Published online Feb 16, 2015. doi: 10.12998/wjcc.v3.i2.148
Peer-review started: July 27, 2014
First decision: September 16, 2014
Revised: September 29, 2014
Accepted: October 28, 2014
Article in press: October 29, 2014
Published online: February 16, 2015
Processing time: 193 Days and 18.1 Hours
Coronary artery disease (CAD) remains the leading cause of death worldwide with approximately 1 in 30 patients with stable CAD experiencing death or acute myocardial infarction each year. The presence and extent of resultant myocardial ischaemia has been shown to confer an increased risk of adverse outcomes. Whilst, optimal medical therapy (OMT) forms the cornerstone of the management of patients with stable CAD, a significant number of patients present with ischaemia refractory to OMT. Historically coronary angiography alone has been used to determine coronary lesion severity in both stable and acute settings. It is increasingly clear that this approach fails to accurately identify the haemodynamic significance of lesions; especially those that are visually “intermediate” in severity. Revascularisation based upon angiographic appearances alone may not reduce coronary events above OMT. Technological advances have enabled the measurement of physiological indices including the fractional flow reserve, the index of microcirculatory resistance and the coronary flow reserve. The integration of these parameters into the routine management of patients presenting to the cardiac catheterization laboratory with CAD represents a critical adjunctive tool in the optimal management of these patients by identifying patients that would most benefit from revascularisation and importantly also highlighting patients that would not gain benefit and therefore reducing the likelihood of adverse outcomes associated with coronary revascularisation. Furthermore, these techniques are applicable to a broad range of patients including those with left main stem disease, proximal coronary disease, diabetes mellitus, previous percutaneous coronary intervention and with previous coronary artery bypass grafting. This review will discuss current concepts relevant to coronary physiology assessment, its role in the management of both stable and acute patients and future applications.
Core tip: Coronary artery disease remains the leading cause of death worldwide. There is increasing evidence to suggest that the use of invasive coronary angiography alone may not reliably identify all lesions associated with haemodynamic compromise. Technological advances have enabled the measurement of a number of coronary physiological indices which when incorporated into routine practice are associated with improved outcomes, reduced risks and greater economy. This review will discuss current concepts relevant to coronary physiology assessment, its role in the management of both stable and acute patients and future applications.
- Citation: Ruparelia N, Kharbanda RK. Role of coronary physiology in the contemporary management of coronary artery disease. World J Clin Cases 2015; 3(2): 148-155
- URL: https://www.wjgnet.com/2307-8960/full/v3/i2/148.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i2.148
Coronary artery disease (CAD) is the leading cause of death worldwide[1] with approximately 1 in 30 patients with stable CAD experiencing acute myocardial infarction (AMI) or cardiovascular death each year[2]. The presence of resultant myocardial ischaemia and its extent has been shown to confer increased risk of adverse outcomes[3-6]. With an increasing burden of atherosclerotic coronary disease and the associated high event rate, there is a need to identify both patients at highest risk with most to benefit from revascularisation strategies and also those that would be best managed by a conservative approach to improve clinical outcomes and minimise exposure to procedural risks.
Prevention by risk factor control and optimal medical therapy (OMT) including aspirin[7], beta-blockers[8], statins[9] and angiotensin converting enzyme inhibitors forms the cornerstone of the management of patients with stable CAD[10,11]. However, a significant number of patients present with myocardial ischaemia refractory to OMT and subsequently undergo coronary revascularisation by percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) with the aim of reducing ischaemic burden and therefore risk[12].
Historically, visual assessment of coronary lesions by invasive coronary angiography in isolation has been used to determine the severity of coronary lesions in both stable and acute settings. It is increasingly clear that this approach fails to accurately and consistently identify the haemodynamic significance of lesions, especially those that are “intermediate” in severity[13] and that revascularisation based upon angiographic appearances may not reduce coronary events above OMT alone[14]. Recent advances in technology and understanding of coronary physiology have resulted in its central role in the assessment of patients in the catheterization laboratory and their optimal management[15,16]. This review will discuss current concepts relevant to coronary physiology assessment, its role in the management of patients and possible future applications.
