Published online Jan 16, 2014. doi: 10.12998/wjcc.v2.i1.24
Revised: October 31, 2013
Accepted: December 9, 2013
Published online: January 16, 2014
Processing time: 95 Days and 16 Hours
Jejunogastric intussusception is a rare long term complication of Billroth II gastrectomy. The case reported here is a 50 year old man with history of a Billroth II gastrectomy and Braun’s side-to-side jejunojejunal anastomosis who presented with hematemesis. On abdominal examination, there was a mass in the left iliac fossa. Computed tomography scan showed a retrograde jejunogastric intussusception across the gastrojejunostomy. On laparotomy, a retrograde intussusception of the distal jejunum through the jejunojejunal anastomosis and across the gastrojejunostomy with a gangrenous intussusceptum was found. The jejunojejunal anastomosis was taken down, the gangrenous segment was resected and bowel continuity was restored with two jejunojejunal anastomoses, proximal and distal to the gastrojejunostomy. The gastrojejunostomy was preserved. This case brings out an unusual type of retrograde gangrenous intussusception which occurred at two points of a previous anastomosis, i.e., jejunojejunostomy and gastrojejunostomy simultaneously, which could be managed with jejunal resection.
Core tip: Retrograde jejunojejunal and jejunogastric intussusceptions are rare. The occurrence of retrograde intussusception across two anastomoses has not been reported in the literature. A high index of suspicion and timely investigations like an esophagogastroscopy or a computed tomography scan will help to clinch the diagnosis early. Emergency surgical intervention can help to prevent clinical deterioration and save the life of the patient. We would like to emphasize the fact that a high index of clinical suspicion should be maintained in patients with gastroenteric anastomosis who present with hematemesis for the possibility of a retrograde jejunogastric intussusception; the results can be gratifying.
- Citation: Gopal R, Elamurugan TP, Hage S, Muthukumarassamy R, Kate V. Retrograde jejunogastric intussusception following Braun’s jejunojejunostomy. World J Clin Cases 2014; 2(1): 24-26
- URL: https://www.wjgnet.com/2307-8960/full/v2/i1/24.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i1.24
Retrograde jejunogastric intussusception is a potentially fatal complication of Billroth II gastrectomy[1,2]. It is a rare complication of this procedure, with only just over 200 cases reported[2]. Retrograde jejunogastric intussusception can present with varied clinical presentations, like abdominal pain, vomiting, hematemesis, gastric outlet or intestinal obstruction and gangrene gut[1,3-6]. There are limited case reports of jejunojejunal intussusception through a Braun’s jejunojejunostomy in cases of total gastrectomy[7]. To the best of our knowledge, there are no reported cases of hematemesis presenting in a patient with retrograde jejunogastric intussusception through a Braun’s jejunojejunostomy. We present a case that brings out an unusual type of retrograde gangrenous intussusception which occurred across two points of previous anastomosis, i.e., jejunojejunostomy and gastrojejunostomy simultaneously, and presented with hematemesis.
