Published online Dec 6, 2025. doi: 10.12998/wjcc.v13.i34.112593
Revised: August 27, 2025
Accepted: November 14, 2025
Published online: December 6, 2025
Processing time: 124 Days and 18.7 Hours
Complications occur in approximately 12% of cases of diverticulitis, with perf
A 66-year-old man presented with lower abdominal pain for 3 days. On examin
Pneumoretroperitoneum and pneumomediastinum are rare complications of perforated diverticulitis, often with delayed diagnosis due to the absence of peritoneal signs. CT aids detection, and timely surgical intervention is crucial.
Core Tip: This case highlights the rare but critical complications of pneumoretroperitoneum and pneumomediastinum in perforated diverticulitis, emphasizing the importance of high clinical suspicion in patients with atypical presentations. Timely computed tomography imaging and prompt surgical intervention are essential, as delayed diagnosis can lead to increased morbidity and mortality. Despite the absence of typical peritoneal signs, early detection and intervention are crucial for improving patient outcomes.
- Citation: Wu PE, Chen PJ, Su WC, Chang TK, Chen YC. Perforated sigmoid colon diverticulitis initially presenting with pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum: A case report. World J Clin Cases 2025; 13(34): 112593
- URL: https://www.wjgnet.com/2307-8960/full/v13/i34/112593.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i34.112593
Complications occur in approximately 12% of cases of diverticulitis[1]. Common complications include abscesses (69%), peritonitis (27%), obstruction (15%), and fistulas (14%)[1]. In patients with acute diverticulitis, the rate of perforation can reach 10%[2]. In the majority of cases, the perforation occurs intraperitoneally, and the patient may present with acute abdominal pain, nausea, and vomiting. Hemodynamic instability accompanied by hypotension and shock may occur in severe cases. Physical examination may reveal peritoneal signs with abdominal guarding, rigidity, and rebound tenderness. Unlike intraperitoneal perforation, pneumoretroperitoneum is a relatively rare complication of perforated diverticulitis. Because of the lack of typical symptoms, diagnosing retroperitoneal colon perforation can be challenging. Moreover, delayed diagnosis and treatment are associated with high morbidity and mortality rates[3]. According to the World Society of Emergency Surgery (WSES) guidelines, uncomplicated diverticulitis may be managed conservatively, whereas complicated diverticulitis, such as cases with perforation, typically requires urgent surgical or interventional management[4]. Herein, we present a rare case of a 66-year-old man who exhibited no toxic signs but received a diag
A 66-year-old man presented to the Emergency Department with a chief complaint of lower abdominal pain for the preceding 3 days.
The patient had experienced dull, intermittent lower abdominal pain for 3 days without any exacerbating or relieving factors. Nausea and poor appetite were also mentioned. He had a vomiting episode on the day he sought medical trea
The patient had history of hypertension and chronic obstructive pulmonary disease with medication control.
The patient had a 30-year history of smoking one pack per day but had quit smoking 5 years previously. He had no significant occupational or social issues, and no major contributory diseases or genetic disorders in the family had been recorded.
Physical examination revealed a soft and mildly distended abdomen. Mild tenderness was observed in the left lower quadrant with deep compression. Neither abdominal guarding nor rebounding pain suggesting peritoneal involvement was observed.
Laboratory tests revealed a white blood cell count of 18720 /μL, a neutrophil level of 91%, a hemoglobin level of 9.2 g/dL, a creatinine level of 1.75 mg/dL, and a C-reactive protein level of 403.19 mg/dL; other parameters were within normal limits.