Technological advances have enabled the measure-ment of a number of physiological indices including the fractional flow reserve (FFR), the index of microcirculatory resistance (IMR) and the coronary flow reserve (CFR). The advantages and disadvantages of each of the coronary physiology indices are summarised in Table 1.
| Advantages | Disadvantages | |
| FFR | Clear "cut-off" value Clinically validated Can be used in a wide range of patients Accounts for collateral circulation | Requires administration of vasodilator Risk of coronary artery injury Relatively expensive |
| IMR | True measure of microcirculatory resistance independent of epicardial coronary disease A tool to potentially predict prognosis in acute patients | Requires administration of vasodilator The full extent of clinical utility is currently unknown |
| CFR | A tool to potentially predict prognosis in acute patients | Value is affected by both epicardial disease and microvasculature The full extent of clinical utility is currently unknown Influenced by hemodynamics |
FFR is the ratio of myocardial blood flow in a stenosed coronary artery at maximal hyperaemia in comparison to normal (proximal) myocardial flow. It quantifies the pressure drop measured across a coronary artery stenosis[17] and therefore the physiological significance of the lesion. The pressure drop is directly proportional to stenosis length, inversely proportional to lumen cross-sectional area and related to the square of the blood velocity. FFR is thus related to both lesion morphology and the volume of viable subtended myocardium and is independent of changes in haemodynamic conditions[18].
CFR is the ratio of hyperaemic to resting coronary flow and incorporates both the epicardial and microvascular circulations[19]. A value of < 2.0 is correlated with stenosis severity[20].
IMR is a measure of true microcirculatory resistance and is calculated by measuring the distal arterial pressure at hyperaemia divided by the inverse of the transit time. The IMR is not influenced by the presence or absence of epicardial artery stenosis[21]. There is no absolute validated “normal” value but a cut-off value of 32 units has been shown to be predictive of myocardial recovery following AMI[22].
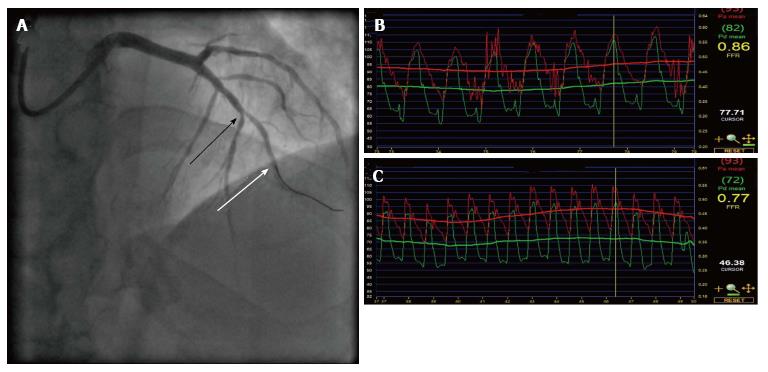
To measure the FFR, a wire with a distal pressure sensor is advanced into a guiding coronary artery catheter, the pressure is equalised, and then passed distal to the coronary stenosis of interest (Figure 1A). The aortic pressure (Pa) is measured from the guide catheter and the distal pressure (Pd) from the pressure sensor distal to the stenosis (Figure 1B). To calculate the FFR, hyperaemia is achieved by the administration of intravenous (140 mcg/kg per minute) or intracoronary (20-50 mcg) adenosine and is the ratio of hyperaemia Pd/Pa (Figure 1C). Other hyperaemic stimuli can be used but adenosine is the most widely validated.
In the measurement of IMR and CFR, the shaft of the pressure wire is used to detect changes in the temperature-dependent electrical resistance and thus acts as a proximal thermistor. The sensor at the end of the wire is used to simultaneously measure pressure and temperature at the distal end of the artery. Therefore, the transit time of room-temperature saline injected through the guiding coronary artery catheter can be calculated using a thermodilution technique[23]. The initial transit time is recorded (Tmn) following three injections of room-temperature saline. Following hyperaemia, three further injections of room-temperature saline are administered and hyperaemia Tmn is measured. The thermodilution CFR is calculated by dividing the resting Tmn by the hyperaemic Tmn. The IMR is calculated as the distal coronary pressure (Pd) at maximal hyperaemia divided by the inverse of the hyperaemic Tmn.
