INTRODUCTION
Cerebrovascular occlusive disease due to atherosclerosis is a common cause of stroke worldwide. However, there are marked racial differences in the distribution of vascular stenosis. Extracranial stenosis is the most common large vessel cause in Caucasians, while intracranial stenosis is more prevalent in Asians, Hispanics and African-Americans[1-4]. Moreover, recent studies suggested that concurrent stenoses of extracranial and intracranial vessels are common in Asians. The purpose of this review is to examine the epidemiology, risk factors, stroke mechanism and genetics of concurrent stenoses and to discuss strategies for investigations and treatment.
EPIDEMIOLOGY
The incidence of concurrent stenoses ranges from 10% to 48% in patients with symptomatic cerebrovascular disease[2,5-8]. Wong et al[9] found that 21% of stroke patients had concurrent stenoses in Hong Kong. Yang et al[10] report 33% of stroke patients had concurrent stenoses in China. Liu et al[8] found that 18% of stroke patients in Taiwan had significant concurrent stenoses. Lee et al[6] reported that 48% of patients with more than 30% extracranial carotid stenosis had concurrent intracranial stenoses in South Korea.
NATURAL HISTORY OF CONCURRENT STENOSES
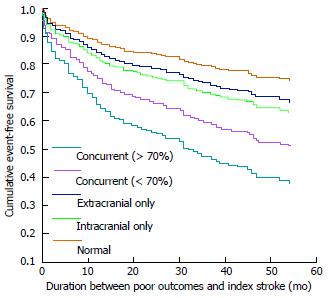
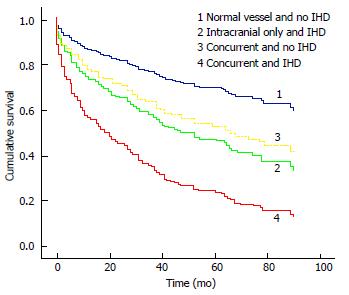
The long-term prognosis of ischemic stroke patients with concurrent atherosclerosis of intracranial and extracranial vessels is poor and they are at high risk of further vascular events or death. Our previous studies showed the 5-year cumulative rates of mortality, re-stroke and poor outcomes were 31%, 41% and 51%, respectively (Figure 1)[11]. Furthermore, ischemic stroke patients with concurrent stenoses and ischemic heart disease have an even worse prognosis. The 5-year cumulative rates of mortality, recurrent vascular events and combined poor outcomes were 40%, 50% and 83%, respectively (Figure 2)[12]. On the other hand, patients with concurrent stenoses and small vessel disease have poorer cognitive and functional outcomes[13]. This may be related to the burden of atherosclerosis and synergistic effect of multiple vascular lesions.
Figure 1 Cumulative event-free survival in patients with different intracranial and extracranial lesions.
Concurrent (< 70%): Concurrent lesions with < 70% extracranial stenosis; Concurrent (> 70%): Concurrent lesions with > 70% extracranial stenosis; Extracranial only: Extracranial stenosis only; Intracranial only: Intracranial stenosis only; Normal: Normal craniocervical vasculature.
Figure 2 Cumulative event-free survival of combined poor outcomes of different groups of patients.
Normal vessel: Normal craniocervical vasculature; Intracranial only: Intracranial stenosis only; Concurrent: Concurrent stenoses.
RISK FACTORS ASSOCIATED WITH CONCURRENT STENOSES
Our previous studies showed that hypertension[14], diabetes mellitus[15], hyperlipidemia[15], recurrent stroke and poor pre-stroke modified Rankin scale[16] are associated with concurrent stenoses.
ETIOLOGIES
The major cause of concurrent stenoses is atherosclerosis of the cerebrovascular circulation which typically affects large or medium sized arteries. These vessels range from 200-850 μm in diameter and are characterized by the accumulation of subintimal foam cells[16]. In the carotid artery, high risk plaques tend to be severely stenotic[17]. However, severe stenosis of the carotid artery is rare in Asian patients with concurrent stenosis[11]. Compared with extracranial vessels, the adventitia and the media of the intracranial arteries are thinner and their internal elastic lamina are fenestrated differently and thicker[18]. Luminal stenosis, lipid area, presence of neovasculature and inflammatory cells are all associated with ischemic stroke in the middle cerebral artery (MCA) territory[19].
STROKE MECHANISMS
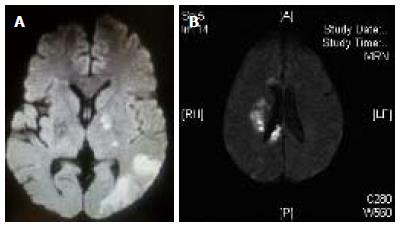
Patients with concurrent stenoses have more symptomatic stenoses, more concomitant perforating artery infarcts, pial infarcts, border zone infarcts and more multiple embolic infarcts in the territory of the leptomeningeal branches of MCA (Figure 3)[14]. The topographic patterns suggest that the combination of hemodynamic compromise attributable to concurrent stenoses and artery-to-artery embolization is a common stroke mechanism in these patients[14].