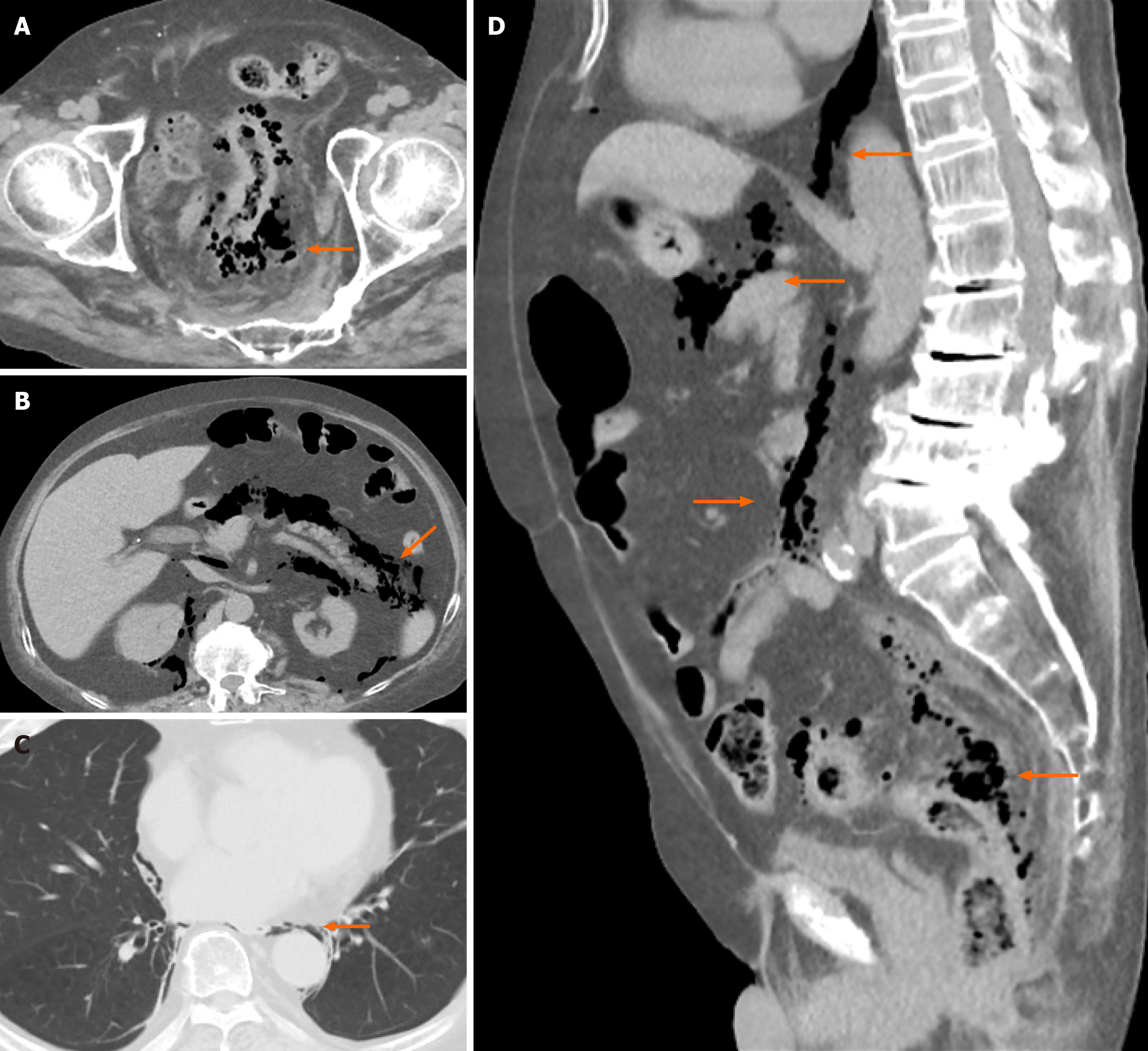
Abdominal computed tomography (CT) was performed with intravenous contrast. Axial, sagittal and coronal reconstructions were obtained. The CT examination revealed mural changes including focal wall thickening and edematous changes at the rectosigmoid junction. The extramural findings were peripheral fat stranding around the affected segment, diffuse pneumoretroperitoneum around the pancreas and kidneys, minor pneumoperitoneum, and pneumomediastinum (Figure 1).
Perforated sigmoid colon diverticulitis with pneumoperitoneum, pneumoretroperitoneum, and pneumomediastinum. The CT findings indicated that the case corresponded to Hinchey stage II and was most consistent with WSES stage 2B complicated diverticulitis.
