Published online Feb 16, 2025. doi: 10.12998/wjcc.v13.i5.97909
Revised: October 11, 2024
Accepted: November 4, 2024
Published online: February 16, 2025
Processing time: 159 Days and 18.7 Hours
Oral cancer is one of the malignant neoplasms that present major global health challenge. It is the sixth most prevalent type of cancer in the world, with a high incidence and mortality rate. This letter is a review of the study by Yin et al which was published in the World Journal of Clinical Cases (2024). The study evaluated the effect of Tongluo Jiedu as an adjuvant treatment for oral cancer. Over the years, there has been a continuous search for effective and less invasive treatments for oral cancer. This article emphasizes and discusses various therapeutic options currently available, and it highlights that early intervention and multidisciplinary management are crucial for improving outcomes. Traditional Chinese medicine, particularly Tongluo Jiedu, presents potential complementary approach to co
Core Tip: In this letter, we highlight the article by Yin et al recently published in the World Journal of Clinical Cases (2024), which was focused on the benefits of Tongluo Jiedu as an adjuvant treatment for oral cancer. The study showed that this treatment improved immune function and reduced oxidative stress, thereby aiding recovery of the oral cancer patients. We emphasize the need for early intervention, multidisciplinary management, and the potential of integrating traditional Chinese medicine with conventional therapies.
- Citation: Lomelí Martínez SM, Martínez Nieto M, Mercado González AE. Tongluo Jiedu as an adjuvant therapy for oral cancer. World J Clin Cases 2025; 13(5): 97909
- URL: https://www.wjgnet.com/2307-8960/full/v13/i5/97909.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i5.97909
Oral cancer is an alarming global health problem with a high incidence and mortality rate. In 2021, the Global Cancer Statistics showed 377000 new cases of lip and oral cavity cancers worldwide, which resulted in approximately 177000 deaths[1]. Globally, oral cancer is the sixth most prevalent type of cancer, and it primarily affects individuals between the ages of 40 and 70 years, predominantly in the form of squamous cell carcinoma[2,3]. Despite advances in oncological treatments, the 5-year survival rate for oral cancer remains between 50% and 60%[1-4].
The stage at which oral cancer is diagnosed is a determining factor for both treatment and prognosis[4]. Unfortunately, two-thirds of oral cancer cases are diagnosed at the advanced stages (stages III and IV). Patients diagnosed in early stages (stage I) have a survival rate greater than 80%, which highlights the importance of early detection. However, early detection remains a challenge, as studies have revealed that in the last decade, only 28.7% of oral cavity and pharynx cancers were diagnosed at a local stage[4]. The prevalence of oral cancer varies significantly between regions, being highest in developing countries. Indeed, every year, approximately 270000 people are diagnosed with oral cancer, with two-thirds of these cases occurring in developing countries[5]. Due to these factors, there has been a constant search for more effective and less invasive treatments for oral cancer.
This letter emphasizes and analyzes the various therapeutic options currently available for oral cancer, while sup
Oral cancer is characterized by uncontrolled cell proliferation that invades and deteriorates adjacent tissues by negatively affecting essential functions such as eating, speaking, and breathing[6]. This neoplasm originates in the oral cavity areas such as the mucosa, gums, floor of the mouth, lips, front part of the tongue, hard palate, and retromolar trigone, and it may extend to the oropharynx[6]. The disease is driven by multiple molecular and cellular signaling pathways such as PI3K/AKT/mTOR, NF-κB, Wnt, Notch, MAPK/ERK, Hippo, and Hedgehog, which regulate cell growth, survival, and proliferation[3,7].
Several risk factors such as poor oral hygiene, excessive tobacco and alcohol use, chewing of betel leaf with areca nut and tobacco, and genetic mutations, contribute to the development of oral cancer[4,8]. Poor oral health may lead to chronic infections and inflammation, thereby creating an environment conducive for cancer development. Excessive consumption of tobacco and alcohol, particularly when combined, significantly increases the risk of oral cancer due to their carcinogenic properties. Additionally, genetic mutations that disrupt normal cell cycle regulation promote the uncontrolled growth characteristic of cancer[8]. Recent studies have demonstrated that human papillomavirus (HPV) is recognized as a significant risk factor in the development of oral cancer, particularly in oropharyngeal cancers. Spe
Early diagnosis of oral cancer is challenging due to its varied presentations which often resemble benign conditions, particularly in young and low-risk patients, leading to delayed diagnosis. Many healthcare professionals lack awareness of common oral lesions, and are reluctant to perform biopsies due to inexperience and limited resources[4]. Early dia
Over the years, several studies have been done, and ongoing research is still going on in order to find effective and less invasive treatments[11-13]. Typically, the conventional treatments involve surgery, radiotherapy, and chemotherapy, which are chosen based on the cancer type, location, stage, and the patient's overall condition[11,12]. Each of these treatments offers specific solutions, depending on the characteristics of the cancer. Therefore, there is need for making a careful evaluation prior to the selection of the most appropriate management approach for each patient.
