Published online Feb 16, 2015. doi: 10.12998/wjcc.v3.i2.199
Peer-review started: July 29, 2014
First decision: September 16, 2014
Revised: November 4, 2014
Accepted: November 17, 2014
Article in press: November 19, 2014
Published online: February 16, 2015
Processing time: 191 Days and 12.4 Hours
The most significant factor for the success in soft tissue grafts is the synergistic relation between vascular configuration and involved tissues. In the soft tissue graft procedures, site specific donor tissue is assumed to have improved potential for function and aesthetic survive at recipient sites. On a clinical level, using site specific gingival unit graft that placed on traditionally prepared recipient site, results in predictable root coverage. In this case report the clinical effectiveness of gingival unit transfer (GUT) technique performed on Miller III recession was presented and a similar recession case treated with free gingival graft (FGG) technique for comparison. Probing depth, recession depth, keratinized tissue width and clinical attachment level clinical parameters were measured at baseline and postoperative 8 mo. Percentage of defect coverage was evaluated at postoperative 8 mo. Creeping attachment was assessed at postoperative 1, 3, 6 and 8 mo. The GUT revealed better defect coverage and creeping attachment results than the FGG in the treatment of Miller III defects.
Core tip: On a clinical level, using site specific vascular configuration gingival unit graft for donor tissue that placed on traditionally prepared recipient site, results in predictable defect coverage. This report was to evaluate effectiveness of gingival unit transfer technique in comparison with free gingival graft technique on clinical parameters in the Miller III recessions treatment.
- Citation: Yıldırım S, Kuru B. Gingival unit transfer using in the Miller III recession defect treatment. World J Clin Cases 2015; 3(2): 199-203
- URL: https://www.wjgnet.com/2307-8960/full/v3/i2/199.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i2.199
Gingival recession is the denudation of root surfaces as a result of the relocation of the gingival margin apical to the cement-enamel junction (CEJ)[1] that causes root hypersensitivity and aesthetic problems[2].
Recession defects can be treated with numerous surgical procedures such as free gingival grafts[3], connective tissue grafts[4], acellular dermal matrix grafts[5], various pedicle flaps[6,7], combinations of these pedicle flaps and graft techniques[8,9] and guided tissue regeneration[10]. The literature review presents different rates of success and predictability with these surgical procedures[11-13]. Nevertheless, additional clinical studies are needed to define the issues that are in a relation with the predictable and successful results[12].
The synergistic relation between vascular configuration and related tissues is one of the major factors for the success in soft tissue grafts[14,15]. Gingival tissue has complex and unique vascularity[16]. Supracrestal part of gingiva, as well as the donor tissue, is naturally created and specifically designed to function and survive above avascular denude root surfaces[14] in the soft tissue grafts procedures[17]. Gingival unit (GU) graft with site specific vascular supply placed on traditionally prepared recipient area may have capacity for survival on root surfaces and results in predictable root coverage[18].
Most clinical studies about root surface coverage have focalized on Miller I-II recession treatment[19]. Defect coverage by using gingival unit transfer (GUT) on Miller I-II recession defects revealed successful results in a previous clinical study[18]. However, there is a lack of success and ability to provide root coverage in Miller III recession defects, because of interproximal bone and soft tissue loss[20]. There are different anatomical characteristics when compared with Miller I-II recession defects, as if prominent and avascular root surfaces, decreased periosteal bed and occasionally deep periodontal pocket depths[21].
The purpose of this case report is to present the clinical results of two cases of Miller III localized recessions treated by using GUT and free gingival graft (FGG).
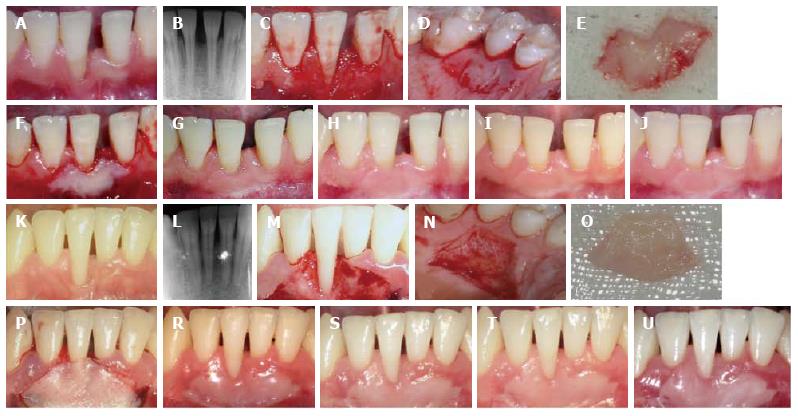
In April 2009, a 25-year-old woman (case I) and 21-year-old man (case II) with single Miller III recession defects on mandibular right central incisor were applied to the Periodontology Department of Marmara University (Figure 1A, B, K and L). Case I had complaints about aesthetics and tooth loss whereas case II about hypersensitivity. Patients were non-smokers, did not have any medical problems and there were no contraindications for periodontal surgery. After clinical examination, oral hygiene motivation and mechanical periodontal treatment were performed.