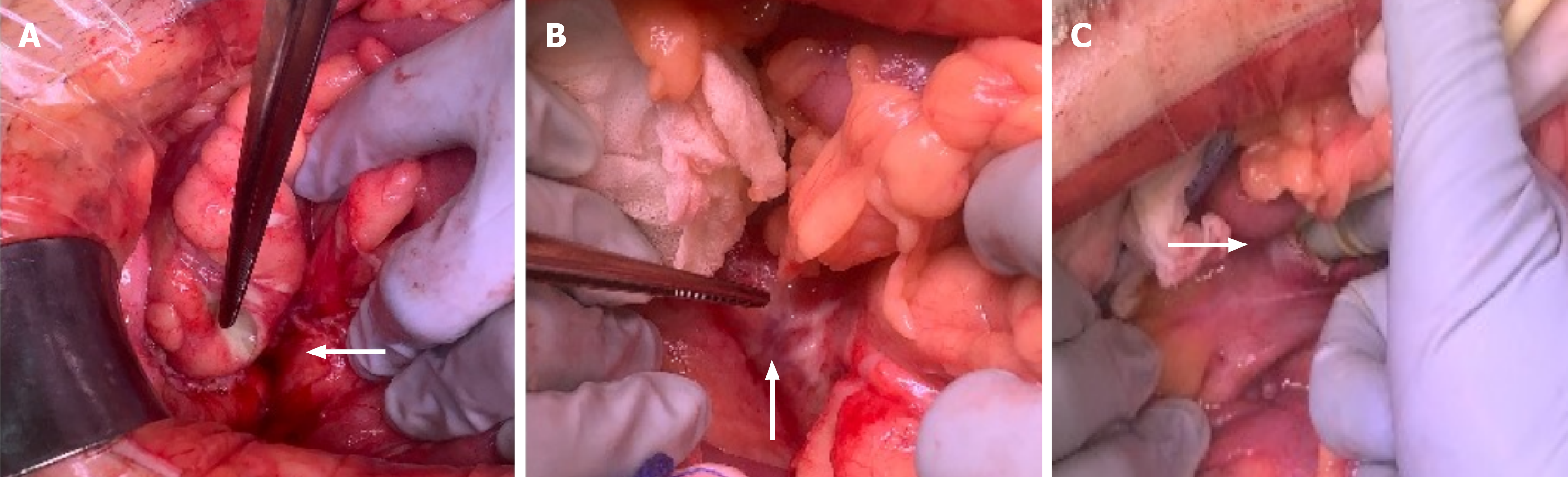
Because intra-abdominal infection caused by hollow organ perforation was suspected, an exploratory laparotomy was arranged immediately. During the procedure, the abdominal cavity was confirmed to be clean without contaminated ascites. However, mild necrosis and an unpleasant odor were identified in the mesocolon tissue near the sacral prom
As empirical therapy for sepsis, intravenous piperacillin-tazobactam (4.5 g every 8 hours) was administered for 2 weeks following the operation, along with fluid hydration. Following hospitalization in the intensive care unit for 5 days, the patient was transferred to a general ward. In the general ward, intermittent low-grade fever was observed, which was suspected to be an acute complication of chronic obstructive pulmonary disease. Abdominal CT on postoperative day 14 revealed no free air in the retroperitoneal space or mediastinum. The patient was discharged on postoperative day 40. His pathology report revealed acute peritonitis and subserosal necrosis, compatible with our intraoperative findings.