Figure 3 Magnetic resonance imaging diffusion-weighted images of different lesion patterns.
A: Concomitant perforating artery infarct and pial infarcts; B: Border zone infarcts.
GENETICS
Genetic factors may play a role in the development of concurrent stenoses on top of the other well established vascular risk factors. Our study showed that genetic polymorphisms of the pathways affecting lipid metabolism and homocysteine are associated with concurrent stenosis[15].
TREATMENT OF CONCURRENT STENOSES
Patients with concurrent stenoses are at high risk of further vascular events or death. The optimal treatment for these groups of patients is still unknown. The American Heart Association/American Stroke Association recommend aspirin monotherapy, aspirin/extended-release dipyridamole combination and clopidogrel monotherapy as the acceptable options for all non-cardioembolic ischemic stroke patients[20]. A South Korean study[21] showed that the progression of intracranial stenosis was significantly less in patients taking cilostazol (a phosphodiesterase inhibitor).
However, medical treatment for patients with concurrent stenoses is often unsatisfactory[11,12] and surgical treatment may be indicated in these patients. Although severe carotid stenosis is rare in Asians, patients with severe carotid stenosis are recommended to have a carotid endarterectomy[17,22]. Carotid stenting is not recommended due to high perioperative risks and death associated with this procedure[23,24].
The Carotid Occlusion Surgery Study trial, which investigated the relationship between cerebral hemodynamics and cognitive function in stroke patients undergoing treatment for unilateral carotid artery occlusion with extracranial-intracranial arterial bypass (EC-IC bypass), was stopped prematurely in 2011 because of slow recruitment and a very low incidence of ipsilateral symptomatic ischemic events in patients assigned to the medical arm[25].
The increasing enthusiasm for intracranial stenting for significant intracranial stenosis was dampened by the significant periprocedural neurological complication rate, estimated at 5.3% to 28%[26-30]. The stenting vs aggressive medical management for prevention recurrent stroke in intracranial stenosis (SAMMPRIS) trial[31] has been halted due to the high perioperative risks of stroke and death in the treatment arm. However, the risks may be lower at centers with high volume and more experience in these stenting procedures. Jiang et al[32] reported on 100 consecutive patients from a single center with a 99% success rate of stent placement and 5% risk of 30 d perioperative stroke and death. Overall, the current evidence does not support the routine use of intracranial stenting in patients with intracranial stenosis.
TRIALS IN PROGRESS
There are two ongoing randomized treatment trials using cilostazol in patients with intracranial stenosis. The first is the Trial of Cilostazol in Symptomatic Intracranial Arterial Stenosis II in Asia, which is a double-blind, randomized trial comparing aspirin (75-150 mg per day) in combination with cilostazol (100 mg twice a day) with a combination of clopidogrel (75 mg per day) in patients with significant MCA or basilar artery stenosis[33]. The second is the open-label trial of Cilostazol-Aspirin Therapy Against Recurrent Stroke With Intracranial Artery Stenosis in Japan, comparing open-label aspirin and cilostazol with aspirin alone in patients with symptomatic 50%-99% stenosis of the supraclinoid internal carotid artery, MCA or basilar artery[34]. These trials may provide important information to optimize medical treatment in patients with intracranial stenosis.
Concerning the surgical treatment for intracranial stenosis, the Japanese EC-IC Bypass Trial (JET study) is in progress to determine the ability of STA-MCA bypass to prevent stroke caused specifically by intracranial stenosis, based on evaluations of hemodynamic ischemia[35,36]. The interim analyses of the JET study suggest that in patients with symptomatic intracranial stenosis and evidence of hemodynamic ischemia, surgical intervention with EC–IC bypass is superior to medical management in terms of stroke prevention. The final results of the trial are pending[36].
The Early Stent-assisted Angioplasty in Symptomatic Intracranial Stenosis (ESASIS) trial[37] aims to study the benefit of stenting in reducing the risk of ipsilateral stroke, similar to the SAMMPRIS trial. The Data Safety Monitoring Board of the ESASIS study reviewed the 30 d safety data (combined stroke and death) of 77 randomized patients and found that the safety data of the stenting arm is reassuring when compared with that of the medical arm and is better than the high event rate of 14% being reported in the stenting arm of the SAMMPRIS study. The ESASIS trial is therefore recommended to continue recruitment but with close monitoring of safety.
CONCLUSION
Concurrent intracranial and extracranial stenoses are common in Asians. The patients have a high risk of death and recurrent vascular events. The risk factors include hypertension, diabetes mellitus, hyperlipidemia, previous history of stroke and poor pre-stroke modified Rankin scale. The combination of hemodynamic compromise attributable to concurrent stenoses and artery-to-artery embolization is a common stroke mechanism in these patients. Optimal treatment for patients with concurrent stenoses is still unknown and more studies are needed on possible interventions which can improve the prognosis of these patients.
P- Reviewers: Juttler E, Kobayashi T S- Editor: Song XX L- Editor: Roemmele A E- Editor: Wu HL