, Xie XJ, Geng CX, Zhan SH. Rare case of upper gastrointestinal bleeding in achalasia. World J Clin Cases 2015; 3(3): 327-329
- URL: https://www.wjgnet.com/2307-8960/full/v3/i3/327.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i3.327
Achalasia is the prototypic esophageal motility disorder characterized by a hypertensive lower esophageal sphincter with incomplete relaxation upon swallowing, accompanied by aperistalsis of the esophageal body[1]. Patients with achalasia are at risk for developing complications such as aspiration-pneumonia, esophagitis, esophageal ulcers and bleeding, esophageal-tracheal fistula, spontaneous rupture of the esophagus, and squamous cell carcinoma[2]. The prevalence is 10 per 100000 in the United States, involving an equal distribution of men and women of all ages and from all ethnicities[3]. We report a rare case of upper gastrointestinal bleeding in a patient with achalasia that was associated with an esophageal stone, ulcer formation and Mallory-Weiss syndrome.
A 61-year-old woman who complained of vomiting blood for six hours was admitted to our department. She experienced dizziness, palpitations, sweating, and fatigue, but did not present with fever, rash or jaundice. Her medical history revealed achalasia that had been present for 30 years, for which she had declined any treatment. When questioned, she reported ingesting 1 kg hawthorn within the past 3 d.
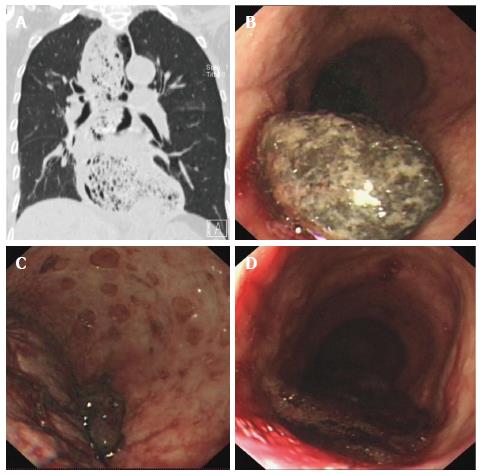
A physical examination indicated that the patient had severe anemia due to pale conjunctiva and nail beds, and mild palpitation in the upper abdomen. Routine blood tests showed: red blood cell count, 1.34 × 1012/L; hemoglobin, 41 g/L; white blood cell count, 11.25 × 109/L; platelet count, 150 × 109/L; blood urea nitrogen, 15.99 mmol/L; and creatinine, 98 μmol/L. Lower esophageal dilatation and esophageal wall thickening were revealed upon CT examination (Figure 1A). An emergency upper endoscopy was performed revealing substantial expansion of the esophagus by a dark round stone (Figure 1B), multiple ulcers on the esophageal wall (Figure 1C), and a slit in the cardiac mucosa with a large clot attached (Figure 1D). Endoscopic sprinkling hemostasis and injection of 2.5% sodium bicarbonate were applied to cease the bleeding and dissolve the stone.
In achalasia, injury to the lower esophageal sphincter neurons and the loss of the main functional inhibitory neurotransmitter result in a hypertensive sphincter that loses its ability to relax, leading to stenosis of cardia and lower esophagus expansion. Occasionally, patients will present with persistent food retention, and esophageal stone formation can occur in those who have ingested foods rich in tannins, such as hawthorn and persimmon. The pressure of stones can cause multiple ulcers and even upper gastrointestinal bleeding. The discomfort when swallowing and frequent nausea and vomiting can then lead to the development of Mallory-Weiss syndrome.
Currently, there are no curative treatments for achalasia cardia, rather palliative measures are provided, such as oral nitrates or calcium channel blockers, endoscopic pneumatic dilation, injection of sclerosant substances, or surgery[4-6]. However, complications such as bleeding and rupture can be prevented by avoiding excessive ingestion of tannins.
A 61-year-old female patient complained of vomiting blood for six hours.
Acute upper gastrointestinal bleeding from Mallory-Weiss syndrome associated with achalasia.
Red blood cell count, 1.34 × 1012/L; hemoglobin, 41 g/L; white blood cell count, 11.25 × 109/L; platelet count, 150 × 109/L; blood urea nitrogen, 15.99 mmol/L; creatinine 98 µmol/L.
CT showed lower esophageal dilatation and esophageal wall thickening. Upper endoscopy revealed a large round stone causing substantial expansion of the esophagus and multiple ulcers on the esophageal wall. A slit in the cardiac mucosa was observed with a large clot attached.
Endoscopic sprinkling hemostasis and injection of 2.5% sodium bicarbonate were applied to cease the bleeding and dissolve the stone.
Although there are some reports of achalasia combined with esophageal intramural hematoma or esophageal varices, reports of achalasia combined with esophageal stones, ulcer formation and Mallory-Weiss syndrome are rare.
Achalasia is characterized by esophageal aperistalsis and impaired relaxation of the lower esophageal sphincter.
This report not only presents a rare case of upper gastrointestinal bleeding associated with achalasia, but also aims to inform patients with achalasia to avoid excessive ingestion of tannin-rich foods to prevent related complications.
This is a very interesting manuscript reporting a rare case of upper gastrointestinal bleeding as a result of long-term achalasia associated with esophageal stones.
| 1. | Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143:328-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 221] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 2. | O’Neill OM, Johnston BT, Coleman HG. Achalasia: a review of clinical diagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2013;19:5806-5812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 159] [Cited by in RCA: 140] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 3. | Fei L, Rossetti G, Moccia F, Cimmino M, Guerriero L, Romano G, Pascotto B, Orlando F. Definition, incidence and etiology: what’s new in the 21st century? Ann Ital Chir. 2013;84:489-494. [PubMed] |
| 4. | Moretó M, Ojembarrena E, Barturen A, Casado I. Treatment of achalasia by injection of sclerosant substances: a long-term report. Dig Dis Sci. 2013;58:788-796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Meireles OR, Horgan S, Jacobsen GR, Katagiri T, Mathew A, Sedrak M, Sandler BJ, Dotai T, Savides TJ, Majid SF. Transesophageal endoscopic myotomy (TEEM) for the treatment of achalasia: the United States human experience. Surg Endosc. 2013;27:1803-1809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2014;259:1098-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 235] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
P- Reviewer: Bax BE, Holtmann GJ, Munoz M S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/