Surgery is the most common treatment for oral cancer. It involves removal of the tumor and, in some cases, the surrounding tissues. This approach allows for the direct removal of the tumor, and it is crucial in the early stages of the disease. The advantages of this procedure include the possibility of complete elimination of the cancer if detected early, as well as achieving clear margins which improve the patient’s prognosis. However, it is associated with postoperative complications such as functional and aesthetic alterations which may affect the patient’s quality of life, especially when a significant part of the oral cavity such as the tongue or jaw, is removed[11].
On the other hand, radiotherapy is a management option used to destroy cancer cells in the affected area, and it may be applied as a primary treatment or as an adjuvant therapy following surgery. One of the main advantages of radiotherapy is its potential to reach tumors that are not surgically accessible, in addition to being a less invasive option[12,14]. However, radiotherapy has significant side effects, such as mucositis, xerostomia (dry mouth), and damage to su
Chemotherapy involves the use of drugs to destroy cancer cells. This treatment option is often used in combination with surgery or radiotherapy, especially in cases of advanced or metastatic cancer[13,14]. Two of the advantages of che
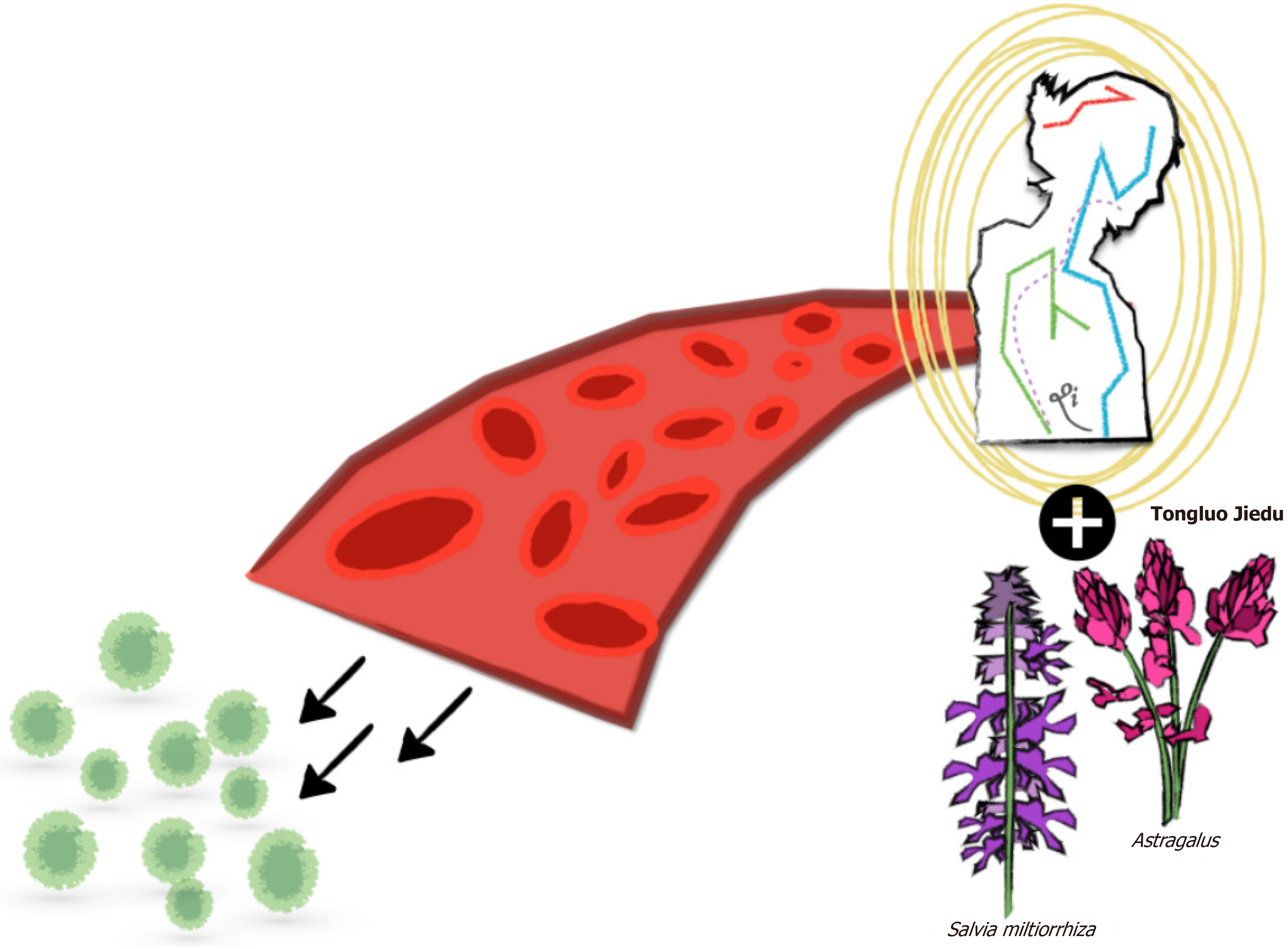
Complementary and alternative medicine, particularly traditional Chinese medicine (TCM), is gaining attention in the treatment of malignant tumors[5,15,16]. The preparation of TCM involves extraction and purification of bioactive compounds from herbs, insects, or animals, using modern scientific methods[5,16]. Plants such as Astragalus, Dandelion, and Salvia miltiorrhiza have shown benefits by boosting immunity and reducing oxidative stress[15]. The mechanism of action of Tongluo Jiedu formula, based on TCM theory, is described as "meridian circulation and toxin elimination." According to TCM, the human body has a system of meridians through which vital energy, or qi, flows. Blockages in these meridians lead to illness, and one of the primary goals of Tongluo Jiedu-based treatment is to unblock the me
The application of Tongluo Jiedu in the treatment of oral cancer has been the subject of several studies aimed at investigating its effectiveness and benefits, when compared to conventional treatments. In the recent 2024 issue of the World Journal of Clinical Cases, Yin et al[15] published a paper titled “Effects of Tongluo Jiedu prescription on immune function and oxidative stress in patients with oral cancer”, a retrospective study which evaluated the effect of Tongluo Jiedu (as an adjuvant treatment) on immune function and oxidative stress in oral cancer patients. Eighty patients with oral cancer included in the study were divided into two groups: A control group given conventional chemotherapy, and an ob