Recession depth (RD) was recorded from CEJ to margin of the gingiva, probing depth (PD) was recorded from margin of the gingiva to the bottom of the pocket, clinical attachment level (CAL) was recorded from CEJ to bottom of the pocket, keratinized tissue width (KTW) was recorded from the margin of the gingiva to mucogingival junction, at baseline and postoperative 8 mo with a manual probe (PCP UNC-15, Hu-Friedy, Chicago, IL.). Only RD parameter was measured at 1, 3 and 6 mo for the evaluation of soft tissue creeping coronally.
One clinician (BK) performed surgical procedures and another clinician (SY) evaluated clinical measurements. Local anesthesia was made and then in both cases, the recipient site was prepared by two vertical beveled incisions that extending apically to adjacent teeth, 3 to 4 mm across to the mucogingival line, and the surfaces of interdental papillae was removed (Figure 1A, C, K and M)[14]. The incisions were divergent therefore the recipient site was trapezoidal. At the mucogingival line, vertical incisions were connected by a horizontal incision. A partial thickness dissection was made apical to the alveolar mucosa. The epithelial surfaces within these incisions were deepithelized. The base of the recipient site was ≥ 5 mm apical to the apical part of the exposed portion of the root surface. The root planning was made in the exposed portion of the root surface with hand instruments. Then irrigated with saline[18].
In case I, the GU graft was harvested from the palatal part of the premolar area (Figure 1D) including the marginal gingival tissue and the papillae. In case II, the donor FGG was conventionally dissected from the palate aspect of the premolar area, but ≥2 mm apical from the margin of the gingiva (Figure 1N)[18]. In both cases, thickness of grafts were about 1 mm[22]. Then the grafts were sutured at the level to the CEJ (Figure 1E, F, O and P), and compressed for 2 min[18]. The periodontal dressing was applied to the donor sites for closing the wound. After 1 wk, the dressing and sutures were removed.
At the postsurgical care for infection control, the patients were advised rinse twice daily with 0.2% chlorhexidine solution for 3 wk, avoid brushing and hard chewing. After that, a gentle coronally directed brushing in the surgical area was recommended. During the first 2 mo recall appointments were scheduled every second week, and then patients were called once a month for the postoperative following period[18].
At postoperative period in both patients clinical healing in both the recipient and donor sites was complete and no complications were observed. Pre (0 d) and postsurgical (8 mo) clinical parameters are shown in Table 1. At 8 mo, 2.5 mm defect coverage with a PD of 1 mm, CAL gain of 2.5 mm and KTW gain of 5 mm was observed in case I grafted with a GUT. Two millimetre defect coverage with a PD of 1.5 mm, CAL gain of 2.5 mm and KTW gain of 4.5 mm was observed in case II grafted with FGG (Table 1). Percentage of defect closure were 83% and 50% in cases I and II, respectively. The creeping attachment level in case I was 1.5 mm between 1 and 8 mo period (Table 2). The margin of the GU graft was moved coronally, and an acceptable colour and configuration harmony with adjacent gingival tissues was seen (Figure 1G, H, I and J). In case II, there was no color harmony with the adjacent tissue and 1 mm of creeping was detected at the same follow-up period (Figure 1R, S, T and U) (Table 2).
| Parameters | Case I gingival unit graft technique | Case II free gingival graft technique | ||||
| 0 d | 8 mo | Gain | 0 d | 8 mo | Gain | |
| Recession depth (mm) | 3 | 0.5 | 2.5 | 4 | 2 | 2 |
| Probing depth (midbuccal) (mm) | 1 | 1 | 0 | 2 | 1.5 | 0.5 |
| Clinical attachment level (mm) | 4 | 1.5 | 2.5 | 6 | 3.5 | 2.5 |
| Keratinized tissue width (mm) | 2 | 7 | 5 | 1.5 | 6 | 4.5 |
| Defect closure (%) | 83 | 50 | ||||
| Recession reduction (mm) | Case I | Case II |
| 1-3 mo | 0 | 0.5 |
| 3-6 mo | 0.5 | 0 |
| 6-8 mo | 1 | 0.5 |
| 1-8 mo | 1.5 | 1 |
GUT technique, using GU graft as a donor tissue with site specific vascular supply, was evaluated in treatment of a single Miller III gingival recession case. GUT is a modification of FGG with the difference of including marginal gingiva and papillae in the conventional palatal tissue graft that vascular supply matches intimately with the recipient site[14,18]. After 8 mo in this case, RD reduction and defect coverage were found in favor of GU graft compared to FGG.
