Published online Sep 16, 2014. doi: 10.12998/wjcc.v2.i9.455
Revised: May 22, 2014
Accepted: June 27, 2014
Published online: September 16, 2014
Processing time: 145 Days and 14.7 Hours
Calcification of the pericardium is a relatively rare finding and often has an uncertain etiology. Incidental findings of pericardial calcification may increase due to widespread application of cardiac computed tomography for the assessment of coronary atherosclerosis in the appropriate clinical setting using coronary artery calcium scoring and/or coronary angiography. Pericardial calcification alone is asymptomatic and is neither necessary nor sufficient for the diagnosis of pericardial constriction. Its presence may suggest of diffused pericardial scarring and consequently, its pathological involvement with pericardial constriction. Calcification of the pericardium must be evaluated with full clinical knowledge to facilitate an accurate diagnosis and an appropriate therapy when required. Our objective is to present a case of asymptomatic pericardial calcification and to discuss the importance of its clinical implications.
Core tip: Pericardial calcification is rare but may be found more often due to the widespread use of cardiac computed tomography for the assessment of coronary atherosclerosis. Pericardial calcification can be seen in the absence of constrictive physiology and therefore, it should be evaluated with full clinical knowledge.
- Citation: Nguyen T, Phillips C, Movahed A. Incidental findings of pericardial calcification. World J Clin Cases 2014; 2(9): 455-458
- URL: https://www.wjgnet.com/2307-8960/full/v2/i9/455.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i9.455
Calcification of the pericardium is relatively rare and often has an uncertain etiology[1]. Incidental findings of pericardial calcification may increase in the asymptomatic subjects due to the widespread use of cardiac computed tomography for coronary artery calcium scoring (CACS) with and without contrast cardiac computed tomography angiography (CCTA) for the assessment of coronary atherosclerosis. Although detecting pericardial calcification may have important clinical implication for confirming the diagnosis of constrictive pericarditis, its presence should be evaluated with full clinical knowledge to facilitate an accurate diagnosis and an appropriate medical management when it is required. Avoiding inaccurate diagnosis of constrictive pericarditis based only on the presence of calcium in an asymptomatic subject relieves patient’s concern and prevents unnecessary, expensive diagnostic testing.
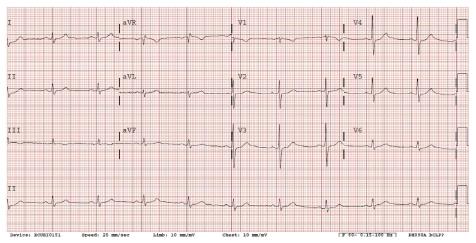
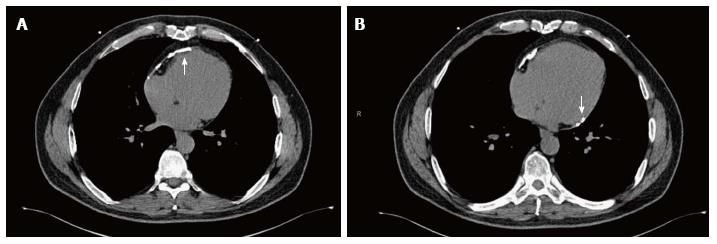
A 58-year-old Caucasian man with hypertension, hyperlipidemia but nonsmoker, and no remarkable history of heart disease, presented to cardiology clinic for cardiovascular risk assessment. He denied chest pain, shortness of breath, palpitation, or dyspnea on exertion. He weighed 97 kg with a body mass index (BMI) of 29 kg/m2. Physical examination revealed a blood pressure of 138/85 mmHg, pulse of 59 bpm, and respiration rate of 16 breaths per minute. Lungs were clear to auscultation. There was no jugular venous distention. Normal heart sounds, no S3 or S4, no murmurs, and no rubs. No hepatomegaly or extremity edema. Electrocardiography (ECG) showed sinus bradycardia with a heart rate of 59 bpm and RSR’ in V1 (Figure 1). Due to his intermediate cardiovascular risk, he underwent non-contrast cardiac computed tomography for CACS for further risk stratification, which showed a low Agatston score of 25.5. This study also revealed an incidental finding of moderate pericardial calcification, mostly involving the anterior and inferobasal portion of the pericardium with no pericardial effusion (Figure 2). Transthoracic echocardiogram showed grade II left ventricular diastolic dysfunction with pseudonormalization pattern, normal valves and normal biventricular size and systolic function. Exercise ECG stress testing demonstrated no evidence of exercise-induced myocardial ischemia at adequate heart rate, achieving 13 metabolic equivalents.
Calcium deposit does not form in a healthy pericardium, but tends to be prominent in the fibrous and scarring pericardium in response to inflammation[1]. Historically, tuberculosis pericarditis is frequently reported as the primary cause of pericardial calcification. More recent cases of pericardial calcifications have been thought to be “idiopathic” and are likely to represent a sequelae of viral pericarditis. Other major known causes include trauma, cardiac surgery, radiation, connective tissue diseases and malignancy[2].
