Published online Nov 6, 2025. doi: 10.12998/wjcc.v13.i31.108301
Revised: May 25, 2025
Accepted: September 11, 2025
Published online: November 6, 2025
Processing time: 203 Days and 10.2 Hours
Papillary fibroelastomas are rare, benign cardiac tumors typically found on the heart valves. This case series presents three patients with aortic valve fibroe
The patients aged 72 years, 51 years, and 42 years underwent EUS for various indications when aortic valve lesions consistent with fibroelastomas were discovered. These findings were subsequently confirmed by transesophageal echocardiography in two cases, with the third patient awaiting assessment. The lesions ranged in size from 0.61 cm to 1.6 cm in diameter and exhibited characteristic sonographic features of fibroelastomas, including hyperechoic appearance and attachment to the aortic valve leaflets. These cases highlight the potential of EUS in identifying subtle cardiac lesions during gastrointestinal evaluation, raising questions about the true prevalence of fib
This case series raises important questions regarding the prevalence of aortic valve fibroelastoma lesions in the general population. This highlights the urgent need for comprehensive evidence-based guidelines to standardize the management and long-term surveillance of affected patients.
Core Tip: This case series presents three instances of aortic valve fibroelastoma detected during endoscopic ultrasound for pancreatic and biliary pathologies. These serendipitous findings highlight the potential of endoscopic ultrasound in identifying subtle cardiac lesions during gastrointestinal evaluations. These cases raise important questions regarding the true prevalence of fibroelastomas and highlight the need for established guidelines for their management and surveillance. This series emphasizes the importance of thorough assessments and multidisciplinary approaches in managing unexpected discoveries, while also highlighting the potential thromboembolic risks associated with fibroelastomas and the challenges in determining appropriate management strategies for asymptomatic patients.
- Citation: Elsayed G, Mohamed L, Almasaabi M, Barakat K, Taha R, AlQahtani MS, Makdisi G, Musa M, Alfadda A, Gadour E. Incidental detection of aortic valve fibroelastomas during endoscopic ultrasound for pancreatic evaluation: Three case reports. World J Clin Cases 2025; 13(31): 108301
- URL: https://www.wjgnet.com/2307-8960/full/v13/i31/108301.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i31.108301
Incidental findings are becoming increasingly common in modern medical imaging, presenting both diagnostic and management challenges for clinicians. Among these, cardiac tumors, although rare, are of particular concern because due of their potential for serious complications. Papillary fibroelastomas, the second most common benign cardiac tumors, exemplify this issue, with a reported prevalence of 0.02% to 0.45% in the general population[1,2]. Papillary fibroelastomas are typically small, benign tumors ranging from 2 mm to 70 mm in size, predominantly arising from the valvular surfaces, with the aortic and mitral valves being the most affected sites[3]. While many patients with fibroelastomas remain asymptomatic, up to half may experience severe complications, including neurological events, such as stroke and myocardial infarction[1-3]. The detection of these tumors is crucial for the prevention of potentially life-threatening outcomes. Traditionally, fibroelastomas have been difficult to detect using standard imaging techniques, often going unnoticed until they are discovered through invasive procedures such as transesophageal echocardiography (TOE) or during autopsy. However, recent advancements in echocardiographic technology and improved image resolution have increased the detection rate of fibroelastomas in living patients[4]. Despite these improvements, there is remains a need for more sensitive and less invasive diagnostic methods. Endoscopic ultrasound (EUS) has emerged as a versatile tool in medical imaging, primarily used for staging upper gastrointestinal malignancies and evaluating pancreato-biliary pathologies[5]. Its high-resolution imaging capabilities have led to the detection of various subtle lesions. However, the potential of EUS to identify cardiac tumors, particularly fibroelastomas, has not been extensively explored or reported in the literature. This case series addresses a critical gap in the literature by presenting three cases in which papillary fibroelastomas were incidentally detected during EUS examinations performed for pancreato-biliary indications. Although EUS is primarily used for gastrointestinal imaging, these cases raise the possibility that it may also be useful have utility in identifying subtle cardiac lesions, a role that remains largely unexplored. By examining these findings, we aim to assess the diagnostic value of EUS in this context and to consider its broader clinical implications for the early recognition and management of fibroelastomas.
Case 1: Epigastric pain, bloating, and nausea.
Case 2: Hemoptysis and pain in the left iliac fossa.
Case 3: Obstructive choledocholithiasis.