These findings are in line with those from a retrospective longitudinal study by Ben-Arie et al[18] and a prospective study by Wang et al[19]. The latter study was aimed at investigating the effect of anticancer TCM decoction when used together with basic chemotherapy and nursing intervention in patients with oral cancer after surgery. Eighty-four patients were divided into two groups: An observation group which received chemotherapy + TMC + nursing inter
On the other hand, the retrospective longitudinal study by Ben-Arie et al[18] used the Taiwan National Health In
The main advantage of integrating Tongluo Jiedu into oral cancer treatment is its comprehensive approach. TCM not only focuses on tumor elimination but also on increasing the general well-being of patients, balancing the immune system, and mitigating side effects. This complementary approach may be beneficial in cases where there is need to minimize the adverse effects of chemotherapy and radiotherapy. Although these results are promising, it is important to highlight that specific evidence of the effectiveness of TCM in oral cancer are limited. Therefore, more research is needed to establish its definitive role. While conventional oral cancer treatment remains the gold standard due to its proven effectiveness, Tongluo Jiedu presents a valuable complementary therapy. The use of Tongluo Jiedu in oral cancer ma
Biomarkers such as IL-6 and TNF-α play crucial roles in inflammatory and immune pathways which are fundamental pillars in the progression of cancer and the response of cancer to treatment. These pro-inflammatory mediators are involved in the pathogenesis of cancer, particularly in the context of oral cancer, and they have been subject of numerous studies aimed at better understanding of their influence on prognosis and the efficacy of therapeutic interventions[20,21].
IL-6 is a key factor that has been associated with three fundamental processes in cancer progression: Promotion of cell proliferation, inhibition of apoptosis, and induction of angiogenesis. This biomarker is associated with poor prognosis in patients with head and neck cancer, and its expression correlates directly with the severity of the disease and reduced response to conventional treatments such as chemotherapy and radiotherapy[20]. On the other hand, TNF-α plays a dual role in cancer. While TNF-α is known for its potential to induce inflammatory responses, it also promotes cell death under certain conditions. However, in the context of cancer, elevated levels of TNF-α foster an inflammatory tumor microenvironment that promotes the invasion and metastasis of malignant cells[21].