Many studies have demonstrated that the presence and extent of myocardial ischaemia is closely related to adverse clinical events[5,6,24] with the annual rate of cardiac death and AMI positively correlated with the extent of myocardial ischaemia[24]. Coronary revascularisation has been demonstrated to be beneficial in individuals with moderate and severe ischaemia, with OMT being optimal in patients with mild or no ischaemia[25,26]. In patients with demonstrated extensive ischaemia (> 20% myocardium), an early revascularisation strategy (as opposed to OMT alone) is associated with a 30% reduction in risk of all-cause death[25].
The identification of the presence and extent of myocardial ischaemia in patients presenting with stable CAD is critical to their optimal management. Myocardial perfusion imaging is the most commonly used modality however stress echocardiography and magnetic resonance imaging are increasingly being employed.
There is some evidence that an ischaemia-guided revascularisation strategy is associated with improved prognosis and outcome[27,28]. In patients that underwent myocardial perfusion imaging prior to revascularisation (PCI or CABG) and then in the follow up period, the incidence of patients with worsening ischaemia (> 5% of total myocardium) was more common in patients treated medically in comparison to patients who underwent revascularisation (PCI or CABG) and was an independent predictor of adverse outcomes[29].
PCI reduces mortality in patients with acute coronary syndromes[30], however, in patients presenting with stable CAD, PCI results in an improvement of angina symptoms alone without a mortality advantage in comparison to OMT alone[14]. These results may be a consequence of sub-optimal patient selection due to the sole reliance of visual assessment of coronary lesion by invasive coronary angiography to determine the severity of disease with no information as to the haemodynamic significance of these lesions[31,32]. This can result in inappropriate coronary revascularisation with little benefit and potential procedural risk.
The severity of a lesion (and resultant extent of myocardial ischaemia) is dependant on a number of factors including the severity of luminal narrowing, lesion length and extent of subtended myocardium. As discussed in the previous section, whilst non-invasive techniques can be employed to ascertain the extent of myocardial ischaemia, many patients present to the cardiac catheterization laboratory without having undergone such assessment and indeed, in the setting of multi-vessel disease, non-invasive stress tests are often not able to definitively detect and localise ischaemia[33]. Furthermore, if a non-invasive image approach is taken, a positive test will result in repeat catheterization for PCI - thus further subjecting a patient to procedural complications, delaying revascularisation and being less economical. The use of coronary physiology provides the unique ability to gain immediate information with regards to the haemodynamic significance of specific coronary lesions in patients already in the cardiac catheterization laboratory attending for coronary angiography and identify those at highest risk who are most likely to benefit from PCI.
In stable CAD, CFR decreases as stenosis severity increases. When compared to non-invasive parameters a value of < 2.0 has been shown to correlate with significant ischaemia[20]. However, because CFR takes account of both epicardial and microvascular circulations, this measure can be influenced by exogenous factors[19] and therefore due to confounding factors is no longer used for stenosis assessment[34].
In the setting of stable CAD, the IMR has recently been shown to be independent of the severity of epicardial stenosis when collateral coronary flow is accounted for[35]. IMR may however, play a role in predicting outcome following elective PCI, with a high IMR pre-PCI predicting peri-procedural myocardial infarction following PCI[36].
FFR is a highly reproducible technique and is insensitive to external factors such as changes in haemodynamics[18]. The normal FFR is 1 with a value of ≤ 0.75 associated with ischaemia[37] and ≥ 0.8 not associated with significant ischaemia[38]. There is therefore a “grey zone” of between 0.75-0.8, however the majority of clinical studies to date have adopted a lower normal value of 0.8[12] to define significant ischaemia.
As opposed to relying solely on angiographic appearances, a FFR guided strategy has been shown to identify patients who would most benefit from coronary revascularisation. In the DEFER (deferral versus performance of PCI of non-ischaemia-producing stenoses) study[39], in patients with single-vessel coronary disease and a measured FFR ≥ 0.75, deferral of PCI was associated with similar event free survival in both OMT and PCI groups at five years[40].
In patients presenting with multi-vessel coronary disease, the clinical utility of myocardial perfusion imaging has been doubted. The technique measures relative differences (normal vs abnormal) in myocardial perfusion between coronary artery territories. Thus, in multi-territory ischaemia, the relative differences may be less pronounced resulting in “balanced ischaemia” even in the presence of significant ischaemia as determined by FFR. The FAME study[12] (FFR vs angiography for multi-vessel evaluation trial) which investigated patients with multi-vessel coronary disease, supported an FFR-guided strategy in comparison to angiography alone with an associated reduction in mortality or MI at 2 years[15]. This benefit was also found to be true when compared to contemporary OMT in the more recent FAME II study[16] that indicated that an FFR-guided strategy resulted in a lower rate of urgent revascularisation.