Pneumoretroperitoneum can result from perforation of the duodenum or posterior aspects of the ascending, descending, and sigmoid colon segments. Patients with pneumoretroperitoneum may present with no clinical signs, which delays their diagnosis and increases the risk of life-threatening complications[3]. Free air in the retroperitoneum may travel through anatomical fascial planes into the esophageal or aortic hiatus of the diaphragm and to the mediastinum[5,6]. The visceral space, as described by Maunder et al[5], is a soft tissue compartment with a fascial plane that connects cervical soft tissues with the mediastinum and retroperitoneum, allowing air leakage. Our patient presented with major em
Diagnosing perforated diverticulitis in patients with atypical symptoms can be challenging. Therefore, diagnosis can often be delayed, particularly in the absence of peritoneal signs and abdominal pain associated with intramesenteric perforation. Many patients in whom diagnosis are delayed have an autoimmune disease and are prescribed either a steroid or immunosuppressive agent, which typically masks the symptoms of diverticulitis perforation. Even if no peritoneal irritation is noted in the majority of cases, fever or unstable vital signs, such as hypotension or shortness of breath, are commonly observed. Our patient presented with no peritoneal signs and with stable vital signs. CT was arranged because of the high suspicion of infection. In stable patients, CT remains the gold standard for diagnosing diverticulitis because it enables visualization of findings such as colonic wall thickening, pericolic fat stranding, abscesses, free air, and perforation, and these findings directly inform disease classification in the WSES 2020 guidelines and can guide appropriate management[4]. In the detection of free air, CT has a success rate of approximately 85%[3,9]. In certain cases, free air may travel to other areas as a result of the pressure gradient, causing subcutaneous emphysema, pneumopericardium, or pneumothorax[6-8,10,11]. This phenomenon of free air travel may be attributed to the relatively long interval between symptom onset and the initiation of therapy, and it can be clearly observed on CT or radiography scans. Bormann et al[8] reported a rare case of a patient who presented with hoarseness due to subcutaneous emphysema caused by perforated diverticulitis. In summary, patients presenting with subcutaneous neck emphysema without a thoracic etiology must undergo further assessment for gastrointestinal sources.
Prompt surgical treatment is required when perforated diverticulitis is suspected. According to the 2020 update of the WSES guidelines, whether a case of acute colonic diverticulitis is of the uncomplicated or complicated form must be determined because the appropriate management strategies for these forms differ substantially. Uncomplicated diverticulitis can often be managed conservatively, whereas complicated diverticulitis includes conditions such as abscess, perforation, obstruction, and fistula formation, which usually require surgical or interventional treatment. Further subclassification of complicated diverticulitis into diverticulitis with vascular (e.g., bleeding, ischemia) or nonvascular (e.g., perforation, abscess, obstruction, fistula) complications may provide a more comprehensive framework for clinical evaluation and tailored management strategies[4]. In the reported cases, almost all patients underwent Hartmann’s procedure. After surgery, most of them survived, with only two deaths reported. Each patient was hospitalized for a duration depending on their disease severity and concurrent comorbidities[7-9]. Several randomized controlled trials have compared Hartmann’s procedure with resection accompanied by primary anastomosis with or without a diverting stoma in patients with Hinchey III-IV diverticulitis[12,13]. However, none of these trials mentioned diverticulitis perforation in the retroperitoneal space. In addition to resection of the diseased segment of the colon and performance of proximal diverting colostomy, opening of the retroperitoneal space for abscess drainage and irrigation is necessary. Notably, pneumoperitoneum and pneumomediastinum in this setting do not require specific intervention. Once the perforation source has been controlled surgically, free air in the peritoneum, retroperitoneum, and mediastinum is gradually reabsorbed. This explains why postoperative follow-up CT in our patient revealed spontaneous resolution of the free air. Patients with pneumoretroperitoneum and pneumomediastinum require tailored management strategies depending on the source of free air and their clinical state.
Pneumoretroperitoneum and pneumomediastinum are rare but serious complications of perforated diverticulitis. Their diagnosis may be delayed, particularly when the patient exhibits no peritoneal signs. Laboratory examinations and CT may be useful. Prompt surgical intervention, such as laparotomy, should be considered in cases of perforated diverticulitis.
