Published online Feb 16, 2014. doi: 10.12998/wjcc.v2.i2.36
Revised: December 20, 2013
Accepted: January 15, 2014
Published online: February 16, 2014
Processing time: 99 Days and 8.5 Hours
Variations in the bile duct and pancreatic duct opening are related to the process of rotation and recanalization during embryologic development. Complete non-union of distal common bile duct and pancreatic duct gives rise to double papillae of Vater. The separation of the drainage of the main pancreatic duct and bile duct can be appreciated by careful assessment at the time of endoscopic retrograde cholangiopancreatograpy. The cranial orifice is a bile duct opening, whereas the caudal orifice is a pancreatic duct opening. The separate orifice finding can be confirmed by cholangiogram and pancreatogram with no communication between the two orifices. Endoscopists should be aware of this rare variant because late recognition can result in unnecessary manipulation and contrast injections of the main pancreatic duct and biliary cannulation failure.
Core tip: Drainage of the main pancreatic and bile duct as two separate orifices is a recognized, but very rare anatomical variant. It is also referred to as double major papillae.
- Citation: Chavalitdhamrong D, Draganov PV. Unexpected anomaly of the common bile duct and pancreatic duct. World J Clin Cases 2014; 2(2): 36-38
- URL: https://www.wjgnet.com/2307-8960/full/v2/i2/36.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i2.36
The common bile duct and the pancreatic duct coalesce into one duct at the level of the ampulla, before they open into the duodenum via a single orifice. A variation in the bile duct and pancreatic duct opening causing two separate orifices is a rare anatomical variant as they fail to coalesce (also known as double papillae). This variant does not predispose to any pancreatobiliary disease, but recognition at the time of endoscopic retrograde cholangiopancreatography (ERCP) is crucial to ensure the procedures technical success. We present a case of a patient with separate drainage orifices of the bile and pancreatic duct which initially was not appreciated. This resulted in obtaining unnecessary pancreatograms, a prolonged procedure and increased risk for post-ERCP pancreatitis.
A 27-year-old presented 3 wk post-partum with acute right upper quadrant abdominal pain associated with elevated liver function tests (aspartate aminotransferase of 396 U/L, alanine aminotransferase of 364 U/L, total bilirubin of 1.5 mg/dL, and alkaline phosphatase of 510 U/L). Abdominal ultrasonography revealed a dilated common bile duct of 12 mm and mild intrahepatic ductal dilatation. Magnetic resonance cholangiopancreatography showed a four millimeter stone in the distal common bile duct.
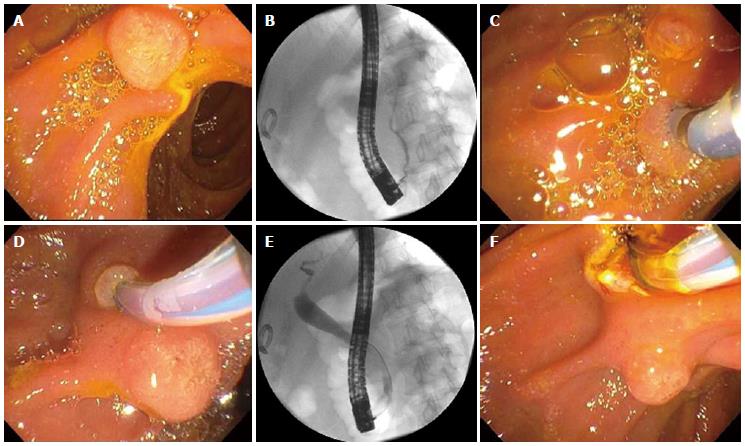
The patient underwent an ERCP for stone removal. The major papilla appeared normal (Figure 1A). Multiple cannulation attempts resulted in repeat pancreatograms (Figure 1B). The major papilla was re-examined, and what originally was thought to be the minor papilla was found to be located at the roof of the major papilla (Figure 1C). This appearance raised the possibility of two separated orifices of the bile duct and the main pancreatic duct, which independently drain with a separation of 10 mm. Indeed, that was confirmed after cannulation of the bile duct through the second orifice (Figures 1D and E). Biliary sphincterotomy was preformed (Figure F) and the biliary stone was easily extracted. Rectal indomethacin was given as a prophylactic measure for prevention of post-ERCP pancreatitis[1]. The patient later underwent a cholecystectomy, and her hospital course was uneventful.
Drainage of the main pancreatic and bile duct as two separate orifices is a recognized, but very rare anatomical variant. It is also referred to as double major papillae. The two separate openings are usually not apparent without close inspection[2]. The cranial orifice communicates with the common bile duct and the caudal orifice communicates with the duct of Wirsung[3]. Double papilla of Vater cannulation of the common bile duct and pancreatic duct could be accomplished through either orifice independently[4,5]. Endoscopists should be aware of this rare variant because late recognition can result in unnecessary manipulation and contrast injections of the main pancreatic duct. Fortunately, our patient did not develop post-ERCP pancreatitis. Furthermore, inability to recognize this anatomic variant can lead to biliary cannulation failure.
This case demonstrates a rare endoscopic finding of papilla during endoscopic retrograde cholangiopancreatography.
A non-union of the bile duct and pancreatic duct opening causes two separate orifices.
The confirmation of two separate ampullary structures can differentiate double major papillae of Vater from other diagnoses.
Cannulation of both orifices can prove that they are the openings of the common bile duct and the pancreatic duct.
Cannulation of the cranial orifice shows cholangiogram, whereas cannulation of the caudal orifice shows pancreatogram.
Cannulation of each orifice can evaluate the biliary or pancreatic abnormality.
Therapeutic interventions by endoscopic retrograde cholangiopancreatography (ERCP) can be performed after proper cannulation.
A literature search revealed only a few documented cases of double papillae of Vater.
Double major papillae of Vater are separate drainages of the common bile duct and the pancreatic duct. The cannulation of the common bile duct and pancreatic duct can be achieved through either orifice independently.
The unnecessary pancreatograms are associated with increased risk for post-ERCP pancreatitis. Fortunately, the patient did not develop post-ERCP pancreatitis.
Careful inspection of the ampulla finding the two openings can lead to appropriate cannulation of the common bile duct and pancreatic duct through either orifice independently.
| 1. | Yaghoobi M, Rolland S, Waschke KA, McNabb-Baltar J, Martel M, Bijarchi R, Szego P, Barkun AN. Meta-analysis: rectal indomethacin for the prevention of post-ERCP pancreatitis. Aliment Pharmacol Ther. 2013;38:995-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 2. | Katsinelos P, Chatzimavroudis G, Fasoulas K, Katsinelos T, Pilpilidis I, Lazaraki G, Terzoudis S, Kokonis G, Patsis I, Zavos C. Double major papilla of Vater--a rare endoscopic finding during endoscopic retrograde cholangiopancreatography: a case report. Cases J. 2009;2:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Francis JM, Kadakia SC. Anomalous double orifice of a single major papilla of Vater. Gastrointest Endosc. 1994;40:524-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Rajnakova A, Tan WT, Goh PM. Double papilla of Vater: a rare anatomic anomaly observed in endoscopic retrograde cholangiopancreatography. Surg Laparosc Endosc. 1998;8:345-348. [PubMed] |
| 5. | Ratanalert S, Soontrapornchai P. Double orifices of a single major papilla of vater: a rare case report. Gastroenterol Nurs. 2007;30:243-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
P- Reviewers: Assimakopoulos SF, Gassler N, Sandblom G, Xu Z S- Editor: Gou SX L- Editor : A E- Editor: Wu HL