FFR has been shown to be reproducible both in singe and multi-vessel coronary disease. However in certain instances, caution should be taken in interpreting coronary physiology parameters.
In patients presenting with left main stem disease, FFR has been shown to be useful in managing revascularisation strategies[41]. This is also true of left main stem disease and concomitant downstream stenosis if the pressure wire is placed in a non-stenosed downstream vessel and the other vessel does not have a critical proximal stenosis[42].
FFR following PCI has been shown to predict outcome. Post PCI FFR was found to be the strongest predictor of major adverse cardiovascular events at 6 mo[43]. FFR has also been utilised following bifurcation stenting, illustrating that even in the presence of appearances in keeping with severe pinching of side branches, FFR was rarely ≤ 0.75 and therefore of no haemodynamic significance[44].
Following AMI, irreversibly injured myocardium is replaced by scar tissue that results in a reduction in the microcirculation to this territory. FFR in this context can therefore still be used to guide future management strategies, with the value representing viability of the subtended myocardium, but after an appropriate interval to allow for myocardial healing following AMI to ensure adequate hyperaemia[45].
FFR can also safely be used in patients with previous CABG. In an observational study, patients with intermediate stenoses in both arterial and vein graft conduits that were managed by adopting a FFR-guided PCI strategy suffered significantly lower major adverse clinical endpoints as compared to an angiography guided group[46].
FFR depends upon the vasodilatative capacity of the coronary system and therefore achieving maximal hyperaemia. Patients with diabetes mellitus, suffer abnormalities in microvascular function with altered vasodilatative capacity and increased vascular resistance. Whilst caution should be taken in when using FFR in this patient group[47], a recent study comparing FFR in diabetic and non-diabetic patients has shown that FFR appears to be accurate and applicable in this patient group[48].
These studies highlight the critical role played by coronary physiology in identifying haemodynamically significant coronary stenoses that may benefit from revascularisation, and allow targeted vessel specific treatment beyond the angiographic appearances. The concept of the functional as opposed to the anatomical SYNTAX score appears to stratify patients appropriately to CABG or PCI or patients that would be best managed by OMT. FFR is broadly applicable to all patient groups and is associated with improved outcomes.
In the setting of AMI, myocardial inflammation resulting in oedema can result in blunting of the hyperaemic response in the microcirculation resulting in falsely high FFR values, however coronary physiology parameters can potentially still be useful in guiding the management of this patient group.
The IMR when measured in the setting of primary PCI has been shown to correlate with the extent of microvascular obstruction and independently predicted left ventricular systolic function and infarct volume[22,49] and thus provides important prognostic information in this patient group. The clinical utility of this approach, however, is presently unknown.
The thermodilution CFR when measured in the first day after primary PCI also offers important prognostic information with a significant decrease in CFR in patients with impaired left ventricular systolic function. Conversely a greater increase in CFR by day 1 was associated with a higher salvage index[50].
A significant number of patients presenting with acute coronary syndromes also have visually severe “non-culprit” epicardial artery lesions. FFR of “non-culprit” lesions has been shown to be reliable[51] and has been used to guide revascularisation of these lesions. A large prospective multicentre randomised trial is currently underway to investigate the utility of this approach further[52].
The adjunctive beneficial role that coronary physiology plays in the management of CAD has been discussed thus far. There are however, some limitations. The possibility of false negative or false positive results does exist, for example if maximal hyperaemia is not achieved or if instrumentation of the coronary artery induces coronary artery spasm. There is a risk of coronary artery injury (perforation or dissection) with instrumention of the artery to obtain measurements. Finally, there is an additional economic cost when adopting coronary physiology into routine clinical practice with the cost of pressure wires, cost of adenosine, and extra cardiac catheterization laboratory time required. These have all currently limited widespread uptake of these techniques.
A current limitation to invasive coronary physiology techniques is the need to induce maximal hyperaemia with agents such as adenosine. Patients may have contraindications to this agent, and additionally there is a time and cost implication. More recently an adenosine independent index of stenosis severity - the instantaneous wave-free ratio (iFR) has been developed[53]. The accuracy of this ratio in comparison to FFR has been shown to be approximately 80%[54] and outcome data from the on-going DEFINE-FLAIR (functional lesion assessment of intermediate stenosis to guide revascularisation) study[55] are awaited to ascertain if this index can be used routinely in clinical practice.