| 1. | Bharucha AE, Parthasarathy G, Ditah I, Fletcher JG, Ewelukwa O, Pendlimari R, Yawn BP, Melton LJ, Schleck C, Zinsmeister AR. Temporal Trends in the Incidence and Natural History of Diverticulitis: A Population-Based Study. Am J Gastroenterol. 2015;110:1589-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 259] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 2. | Pavlidis ET, Pavlidis TE. Current Aspects on the Management of Perforated Acute Diverticulitis: A Narrative Review. Cureus. 2022;14:e28446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 3. | Onur MR, Akpinar E, Karaosmanoglu AD, Isayev C, Karcaaltincaba M. Diverticulitis: a comprehensive review with usual and unusual complications. Insights Imaging. 2017;8:19-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 4. | Sartelli M, Weber DG, Kluger Y, Ansaloni L, Coccolini F, Abu-Zidan F, Augustin G, Ben-Ishay O, Biffl WL, Bouliaris K, Catena R, Ceresoli M, Chiara O, Chiarugi M, Coimbra R, Cortese F, Cui Y, Damaskos D, De' Angelis GL, Delibegovic S, Demetrashvili Z, De Simone B, Di Marzo F, Di Saverio S, Duane TM, Faro MP, Fraga GP, Gkiokas G, Gomes CA, Hardcastle TC, Hecker A, Karamarkovic A, Kashuk J, Khokha V, Kirkpatrick AW, Kok KYY, Inaba K, Isik A, Labricciosa FM, Latifi R, Leppäniemi A, Litvin A, Mazuski JE, Maier RV, Marwah S, McFarlane M, Moore EE, Moore FA, Negoi I, Pagani L, Rasa K, Rubio-Perez I, Sakakushev B, Sato N, Sganga G, Siquini W, Tarasconi A, Tolonen M, Ulrych J, Zachariah SK, Catena F. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 224] [Cited by in RCA: 228] [Article Influence: 38.0] [Reference Citation Analysis (4)] |
| 5. | Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447-1453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 314] [Cited by in RCA: 317] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Welikumbura S, Pham T, Jain A, Williams M, Smart P. Approach to the patient with pneumoretroperitoneum. ANZ J Surg. 2021;91:206-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Muronoi T, Kidani A, Hira E, Takeda K, Kuramoto S, Oka K, Shimojo Y, Watanabe H. Mediastinal, retroperitoneal, and subcutaneous emphysema due to sigmoid colon penetration: A case report and literature review. Int J Surg Case Rep. 2019;55:213-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Bormann SL, Wood R, Guido JM. Hoarseness due to subcutaneous emphysema: a rare presentation of diverticular perforation. J Surg Case Rep. 2024;2024:rjad566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Hafiani H, Bouknani N, Choukri EM, Saibari RC, Rami A. Pneumoperitoneum, pneumoretroperitoneum and pneumomediastinum: rare complications of perforation peritonitis: a case report. J Med Case Rep. 2024;18:187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 10. | Kurti F, Cala V, Vyshka G. Pneumoretroperitoneum, pneumomediastinum, and neck emphysema due to rectal diverticulosis. Clin Case Rep. 2022;10:e6679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Luo RR, Fu-Shan J, Hsieh CC. Pneumoretroperitoneum, pneumoperitoneum, pneumomediastinum and pneumopericardium in an elderly woman with rupture of diverticulitis. Asian J Surg. 2023;46:2225-2226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Bridoux V, Regimbeau JM, Ouaissi M, Mathonnet M, Mauvais F, Houivet E, Schwarz L, Mege D, Sielezneff I, Sabbagh C, Tuech JJ. Hartmann's Procedure or Primary Anastomosis for Generalized Peritonitis due to Perforated Diverticulitis: A Prospective Multicenter Randomized Trial (DIVERTI). J Am Coll Surg. 2017;225:798-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 165] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 13. | Lambrichts DPV, Vennix S, Musters GD, Mulder IM, Swank HA, Hoofwijk AGM, Belgers EHJ, Stockmann HBAC, Eijsbouts QAJ, Gerhards MF, van Wagensveld BA, van Geloven AAW, Crolla RMPH, Nienhuijs SW, Govaert MJPM, di Saverio S, D'Hoore AJL, Consten ECJ, van Grevenstein WMU, Pierik REGJM, Kruyt PM, van der Hoeven JAB, Steup WH, Catena F, Konsten JLM, Vermeulen J, van Dieren S, Bemelman WA, Lange JF; LADIES trial collaborators. Hartmann's procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol. 2019;4:599-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 138] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/