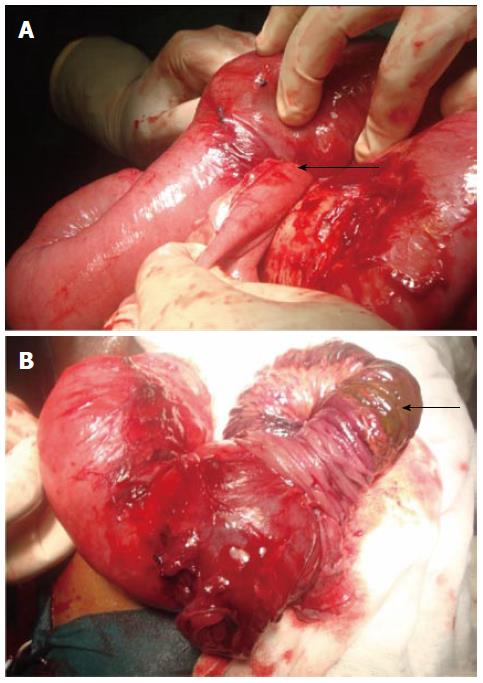
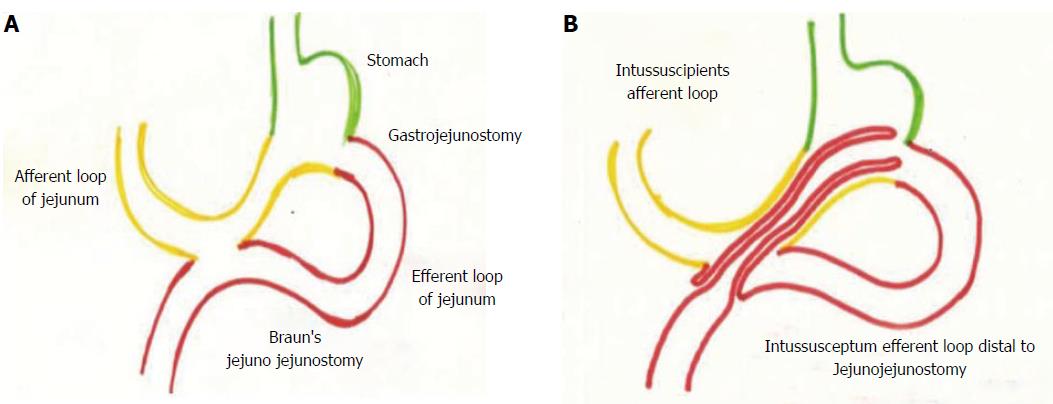
A 50 year old gentleman who had undergone a Billroth II gastrectomy and Braun’s side-to-side jejunojejunal anastomosis five years ago for gastric outlet obstruction presented to our emergency department with a one day history of hematemesis. He had five episodes of vomiting altered blood. He gave no history of anything similar in the past. The patient was hemodynamically stable. Abdominal examination did not show any peritoneal signs. An 8 cm × 8 cm mass was palpable in his left iliac fossa. There was no palpable hepatosplenomegaly. An upper gastrointestinal endoscopy was attempted but visualization was poor due to the pooled altered blood. An emergency computed tomography (CT) scan of the abdomen revealed a retrograde intussusception of the jejunum into the stomach across the gastrojejunostomy (Figure 1). The patient was stabilized and taken up for emergency laparotomy. The findings of the CT scan were confirmed intraoperatively. The patient had a gastrojejunostomy and a diverting Braun’s side-to-side jejunojejunal anastomosis. The efferent limb of the jejunum distal to the jejunojejunal anastomosis was seen telescoping across the jejunojejunostomy (Figure 2A) into the stomach through the gastrojejunostomy. Schematic representation of the normal anatomy and the retrograde intussusception is shown in Figure 3. The intussuscepted segment was gangrenous (Figure 2B) and there was around 500 mL of altered blood in the stomach but there was no obvious peritoneal contamination. The rest of the bowel, including the intussuscipiens segment, appeared viable. The jejunojejunal anastomosis was taken down and the contents reduced. The gangrenous segment of the jejunum was resected and the gastrojejunostomy was preserved. The bowel continuity was restored with two jejunojejunal anastomoses, one proximal and one distal to the gastrojejunostomy. A Witzel’s type of feeding jejunostomy was placed distal to the second anastomotic line in the efferent loop. The postoperative period was uneventful. The patient’s bowel activity returned to normal on the fourth postoperative day. He was initially started on jejunostomy feeds on the fifth postoperative day, on oral diet in the second postoperative week and discharged from hospital after removal of the feeding jejunostomy tube. The patient was asymptomatic at the first and second month follow-up visits.