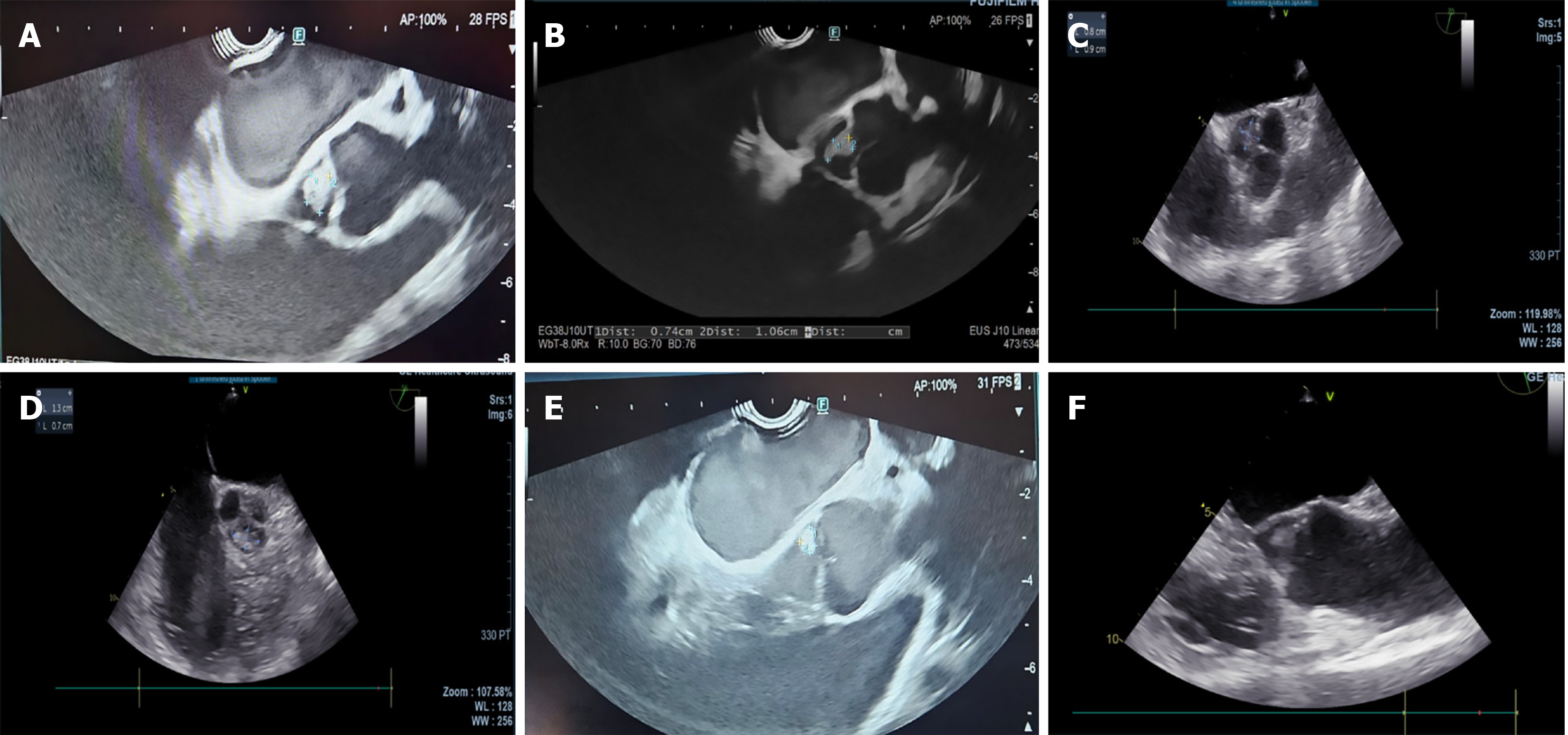
Case 1: 72-year-old female with recurrent bilateral breast cancer presented with epigastric pain, bloating, and nausea. Computed tomography (CT) revealed a suspicious lesion in the pancreatic head causing biliary and pancreatic duct obstruction. EUS and endoscopic retrograde cholangiopancreatography confirmed a poorly differentiated adenocarcinoma, staged as T3N0M0 or T2N0Mx. EUS also identified a 1 cm lesion on the non-coronary cusp of the aortic valve leaflet, suggestive of benign fibroelastoma (Figure 1A).
Case 2: 51-year-old female with Sjogren syndrome presented with hemoptysis and left iliac fossa pain. CT showed an enlarged pancreas. EUS revealed features consistent with autoimmune pancreatitis and a 1.6 cm aortic valve lesion (Figure 1B), suggestive of benign fibroelastoma, confirmed by TOE (Figure 1C).