In the future, there may be non-invasive anatomical and functional imaging surrogates for FFR. Current anatomical imaging modalities [e.g., computed tomography (CT)] correlate poorly with lesion haemodynamic significance and do not capture information related to translesional energy/pressure losses[56]. Newer techniques including CT myocardial perfusion[57], the measurement of contrast gradients in conventional CT angiography[58] and the use of three-dimensional luminal anatomy are currently being evaluated to investigate if they correlate with FFR values for the evaluation of coronary stenoses[59]. Current technologies however have not been shown to equal the sensitivity and specificity of FFR[60].
The integration of invasive coronary physiology measurements into the routine management of patients presenting to the cardiac catheterization laboratory with CAD represents a critical adjunctive tool in the optimal management of these patients. The use of FFR can identify patients that would most benefit from revascularisation either by PCI or CABG and importantly also highlights patients that would not gain benefit and therefore reducing the likelihood of adverse outcomes associated with coronary revascularisation. In the setting of acute coronary syndromes, the use of IMR and CFR provides important information with regard to outcome and myocardial salvage, although the clinical value of these measures remains uncertain. The interpretation of the described coronary physiology indices is now essential in current interventional cardiology practice and is represented by current training medical curricula in this sub-specialty field.
The use of newer techniques to derive FFR– both invasively that do not depend on the administration of agents to induce hyperaemia and non-invasive functional imaging may result in coronary physiology parameters playing an even more central role in the future.
P- Reviewer: Pani SP, Teragawa H S- Editor: Tian YL L- Editor: A E- Editor: Lu YJ
| 1. | Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6517] [Cited by in RCA: 7008] [Article Influence: 350.4] [Reference Citation Analysis (4)] |
| 2. | Steg PG, Bhatt DL, Wilson PW, D’Agostino R, Ohman EM, Röther J, Liau CS, Hirsch AT, Mas JL, Ikeda Y. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA. 2007;297:1197-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1005] [Cited by in RCA: 990] [Article Influence: 52.1] [Reference Citation Analysis (0)] |
| 3. | Marwick TH, Case C, Vasey C, Allen S, Short L, Thomas JD. Prediction of mortality by exercise echocardiography: A strategy for combination with the duke treadmill score. Circulation. 2001;103:2566-2571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 124] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Marwick TH, Case C, Sawada S, Rimmerman C, Brenneman P, Kovacs R, Short L, Lauer M. Prediction of mortality using dobutamine echocardiography. J Am Coll Cardiol. 2001;37:754-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 133] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Brown KA, Boucher CA, Okada RD, Guiney TE, Newell JB, Strauss HW, Pohost GM. Prognostic value of exercise thallium-201 imaging in patients presenting for evaluation of chest pain. J Am Coll Cardiol. 1983;1:994-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 248] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 6. | Ladenheim ML, Pollock BH, Rozanski A, Berman DS, Staniloff HM, Forrester JS, Diamond GA. Extent and severity of myocardial hypoperfusion as predictors of prognosis in patients with suspected coronary artery disease. J Am Coll Cardiol. 1986;7:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 314] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Hennekens CH, Buring JE, Sandercock P, Collins R, Peto R. Aspirin and other antiplatelet agents in the secondary and primary prevention of cardiovascular disease. Circulation. 1989;80:749-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 150] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Cruickshank JM. Beta-blockers: primary and secondary prevention. J Cardiovasc Pharmacol. 1992;20 Suppl 11:S55-S69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Bulbulia R, Bowman L, Wallendszus K, Parish S, Armitage J, Peto R, Collins R. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20,536 high-risk individuals: a randomised controlled trial. Lancet. 2011;378:2013-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 217] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 10. | Pfisterer ME, Zellweger MJ, Gersh BJ. Management of stable coronary artery disease. Lancet. 2010;375:763-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58:2432-2446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 564] [Cited by in RCA: 673] [Article Influence: 44.9] [Reference Citation Analysis (0)] |
| 12. | Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’ t Veer M, Klauss V, Manoharan G, Engstrøm T, Oldroyd KG. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360:213-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2974] [Cited by in RCA: 3145] [Article Influence: 185.0] [Reference Citation Analysis (0)] |