Pericardial calcification alone is asymptomatic. Signs and symptoms are secondary to associate processes such as constrictive pericarditis, which is typically insidious in onset and develops weeks to decades after an episode of pericarditis or chest trauma[3]. Patient usually present with signs and symptoms of right heart failure or low cardiac output including hepatomegaly, ascites, bilateral leg edema, exertion dyspnea, orthopnea, fatigue, elevated JVP, hepatojugular reflux, Kussmaul’s sign, and pulsus paradoxus[2,3].
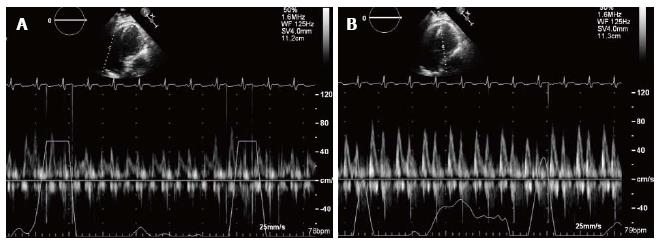
Evaluating patients with symptomatic pericardial calcification or a high suspicion of constrictive pericarditis may involve multiple imaging modalities. Electrocardiogram may show decreased QRS voltage and flattened T waves[2]. On chest radiographs, calcification may be seen as curvilinear opacities follow expected pericardial contour located predominantly over right atrium and ventricle, diaphragmatic surface, and atrioventricular grooves[4,5]. Computed tomography (CT) scan is useful to define pericardial disease and to distinguish coronary, pericardial, myocardial, and intraluminal calcification. In many cases of constrictive pericarditis, CCTA signs of pericardial constriction will be presented and help to confirm the diagnosis. This includes global or focal pericardial thickening (> 4 mm) or calcification, tube-like configuration of ventricles, narrowing of atrioventricular groove, and sinuous appearance of the intraventricular septum[6]. CCTA scan may also shows enlargement of atriums, and enlargement of SVC (> the diameter of descending aorta) and IVC (> twice the diameter of descending aorta)[6]. Magnetic resonance imaging can accurately demonstrates pericardial thickening and provides additional functional analysis of constrictive physiology. Similarly, echocardiogram may demonstrate pericardial thickening or echogenic shadowing from calcium, and an enlargement of one or both atrium, IVC and hepatic veins[3]. Respiratory variation of ≥ 25% of early mitral inflow velocity is a well-recognized echocardiographic feature of constrictive pericarditis, which does not exhibits in those with restrictive cardiomyopathy[7]. Right heart catheterization (RHC) provides documentation of the hemodynamics of constrictive physiology and assists in discriminating between constrictive pericarditis and restrictive cardiomyopathy. RHC demonstrates preserved x descent and a prominent y descent, elevated right atrial pressure and right ventricular end diastolic pressure. Left atrial and left ventricular pressures are usually elevated. The equalization of diastolic pressures of all chambers (within less than 5 mmHg) with impaired diastolic filling pattern is a hallmark of constrictive physiology[3]. In our case, pericardial calcification was discovered incidentally without imaging findings suggestive of constrictive physiology. An example illustrating respiratory variation of mitral and tricuspid inflow velocity of a patient with constrictive pericarditis is shown in Figure 3.
The 2010 Appropriate Use Criteria for Cardiac Computed Tomography found that CACS use is appropriate in asymptomatic, intermediate-risk CHD patients, and this unanimous advocacy by the American College of Cardiology Foundation could have a significant impact on therapeutic decision-making and intervention[8]. In our case, pericardial calcification was discovered incidentally on non-contrast cardiac CT for CACS for further coronary artery risk stratification. Our patient has an in intermediate 10-year risk (17%) for hard CHD events such as myocardial infarction and CHD death, using the Framingham risk scoring[9]. As detailed in the 2010 ACC/AHA Guideline for assessment of cardiovascular risk in asymptomatic adults, CACS use is appropriate for evaluating this patient’s elevated risk for future cardiovascular events[10]. Ultimately, the goal of our assessment is to refine targeted preventative efforts based on patient risk.
Although detecting and recognizing pericardial calcification on chest radiography and other imaging modalities such as CT, and echocardiography may have important clinical implications, it requires further investigations and multimodal cardiac imaging in expediting the diagnosis. Pericardial calcification is thought to occur after extensive scarring of the pericardium, and the fibrotic change in the pericardium may produce pericardial constriction. However, asymptomatic pericardial calcifications may be increasingly encountered by the use of cardiac computed tomography[1,11]. In a study of 1812 consecutive patients underwent electron-beam tomography for CACS, Hunold et al[12] found that approximately 1% (17/1812) had pericardial calcification without sign of pericardial constriction on the echocardiogram. Approximately 30% of patients with calcified pericardium may have signs and symptoms of constrictive pericarditis, and up to 50% of patients with constrictive pericarditis demonstrate pericardial calcification on plain chest radiographs[1,5]. Hence, the absence of calcification does not exclude constrictive pericarditis.