The monitoring and identification of these biomarkers provide a valuable tool for the early detection of immune alterations and tumor progression, and also act as a guide for more personalized therapeutic strategies. For example, in a recent study, it was suggested that modulation of these biomarkers through photo-biomodulatory therapies may have a positive impact on the reduction of the severity of conditions associated with cancer treatment, e.g., oral mucositis, thereby highlighting their potential in the comprehensive clinical management of patients[14].
The findings presented in the study by Yin et al[15] on the effect of Tongluo Jiedu on patients with oral cancer open the door to several important directions for future research, not only on the treatment, but also on understanding it as a therapeutic alternative. Large-scale clinical trials are essential for validating the efficacy and safety of Tongluo Jiedu in a broader population. This will confirm the benefits observed in preliminary studies and allow for a better understanding of its impact on different subgroups of patients.
Tongluo Jiedu has proven to be effective as a complementary treatment for oral cancer[15]. However, it will be beneficial to propose longitudinal studies with long-term follow-up of patients, for better understanding of its effectiveness, and to explore prognostic factors related to longevity, post-treatment quality of life, and disease-free survival. It is essential to delve into the molecular mechanisms through which Tongluo Jiedu exerts its therapeutic effects. The identification of the specific associated molecular pathways and predictive biomarkers will optimize its clinical application. Additionally, genetic research has the potential to aid personalized treatments based on patients' individual genetic characteristics.
Studies have shown that TCM improves immune response, reduces oxidative stress, and accelerates the recovery of patients. Thus, Tongluo Jiedu not only offers a complementary effect but also a synergistic effect when combined with chemotherapy and radiotherapy. This opens a promising avenue for future large-scale, well-designed multicenter clinical trials in order to further validate its efficacy and safety. Future research should focus not only on clinical outcomes but also on the molecular mechanisms through which Tongluo Jiedu exerts its effects. The understanding of these mechanisms, particularly those related to inflammation and immune modulation, will help optimize treatment strategies and identify potential biomarkers for personalized therapy. Indeed, the identification and validation of specific biomarkers for prediction of response to treatment with Tongluo Jiedu will allow for a more personalized and targeted therapeutic strategy for oral cancer. This process should involve the evaluation of markers of cell proliferation and apoptosis that are influenced by Tongluo Jiedu. Moreover, it will be interesting to test Tongluo Jiedu in combination with other recently introduced adjuvant treatments such as ozone therapy[22], photo-biomodulation[23], and para-probiotics[24], so as to understand their mutual effect on periodontal tissues.
Tongluo Jiedu showed potential as a complementary treatment for oral cancer, but more research is needed to establish its role in clinical practice. Possible risks associated with this treatment should be considered, including interactions with other therapies such as conventional treatments like chemotherapy and radiotherapy; unknown adverse effects, risk of toxicity, and the need for regulation and standardization, among others. Future research should be aimed at validation of its efficacy and safety through large, well-designed clinical trials; better understanding of the molecular mechanisms involved, and optimization of therapeutic combinations. Additionally, personalization of treatment through the use of biomarkers and genetic tests, along with continuous education for healthcare professionals, is essential for the safe and effective integration of traditional medicine into clinical practice.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 68462] [Article Influence: 13692.4] [Reference Citation Analysis (201)] |
| 2. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12461] [Article Influence: 6230.5] [Reference Citation Analysis (6)] |
| 3. | Kumari M, Chhikara BS, Singh P, Rathi B. Signaling and molecular pathways implicated in oral cancer: A concise review. Chem Biol Lett. 2023;11:652. [DOI] [Full Text] |
| 4. | Saka-Herrán C, Jané-Salas E, Mari-Roig A, Estrugo-Devesa A, López-López J. Time-to-Treatment in Oral Cancer: Causes and Implications for Survival. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Jiang D, Xiao F, Liu L, Meng Z, Zhang C. Effects of Traditional Chinese Medicine Anticancer Decoction Combined with Basic Chemotherapy and Nursing Intervention on Oral Cancer Patients after Surgery and Its Effect on Tumor Markers and Immune Function. Biomed Res Int. 2022;2022:6341381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Goswami B, Bhuyan MK, Alfarhood S, Safran M. Classification of Oral Cancer Into Pre-Cancerous Stages From White Light Images Using LightGBM Algorithm. IEEE Access. 2024;12:31626-31639. [DOI] [Full Text] |