This is the first case reporting the use of GUT technique in the Miller III localized gingival recession treatment. There are no clinical studies or case reports with which to compare our clinical outcomes. There is one case report in which gingival unit was used as a FGG[14] and a randomized clinical trial evaluating GUT in comparison with FGG in the Miller I-II recession defects treatment[18]. In this case report, the GU graft performed in the Miller III recession defect treatment, 2.5 mm of RD reduction; 83% defect coverage together with gains in CAL and keratinized tissue (KT) were reported. The reduction in recession was in accordance with the attachment gain. The mean defect coverage was 50% in the FGG case, presenting an obvious difference from the GUT case.
According to our clinical outcomes, GUT resulted in almost indistinguishable texture and colour with neighbouring soft tissues. Creeping defines the postoperative movement of marginal gingiva coronally[23]. Allen[14] presented equivalent results in his case report that the marginal position of the GU graft is more coronal than the neighbouring gingival tissue at 3 mo. Creeping has been detected in several clinical studies[24-27]. With an average of 1 mm, creeping can be seen within 1-12 mo after FGG in narrow recessions[25,26]. However, after 8 mo, the coronal ascent of gingival margins in case I, treated with a GUT (1.5 mm) was higher than in case II (1 mm). The unique vascular supply of GU graft is believed to be of importance for this difference[18]. The present outcomes support the usefulness of GUT for suitable root coverage in aesthetic areas. Although FGG has lost its popularity for aesthetic area[28,29], it may be still the gold standard surgical technique to increased KT[30] especially when it is modified with the inclusion of marginal and papillary gingival tissue.
The GU donor site healed uneventfully. No unacceptable attachment loss or recession were detected at the premolar site where the GU graft was harvested from in case I after postoperative 8 mo. Inevitable recession at donor site were reported in laterally positioned flap procedure[6]. This does not possible for GUT procedure. Harvesting donor graft with marginal gingiva is easy, less invasive. Any harmful results can be prevented with cautious manipulation. Before harvesting the GU graft, the depth of gingival sulcus at palatal donor premolar area was measured. Donor tissue was harvested carefully not to cause any attachment loss. If some injury had happened at the attachment, new attachment apparatus would have been developed quickly[31].
In conclusion, the GUT technique performed on case I can be successfully used for the Miller III recession defect treatment.
Twenty-five (female) and 20-year-old (male) patients with Miller Class III localized gingival recession defects on mandibular anterior teeth.
Miller Class III recession defect on mandibular anterior teeth.
One patient was treated with gingival unit transfer whereas the other with free gingival graft technique.
Gingival unit graft is masticatory palatal tissue involving marginal gingival and papillary tissue.
Surgical treatment of Miller III gingival recessions are more challenging, due to loss of interproximal bone and soft tissues. This case report represents the effectiveness of gingival unit transfer technique in comparison with free gingival graft technique on clinical parameters in the treatment of Miller III gingival recession.
This is an interesting case report.