Case 3: 42-year-old female diagnosed with obstructive choledocholithiasis underwent emergency endoscopic retrograde cholangiopancreatography in October 2024. Post-cholecystectomy complications led to infection of the gallbladder bed. EUS revealed a semi-organized collection and a 0.61 cm × 0.43 cm aortic valve lesion suggestive of fibroelastoma.
Case 1: Bilateral breast cancer diagnosed in 2000 year, treated with bilateral lumpectomy followed by bilateral mastectomy due to recurrence. Hormone receptor-negative tumor.
Case 2: Sjogren syndrome and history of latent tuberculosis treatment 16 years prior.
Case 3: No significant past medical history mentioned.
Case 1: No family history of a similar condition. Apart from previously treated breast cancer, no other clinical history.
Case 2: No family history of a similar condition. Patient is undergoing regular rheumatology follow-up for the Sjogren syndrome.
Case 3: No family history of a similar condition and no other past medical history.
Cases 1-3: Physical examination was unremarkable. Vital signs were all normal throughout.
Cases 1-3: The results of the laboratory examinations were non-significant, with all findings falling within the normal range for each of the three cases.
Case 1: An initial CT scan revealed a suspicious lesion in the pancreatic head, causing biliary and pancreatic duct obstructions. Staging CT confirmed a T3N0M0 pancreatic tumor. EUS staged the tumor as T2N0Mx and detected a 1 cm lesion on the non-coronary cusp of the aortic valve, suggestive of a fibroelastoma. TOE confirmed EUS findings of aortic valve lesions (Figure 1D).
Case 2: CT showed an enlarged pancreas with a normal pancreatic duct caliber and no evident soft tissue or cystic lesions. EUS revealed features consistent with autoimmune pancreatitis and incidentally identified a 1.6 cm aortic valve lesion suggestive of fibroelastoma. TOE confirmed features consistent with papillary fibroelastoma (Figure 1E).
Case 3: EUS was performed to evaluate post-cholecystectomy collection in the gallbladder bed. EUS identified a 0.61 cm × 0.43 cm lesion on the aortic valve, with characteristics suggestive of a fibroelastoma (Figure 1F).
Aortic valve fibroelastoma (1 cm lesion on the non-coronary cusp) on top of a poorly differentiated pancreatic adenocarcinoma (T2N0Mx).
Aortic valve fibroelastoma (1.6 cm lesion) and autoimmune pancreatitis.
Incidental suspected aortic valve fibroelastoma (0.61 cm × 0.43 cm lesion). Obstructing choledocholithiasis (resolved). Aortic valve fibroelastoma (0.61 cm × 0.43 cm lesion).
In all three cases, aortic valve fibroelastomas were discovered during EUS procedures for pancreatic/biliary issues. Fibroelastoma diagnoses were confirmed using TOE in all cases.
Cases 1-3: The patients were managed conservatively because of their asymptomatic presentation and tumor size. Long-term follow-up was implemented, although challenging, without established guidelines for monitoring fibroelastomas.
Cases 1-3: The patients were managed conservatively using a watch-and-wait approach because of their asymptomatic presentation and tumor size. Long-term follow-up without established guidelines for monitoring fibroelastomas remains challenging remains challenging without established guidelines for monitoring fibroelastomas. Multidisciplinary evaluation is crucial for determining the management (Table 1).
| Patient | Age | Indication for EUS | Valve lesion size | TOE confirmation | Management |
| Case 1 | 72 | Epigastric pain, bloating, nausea | 1.0 cm | Yes | Conservative (watch-and-wait) |
| Case 2 | 51 | Hemoptysis and left iliac fossa pain | 1.6 cm | Yes | Conservative (watch-and-wait) |
| Case 3 | 42 | Obstructive choledocholithiasis | 0.61 cm | Yes | Conservative (watch-and-wait) |
The incidental discovery of cardiac fibroelastomas during EUS examinations of the pancreas underscores an unanticipated capability of EUS, rather than its recommended application for detecting cardiac lesions. These case reports underscore the essential role of comprehensive EUS evaluations in identifying incidental pathologies, such as cardiac findings and aortic valve lesions, which add an intriguing dimension to the patient's clinical course. The visualization of the aortic valve region during EUS procedures is not standard practice, and these findings emerge from a unique interplay of physician expertise and patient-specific factors. This distinction is crucial to understanding the context of these discoveries. Primary cardiac neoplasms, also known as tumors, are rare, with an estimated prevalence of approximately 0.02%. About 75% of these tumors are benign. The most common types of primary cardiac tumors include papillary fibroelastomas, myxomas, hemangiomas, and lipomas, with fibroelastomas and myxomas being the most prevalent[6,7].