| 7. | Dey S, Singh AK, Singh AK, Rawat K, Banerjee J, Agnihotri V, Upadhaya D. Critical pathways of oral squamous cell carcinoma: molecular biomarker and therapeutic intervention. Med Oncol. 2022;39:30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Kavyashree C, Vimala HS, Shreyas J. A systematic review of artificial intelligence techniques for oral cancer detection. Healthcare Analytics. 2024;5:100304. [DOI] [Full Text] |
| 9. | Muzio LL, Ballini A, Cantore S, Bottalico L, Charitos IA, Ambrosino M, Nocini R, Malcangi A, Dioguardi M, Cazzolla AP, Brauner E, Santacroce L, Cosola MD. Overview of Candida albicans and Human Papillomavirus (HPV) Infection Agents and their Biomolecular Mechanisms in Promoting Oral Cancer in Pediatric Patients. Biomed Res Int. 2021;2021:7312611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 10. | Saikia PJ, Pathak L, Mitra S, Das B. The emerging role of oral microbiota in oral cancer initiation, progression and stemness. Front Immunol. 2023;14:1198269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 42] [Reference Citation Analysis (0)] |
| 11. | Wong T, Wiesenfeld D. Oral Cancer. Aust Dent J. 2018;63 Suppl 1:S91-S99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | Liu C, Wang M, Zhang H, Li C, Zhang T, Liu H, Zhu S, Chen J. Tumor microenvironment and immunotherapy of oral cancer. Eur J Med Res. 2022;27:198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 78] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 13. | Szewczyk M, Pazdrowski J, Pieńkowski P, Wojtera B, Więckowska B, Golusiński P, Golusiński W. A Matter of Margins in Oral Cancer-How Close Is Enough? Cancers (Basel). 2024;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 14. | Khalil M, Hamadah O, Saifo M, Khalil H, Adi M, Alabeedi F, Kujan O. Effect of Photobiomodulation on Salivary Cytokines in Head and Neck Cancer Patients with Oral Mucositis: A Systematic Review. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 15. | Yin Y, Yao Y, Li YJ, Zhao LL, Zhang Q. Effects of Tongluo Jiedu prescription on immune function and oxidative stress in patients with oral cancer. World J Clin Cases. 2024;12:3045-3052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | Wang D, Duan X, Zhang Y, Meng Z, Wang J. Traditional Chinese medicine for oral squamous cell carcinoma: A Bayesian network meta-analysis protocol. Medicine (Baltimore). 2020;99:e22955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 17. | Youn BY, Kim JH, Jo YK, Yoon S, Im JY, Kim HJ, Lee JD, Ko SG. Current Characteristics of Herbal Medicine Interventions for Cancer on Clinical Databases: A Cross-Sectional Study. Integr Cancer Ther. 2023;22:15347354231218255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Ben-Arie E, Lottering B, Inprasit C, Yip HT, Ho WC, Ton G, Lee YC, Kao PY. Traditional Chinese medicine use in patients with oral cancer: A retrospective longitudinal cohort study in Taiwan. Medicine (Baltimore). 2022;101:e30716. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 19. | Wang M, Jiang H, Zhang M, Chen Y, Wang T, Li P. "Highly Exposed Chinese Herbal Medicine" Combined With Apatinib as Maintenance Treatment Following First-Line or Second-Line Chemotherapy for Extensive-Stage Small-Cell Lung Cancer: A Single-Arm, Prospective Study. Dose Response. 2021;19:15593258211055016. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Abati S, Bramati C, Bondi S, Lissoni A, Trimarchi M. Oral Cancer and Precancer: A Narrative Review on the Relevance of Early Diagnosis. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 206] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 21. | Montero PH, Patel SG. Cancer of the oral cavity. Surg Oncol Clin N Am. 2015;24:491-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 418] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 22. | Scribante A, Gallo S, Pascadopoli M, Frani M, Butera A. Ozonized gels vs chlorhexidine in non-surgical periodontal treatment: A randomized clinical trial. Oral Dis. 2024;30:3993-4000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 23. | Elbay M, Elbay ÜŞ, Kaya E, Kalkan ÖP. Effects of photobiomodulation with different application parameters on injection pain in children: a randomized clinical trial. J Clin Pediatr Dent. 2023;47:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 24. | Butera A, Pascadopoli M, Nardi MG, Ogliari C, Chiesa A, Preda C, Perego G, Scribante A. Clinical Use of Paraprobiotics for Pregnant Women with Periodontitis: Randomized Clinical Trial. Dent J (Basel). 2024;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/