| 13. | Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333-2342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 767] [Cited by in RCA: 692] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 14. | Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, Knudtson M, Dada M, Casperson P, Harris CL. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356:1503-1516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3259] [Cited by in RCA: 3260] [Article Influence: 171.6] [Reference Citation Analysis (0)] |
| 15. | Pijls NH, Fearon WF, Tonino PA, Siebert U, Ikeno F, Bornschein B, van’t Veer M, Klauss V, Manoharan G, Engstrøm T. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation) study. J Am Coll Cardiol. 2010;56:177-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 807] [Cited by in RCA: 852] [Article Influence: 53.3] [Reference Citation Analysis (0)] |
| 16. | De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, Jagic N, Möbius-Winkler S, Rioufol G, Witt N. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367:991-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1837] [Cited by in RCA: 2055] [Article Influence: 146.8] [Reference Citation Analysis (0)] |
| 17. | Pijls NH, Bech GJ, el Gamal MI, Bonnier HJ, De Bruyne B, Van Gelder B, Michels HR, Koolen JJ. Quantification of recruitable coronary collateral blood flow in conscious humans and its potential to predict future ischemic events. J Am Coll Cardiol. 1995;25:1522-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 171] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | de Bruyne B, Bartunek J, Sys SU, Pijls NH, Heyndrickx GR, Wijns W. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996;94:1842-1849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 284] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 19. | McGinn AL, White CW, Wilson RF. Interstudy variability of coronary flow reserve. Influence of heart rate, arterial pressure, and ventricular preload. Circulation. 1990;81:1319-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 216] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Miller DD, Donohue TJ, Younis LT, Bach RG, Aguirre FV, Wittry MD, Goodgold HM, Chaitman BR, Kern MJ. Correlation of pharmacological 99mTc-sestamibi myocardial perfusion imaging with poststenotic coronary flow reserve in patients with angiographically intermediate coronary artery stenoses. Circulation. 1994;89:2150-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 175] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Fearon WF, Balsam LB, Farouque HM, Caffarelli AD, Robbins RC, Fitzgerald PJ, Yock PG, Yeung AC. Novel index for invasively assessing the coronary microcirculation. Circulation. 2003;107:3129-3132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 535] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 22. | Fearon WF, Shah M, Ng M, Brinton T, Wilson A, Tremmel JA, Schnittger I, Lee DP, Vagelos RH, Fitzgerald PJ. Predictive value of the index of microcirculatory resistance in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2008;51:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 234] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 23. | De Bruyne B, Pijls NH, Smith L, Wievegg M, Heyndrickx GR. Coronary thermodilution to assess flow reserve: experimental validation. Circulation. 2001;104:2003-2006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 217] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 24. | Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, Friedman J, Diamond GA. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 848] [Cited by in RCA: 818] [Article Influence: 29.2] [Reference Citation Analysis (1)] |
| 25. | Hachamovitch R, Rozanski A, Shaw LJ, Stone GW, Thomson LE, Friedman JD, Hayes SW, Cohen I, Germano G, Berman DS. Impact of ischaemia and scar on the therapeutic benefit derived from myocardial revascularization vs. medical therapy among patients undergoing stress-rest myocardial perfusion scintigraphy. Eur Heart J. 2011;32:1012-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 362] [Cited by in RCA: 372] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 26. | Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900-2907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1163] [Cited by in RCA: 1123] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 27. | Kim YH, Ahn JM, Park DW, Song HG, Lee JY, Kim WJ, Yun SC, Kang SJ, Lee SW, Lee CW. Impact of ischemia-guided revascularization with myocardial perfusion imaging for patients with multivessel coronary disease. J Am Coll Cardiol. 2012;60:181-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Hachamovitch R, Rozanski A, Hayes SW, Thomson LE, Germano G, Friedman JD, Cohen I, Berman DS. Predicting therapeutic benefit from myocardial revascularization procedures: are measurements of both resting left ventricular ejection fraction and stress-induced myocardial ischemia necessary? J Nucl Cardiol. 2006;13:768-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 124] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 29. | Farzaneh-Far A, Phillips HR, Shaw LK, Starr AZ, Fiuzat M, O’Connor CM, Sastry A, Shaw LJ, Borges-Neto S. Ischemia change in stable coronary artery disease is an independent predictor of death and myocardial infarction. JACC Cardiovasc Imaging. 