Retrograde jejunojejunal and jejunogastric intussusceptions are rare but dangerous long term complications of Billroth II gastrectomy and gastrojejunostomy. Jejunogastric intussusception is more common than the jejunojejunal variety[8]. There have also been reports of retrograde intussusception in patients who have undergone Roux-en-Y gastrointestinal anastomosis after gastrectomy[9] but the occurrence of retrograde intussusception across two anastomoses has not been reported in the literature. A high index of suspicion and timely investigations like an esophagogastroscopy or a CT scan will help to clinch the diagnosis early. Emergency surgical intervention can help to prevent clinical deterioration and save the life of the patient[2]. All the reported cases of retrograde intussusceptions of jejunum into the stomach through a gastrojejunostomy have been managed by emergency laparotomy and appropriate resection procedures. In our case also, the relatively early presentation, the clinical suspicion and timely imaging helped in the early diagnosis and proper management and survival of the patient. We would like to emphasize the fact that a high index of clinical suspicion should be maintained in patients with gastroenteric anastomosis who present with hematemesis for the possibility of a retrograde jejunogastric intussusception; the results can be gratifying.
A 50 year old man with history of a Billroth II gastrectomy and Braun’s side-to-side jejunojejunal anastomosis presented with hematemesis and mass in the left iliac fossa.
Unusual type of retrograde gangrenous intussusception which occurred at two points of previous anastomosis, i.e., jejunojejunostomy and gastrojejunostomy simultaneously.
Clinical examination, upper gastrointestinal endoscopy and imaging methods can help in arriving at the diagnosis.
Computed tomography scan showed a retrograde jejunogastric intussusception across the gastrojejunostomy.
The jejunojejunal anastomosis was taken down, the gangrenous segment of jejunum was resected and bowel continuity was restored with two jejunojejunal anastomoses, proximal and distal to the gastrojejunostomy.
Braun’s gastrojejunostomy: gastrojejunostomy with diverting jejunojejunal anastomosis.
A high index of clinical suspicion should be maintained in patients with gastroenteric anastomosis who present with hematemesis for the possibility of a retrograde jejunogastric intussusception.
This is an interesting subject with very good pictures.
| 1. | Miah AG, Imam NA, Joarder RH, Talukder SI, Hossain MS. Retrograde jejunogastric intussusception (JGI) with strangulation following previous gastrojejunostomy. Mymensingh Med J. 2006;15:99-101. [PubMed] |
| 2. | Tauro LF, Roshan M, Aithala PS, Hegde BR, Anand IP, John SK. A rare cause of haematemesis: retrograde jejunogastric intussusception. J Assoc Physicians India. 2006;54:333-335. [PubMed] |
| 3. | Edwards JL, Aubrey DA. Retrograde jejunogastric intussusception: report of 2 cases. Br J Surg. 1977;64:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Bapaye M, Kolte S, Pai K, Godse A, Pardeshi A, Bhave A, Kumar A. Jejunogastric intussusception presenting with outlet obstruction. Indian J Gastroenterol. 2003;22:31-32. [PubMed] |
| 5. | Gupta S, Singh G. Retrograde jejunogastric intussusception: an unusual cause of hematemesis (a case report). J Postgrad Med. 1986;32:105-106. [PubMed] |
| 6. | Wolukau-Wanambwa PP. An uncommon cause of haematemesis--retrograde jejuno-gastric intussusception. Br J Clin Pract. 1979;33:53-54, 58. [PubMed] |
| 7. | Jang WI, Kim ND, Bae SW, Kim WT, Kwon SO, Yoon KS, Kim SY. Intussusception into the enteroanastomosis after Billroth II gastric resection; diagnosed by gastroscopy. J Korean Med Sci. 1989;4:51-54. [PubMed] |
| 8. | Kwak JM, Kim J, Suh SO. Anterograde jejunojejunal intussusception resulted in acute efferent loop syndrome after subtotal gastrectomy. World J Gastroenterol. 2010;16:3472-3474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
P- Reviewer: Andrei S S- Editor: Wen LL L- Editor: Roemmele A E- Editor: Wang CH