| 1. | American Academy of Periodontology. Glossary of Periodontal Terms, 4th ed. Chicago, IL: American Academy of Periodontology 2001; 44 Available from: http//www.joponline.org/page/glossary. |
| 2. | Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 286] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 3. | Sullivan HC, Atkins JH. Free autogenous gingival grafts. 3. Utilization of grafts in the treatment of gingival recession. Periodontics. 1968;6:152-160. [PubMed] |
| 4. | Langer B, Langer L. Subepithelial connective tissue graft technique for root coverage. J Periodontol. 1985;56:715-720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 502] [Cited by in RCA: 494] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 5. | Mahajan A, Dixit J, Verma UP. A patient-centered clinical evaluation of acellular dermal matrix graft in the treatment of gingival recession defects. J Periodontol. 2007;78:2348-2355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Guinard EA, Caffesse RG. Treatment of localized gingival recessions. Part III. Comparison of results obtained with lateral sliding and coronally repositioned flaps. J Periodontol. 1978;49:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 7. | Bernimoulin JP, Lüscher B, Mühlemann HR. Coronally repositioned periodontal flap. Clinical evaluation after one year. J Clin Periodontol. 1975;2:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 183] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Kuru BE. Treatment of localized gingival recessions using enamel matrix derivative as an adjunct to laterally sliding flap: 2 case reports. Quintessence Int. 2009;40:461-469. [PubMed] |
| 9. | Zucchelli G, Amore C, Sforza NM, Montebugnoli L, De Sanctis M. Bilaminar techniques for the treatment of recession-type defects. A comparative clinical study. J Clin Periodontol. 2003;30:862-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 113] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Pini Prato G, Tinti C, Vincenzi G, Magnani C, Cortellini P, Clauser C. Guided tissue regeneration versus mucogingival surgery in the treatment of human buccal gingival recession. J Periodontol. 1992;63:919-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 179] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 11. | Roccuzzo M, Bunino M, Needleman I, Sanz M. Periodontal plastic surgery for treatment of localized gingival recessions: a systematic review. J Clin Periodontol. 2002;29 Suppl 3:178-194; discussion 195-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 264] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 12. | Cairo F, Pagliaro U, Nieri M. Treatment of gingival recession with coronally advanced flap procedures: a systematic review. J Clin Periodontol. 2008;35:136-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 271] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 13. | Chambrone L, Sukekava F, Araújo MG, Pustiglioni FE, Chambrone LA, Lima LA. Root coverage procedures for the treatment of localised recession-type defects. Cochrane Database Syst Rev. 2009;2:CD007161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Allen AL. Use of the gingival unit transfer in soft tissue grafting: report of three cases. Int J Periodontics Restorative Dent. 2004;24:165-175. [PubMed] |
| 15. | Burkhardt R, Lang NP. Coverage of localized gingival recessions: comparison of micro- and macrosurgical techniques. J Clin Periodontol. 2005;32:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 107] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 16. | Schroeder HE, Listgarten MA. The gingival tissues: the architecture of periodontal protection. Periodontol 2000. 1997;13:91-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 205] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Nobuto T, Imai H, Yamaoka A. Microvascularization of the free gingival autograft. J Periodontol. 1988;59:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Kuru B, Yıldırım S. Treatment of localized gingival recessions using gingival unit grafts: a randomized controlled clinical trial. J Periodontol. 2013;84:41-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Bouchard P, Malet J, Borghetti A. Decision-making in aesthetics: root coverage revisited. Periodontol 2000. 2001;27:97-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 113] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Remya V, Kishore Kumar K, Sudharsan S, Arun KV. Free gingival graft in the treatment of class III gingival recession. Indian J Dent Res. 2008;19:247-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Aroca S, Keglevich T, Nikolidakis D, Gera I, Nagy K, Azzi R, Etienne D. Treatment of class III multiple gingival recessions: a randomized-clinical trial. J Clin Periodontol. 2010;37:88-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 121] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 22. | Côrtes Ade Q, Martins AG, Nociti FH, Sallum AW, Casati MZ, Sallum EA. Coronally positioned flap with or without acellular dermal matrix graft in the treatment of Class I gingival recessions: a randomized controlled clinical study. J Periodontol. 2004;75:1137-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Goldman HM, Cohen DW. Periodontal Therapy. 5th ed. St. Louis: C.V. Mosby 1973; 715-718. |
| 24. | Matter J, Cimasoni G. Creeping attachment after free gingival grafts. J Periodontol. 1976;47:574-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 63] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Bell LA, Valluzzo TA, Garnick JJ, Pennel BM. The presence of “creeping attachment” in human gingiva. J Periodontol. 1978;49:513-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Matter J. Creeping attachment of free gingival grafts. A five-year follow-up study. J Periodontol. 1980;51:681-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 88] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Harris RJ. Creeping attachment associated with the connective tissue with partial-thickness double pedicle graft. J Periodontol. 1997;68:890-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | Agudio G, Nieri M, Rotundo R, Cortellini P, Pini Prato G. Free gingival grafts to increase keratinized tissue: a retrospective long-term evaluation (10 to 25 years) of outcomes. J Periodontol. 2008;79:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | McGuire MK. Coverage of the denuded root surface using the free soft tissue autograft. J Am Dent Assoc. 1990;121:277-279. [PubMed] |
| 30. | Camargo PM, Melnick PR, Kenney EB. The use of free gingival grafts for aesthetic purposes. Periodontol 2000. 2001;27:72-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 88] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 31. | Listgarten M. Ultrastructure of the dento-gingival junction after gingivectomy. J Periodontal Res. 1972;7:151-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
P- Reviewer: Arabaci T, Jeng JH S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/