2012;5:715-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Armstrong PW. A comparison of pharmacologic therapy with/without timely coronary intervention vs. primary percutaneous intervention early after ST-elevation myocardial infarction: the WEST (Which Early ST-elevation myocardial infarction Therapy) study. Eur Heart J. 2006;27:1530-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 187] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 31. | DeRouen TA, Murray JA, Owen W. Variability in the analysis of coronary arteriograms. Circulation. 1977;55:324-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 354] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 32. | Goldberg RK, Kleiman NS, Minor ST, Abukhalil J, Raizner AE. Comparison of quantitative coronary angiography to visual estimates of lesion severity pre and post PTCA. Am Heart J. 1990;119:178-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 75] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 33. | Lima RS, Watson DD, Goode AR, Siadaty MS, Ragosta M, Beller GA, Samady H. Incremental value of combined perfusion and function over perfusion alone by gated SPECT myocardial perfusion imaging for detection of severe three-vessel coronary artery disease. J Am Coll Cardiol. 2003;42:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 284] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 34. | Kern MJ, Lerman A, Bech JW, De Bruyne B, Eeckhout E, Fearon WF, Higano ST, Lim MJ, Meuwissen M, Piek JJ. Physiological assessment of coronary artery disease in the cardiac catheterization laboratory: a scientific statement from the American Heart Association Committee on Diagnostic and Interventional Cardiac Catheterization, Council on Clinical Cardiology. Circulation. 2006;114:1321-1341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 381] [Cited by in RCA: 363] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 35. | Yong AS, Ho M, Shah MG, Ng MK, Fearon WF. Coronary microcirculatory resistance is independent of epicardial stenosis. Circ Cardiovasc Interv. 2012;5:103-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 36. | Ng MK, Yong AS, Ho M, Shah MG, Chawantanpipat C, O’Connell R, Keech A, Kritharides L, Fearon WF. The index of microcirculatory resistance predicts myocardial infarction related to percutaneous coronary intervention. Circ Cardiovasc Interv. 2012;5:515-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 37. | Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek J Koolen JJ, Koolen JJ. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1629] [Cited by in RCA: 1647] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 38. | Kern MJ, Samady H. Current concepts of integrated coronary physiology in the catheterization laboratory. J Am Coll Cardiol. 2010;55:173-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 208] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 39. | Bech GJ, De Bruyne B, Pijls NH, de Muinck ED, Hoorntje JC, Escaned J, Stella PR, Boersma E, Bartunek J, Koolen JJ. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation. 2001;103:2928-2934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 573] [Cited by in RCA: 629] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 40. | Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van’t Veer M, Bär F, Hoorntje J, Koolen J, Wijns W. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105-2111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1099] [Cited by in RCA: 1188] [Article Influence: 62.5] [Reference Citation Analysis (12)] |
| 41. | Hamilos M, Muller O, Cuisset T, Ntalianis A, Chlouverakis G, Sarno G, Nelis O, Bartunek J, Vanderheyden M, Wyffels E. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120:1505-1512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 288] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 42. | Yong AS, Daniels D, De Bruyne B, Kim HS, Ikeno F, Lyons J, Pijls NH, Fearon WF. Fractional flow reserve assessment of left main stenosis in the presence of downstream coronary stenoses. Circ Cardiovasc Interv. 2013;6:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 43. | Pijls NH, Klauss V, Siebert U, Powers E, Takazawa K, Fearon WF, Escaned J, Tsurumi Y, Akasaka T, Samady H. Coronary pressure measurement after stenting predicts adverse events at follow-up: a multicenter registry. Circulation. 2002;105:2950-2954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 241] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 44. | Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, Sohn DW, Oh BH, Lee MM, Park YB. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46:633-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 229] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 45. | De Bruyne B, Pijls NH, Bartunek J, Kulecki K, Bech JW, De Winter H, Van Crombrugge P, Heyndrickx GR, Wijns W. Fractional flow reserve in patients with prior myocardial infarction. Circulation. 