Due to the increase use of CACS and CCTA for the assessment of coronary atherosclerosis, incidental findings of pericardial calcification may become increasingly apparent, with or without significant clinical implications. The presence of pericardial calcification may suggest of diffused pericardial scarring and raises concerns for secondary associated processes and complications such as pericardial constriction. However, a thickened pericardium or calcification per se is not diagnostic of constrictive pericarditis. Pericardial constriction can occur without pericardial thickening or calcification, and calcification can be seen in the absence of constrictive physiology. If constriction is strongly suggested on clinical contexts, it should only be undertaken after careful consideration to establish or exclude the diagnosis. Calcification of the pericardium must be evaluated with full clinical knowledge to facilitate an accurate diagnosis and an appropriate therapy when required.
A 58-year-old Caucasian man with hypertension, hyperlipidemia but nonsmoker, and no remarkable history of heart disease presented to cardiology clinic for cardiovascular risk assessment without having any symptoms.
Lungs were clear to auscultation. Normal heart sounds, no S3 or S4, no murmurs, and no rubs. No hepatomegaly or extremity edema.
Non-contrast cardiac computed tomography for coronary artery calcium scoring revealed a low agatston score of 25.5 and incidental finding of moderate pericardial calcification.
Pericardial calcification with and without constrictive pericarditis.
Monitoring for signs and symptoms of pericardial constrictions is sufficient for asymptomatic pericardial calcification.
Incidental pericardial calcification is rare but may become more apparent due to the widespread application of cardiac computed tomography.
Calcification of the pericardium must be evaluated with full clinical knowledge to facilitate an accurate diagnosis and an appropriate therapy when required.
Pericardial calcification is an occasional finding in patients undergoing computed tomography (CT) scan for coronary artery assessment or calcium score. Its clinical meaning remains unsettled and unless causing pericardial constriction, does not require any therapeutic intervention. In this manuscript, moving from the observation of a patient with pericardial calcification, authors address this fortuitous and serendipitous finding in patients undergoing CT scan for other purposes. The manuscript is interesting and minor changes would improve its readability.
| 1. | Mathewson FA. Calcification of the pericardium in apparently healthy people; electrocardiographic abnormalities found in tracings from apparently healthy persons with calcification of the pericardium. Circulation. 1955;12:44-51. [PubMed] |
| 2. | Isaacs D, Stark P, Nichols C, Antevil J, Shabetai R. Post-traumatic pericardial calcification. J Thorac Imaging. 2003;18:250-253. [PubMed] |
| 3. | Sengupta PP, Eleid MF, Khandheria BK. Constrictive pericarditis. Circ J. 2008;72:1555-1562. [PubMed] |
| 4. | Ling LH, Oh JK, Breen JF, Schaff HV, Danielson GK, Mahoney DW, Seward JB, Tajik AJ. Calcific constrictive pericarditis: is it still with us? Ann Intern Med. 2000;132:444-450. [PubMed] |
| 5. | Ferguson EC, Berkowitz EA. Cardiac and pericardial calcifications on chest radiographs. Clin Radiol. 2010;65:685-694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Reinmüller R, Gürgan M, Erdmann E, Kemkes BM, Kreutzer E, Weinhold C. CT and MR evaluation of pericardial constriction: a new diagnostic and therapeutic concept. J Thorac Imaging. 1993;8:108-121. [PubMed] |
| 7. | Hatle LK, Appleton CP, Popp RL. Differentiation of constrictive pericarditis and restrictive cardiomyopathy by Doppler echocardiography. Circulation. 1989;79:357-370. [PubMed] |
| 8. | Taylor AJ, Cerqueira M, Hodgson JM, Mark D, Min J, O’Gara P, Rubin GD. ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the North American Society for Cardiovascular Imaging, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. J Cardiovasc Comput Tomogr. 2010;4:407.e1-407.33. [PubMed] [DOI] [Full Text] |
| 9. | Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Stone NJ. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004;110:227-239. [PubMed] |
| 10. | Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG. 2010 ACCF/AHA guideline for assessment of cardiovascular risk in asymptomatic adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2010;56:e50-103. [PubMed] [DOI] [Full Text] |
| 11. | Lewis WM, Killip T. Traumatic calcific nonconstrictive pericarditis. Am J Cardiol. 1965;16:901-905. [PubMed] |
| 12. | Hunold P, Schmermund A, Seibel RM, Grönemeyer DH, Erbel R. Prevalence and clinical significance of accidental findings in electron-beam tomographic scans for coronary artery calcification. Eur Heart J. 2001;22:1748-1758. [PubMed] |
P- Reviewer: Schoenhagen P, Sicari R, Said SAM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