In the patients described herein, a meticulous EUS examination of the posterior mediastinum facilitated the diagnosis of these aortic lesions. In the absence of clinical indicators of infective endocarditis, the diagnosis of papillary fibroelastoma was confirmed and corroborated using TOE. Notably, these cases were diagnosed between September 2024 and January 2025, prompting inquiries regarding the actual prevalence of these lesions, which may be higher than that previously reported. The precise etiology of these tumors remains uncertain; however, the prevailing hypothesis suggests that they may originate from the aggregation of microthrombi at the coaptation margins of the heart valves. On echocardiography, these tumors appear pedunculated and mobile with a filamentous surface, typically exhibiting a speckled appearance characterized by echolucency and stippled patterns along their edges[8]. The echocardiographic descriptions of these lesions were closely aligned with the EUS findings, particularly their pedunculated and echolucent characteristics. Fibroelastomas can also be evaluated using cardiac magnetic resonance imaging to determine their precise size and assess other cardiac structures. However, data on potential complications related to fibroelastoma size are limited. Most of these tumors are indolent and exhibit benign behavior[3]. In the patients studied, the multidisciplinary team consensus was to adopt a watch-and-wait approach, considering the tumor size and absence of clinical symptoms.
Currently, there are no established guidelines for the management and surveillance of these tumors. However, the literature suggests that symptomatic fibroelastomas should be surgically excised. For asymptomatic cases, management decisions vary depending on factors such as tumor mobility, embolic risk, location, planned cardiac surgeries, and the patient’s overall performance status. Ultimately, tumor size and mobility were regarded as the most significant independent predictors of embolic events, regardless of whether the tumor was located on the left or right side of the heart[8]. Similar findings of incidental aortic valve fibroelastomas detected during EUS have not been widely reported in the literature, making these cases relatively unique. While visualization of the aortic valve during routine EUS is not standard practice, these cases suggest that it may be technically feasible in some instances, depending on factors such as patient anatomy and operator expertise. The findings of this case series should be interpreted in the light of several limitations. The small sample size of the three cases limits the generalizability to broader populations. The absence of histopathological confirmation introduces some uncertainty regarding the precise nature of the observed lesions. Additionally, the lack of long-term follow-up data constrains our understanding of the outcomes and optimal management approaches. These limitations underscore the need for larger and, more comprehensive studies to further elucidate the clinical implications of these observations.
These cases highlight the potential of EUS in identifying subtle cardiac lesions during gastrointestinal evaluation, raising questions about the true prevalence of fibroelastomas and the need for establishing management guidelines. A multidisciplinary approach, primarily involving consultations with cardiologists specializing in imaging, to meticulously evaluate the risks associated with surgical excision vs conservative management, is recommended. For this cohort of patients, determining the appropriate monitoring duration remains challenging owing to the lack of established guidelines.
| 1. | Adams HP Jr. Cerebrovascular manifestations of tumors of the heart. Handb Clin Neurol. 2021;177:275-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Amano J, Nakayama J, Yoshimura Y, Ikeda U. Clinical classification of cardiovascular tumors and tumor-like lesions, and its incidences. Gen Thorac Cardiovasc Surg. 2013;61:435-447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 70] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 3. | Devanabanda AR, Lee LS. Papillary Fibroelastoma. 2023 Apr 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. [PubMed] |
| 4. | Gegouskov V, Kadner A, Engelberger L, Carrel T, Tevaearai H. Papillary fibroelastoma of the heart. Heart Surg Forum. 2008;11:E333-E339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Prager M, Prager E, Sebesta C Jr, Sebesta C. Diagnostic and Therapeutic Indications for Endoscopic Ultrasound (EUS) in Patients with Pancreatic and Biliary Disease-Novel Interventional Procedures. Curr Oncol. 2022;29:6211-6225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 6. | Hajouli S, Belcher AM, Mitulescu L, Annie FH, Bafakih FF, Grigore AM, Alwair H. Pulmonic valve fibroelastoma-A rare incidental finding. Radiol Case Rep. 2024;19:1571-1574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 7. | Bouhzam N, Kurtz B, Doguet F, Eltchaninoff H, Bauer F. Incidental papillary fibroelastoma multimodal: imaging and surgical decisions in 2 patients. Tex Heart Inst J. 2012;39:731-735. [PubMed] |
| 8. | Lopes JL, Freitas A, Augusto JB. Fibroelastoma, an Incidentaloma Disease? - Image Cases of Fibroelastomas as Incidental Findings in Four Patients, Four Different Valves. Arq Bras Cardiol. 2024;121:e20230222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/