2001;104:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 276] [Cited by in RCA: 268] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 46. | Di Serafino L, De Bruyne B, Mangiacapra F, Bartunek J, Agostoni P, Vanderheyden M, Scognamiglio G, Heyndrickx GR, Wijns W, Barbato E. Long-term clinical outcome after fractional flow reserve- versus angio-guided percutaneous coronary intervention in patients with intermediate stenosis of coronary artery bypass grafts. Am Heart J. 2013;166:110-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 47. | Sahinarslan A, Kocaman SA, Olgun H, Kunak T, Kiziltunç E, Ozdemir M, Timurkaynak T. The reliability of fractional flow reserve measurement in patients with diabetes mellitus. Coron Artery Dis. 2009;20:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Reith S, Battermann S, Hellmich M, Marx N, Burgmaier M. Impact of type 2 diabetes mellitus and glucose control on fractional flow reserve measurements in intermediate grade coronary lesions. Clin Res Cardiol. 2014;103:191-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | McGeoch R, Watkins S, Berry C, Steedman T, Davie A, Byrne J, Hillis S, Lindsay M, Robb S, Dargie H. The index of microcirculatory resistance measured acutely predicts the extent and severity of myocardial infarction in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2010;3:715-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 162] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 50. | Cuculi F, Dall’armellina E, Manlhiot C, De Caterina AR, Colyer S, Ferreira V, Morovat A, Prendergast BD, Forfar JC, Alp NJ. Early change in invasive measures of microvascular function can predict myocardial recovery following pci for st-elevation myocardial infarction. Eur Heart J. 2014;35:1971-1980. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 61] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Ntalianis A, Sels JW, Davidavicius G, Tanaka N, Muller O, Trana C, Barbato E, Hamilos M, Mangiacapra F, Heyndrickx GR. Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2010;3:1274-1281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 257] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 52. | Berry C, Layland J, Sood A, Curzen NP, Balachandran KP, Das R, Junejo S, Henderson RA, Briggs AH, Ford I. Fractional flow reserve versus angiography in guiding management to optimize outcomes in non-ST-elevation myocardial infarction (FAMOUS-NSTEMI): rationale and design of a randomized controlled clinical trial. Am Heart J. 2013;166:662-668.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 53. | Sen S, Escaned J, Malik IS, Mikhail GW, Foale RA, Mila R, Tarkin J, Petraco R, Broyd C, Jabbour R. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012;59:1392-1402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 485] [Cited by in RCA: 544] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 54. | Jeremias A, Maehara A, Généreux P, Asrress KN, Berry C, De Bruyne B, Davies JE, Escaned J, Fearon WF, Gould KL. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. J Am Coll Cardiol. 2014;63:1253-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 288] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 55. | Jeremias A; Clinicaltrials. Functional lesion assessment of intermediate stenosis to guide revascularization (DEFINE-FLAIR); NCT02053038. Available from: http://clinicaltrials.gov/show/NCT02053038. |
| 56. | Meijboom WB, Van Mieghem CA, van Pelt N, Weustink A, Pugliese F, Mollet NR, Boersma E, Regar E, van Geuns RJ, de Jaegere PJ. Comprehensive assessment of coronary artery stenoses: computed tomography coronary angiography versus conventional coronary angiography and correlation with fractional flow reserve in patients with stable angina. J Am Coll Cardiol. 2008;52:636-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 495] [Cited by in RCA: 498] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 57. | Blankstein R, Shturman LD, Rogers IS, Rocha-Filho JA, Okada DR, Sarwar A, Soni AV, Bezerra H, Ghoshhajra BB, Petranovic M. Adenosine-induced stress myocardial perfusion imaging using dual-source cardiac computed tomography. J Am Coll Cardiol. 2009;54:1072-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 301] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 58. | Chow BJ, Kass M, Gagné O, Chen L, Yam Y, Dick A, Wells GA. Can differences in corrected coronary opacification measured with computed tomography predict resting coronary artery flow? J Am Coll Cardiol. 2011;57:1280-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 59. | Koo BK, Erglis A, Doh JH, Daniels DV, Jegere S, Kim HS, Dunning A, DeFrance T, Lansky A, Leipsic J. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol. 2011;58:1989-1997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 825] [Cited by in RCA: 983] [Article Influence: 65.5] [Reference Citation Analysis (0)] |
| 60. | Min JK, Leipsic J, Pencina MJ, Berman DS, Koo BK, van Mieghem C, Erglis A, Lin FY, Dunning AM, Apruzzese P. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA. 2012;308:1237-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 819] [Cited by in RCA: 913] [Article Influence: 65.2] [Reference Citation Analysis (0)] |