Published online Jan 26, 2025. doi: 10.12998/wjcc.v13.i3.94389
Revised: September 28, 2024
Accepted: October 21, 2024
Published online: January 26, 2025
Processing time: 238 Days and 16.5 Hours
In this editorial, we have commented on the article that has been published in the recent issue of World Journal of Clinical Cases. The authors have described a case of unilateral thyroid cyst and have opined that the acute onset of infection may be linked to diabetes mellitus (DM). We have focused on the role of nutrition in the association between DM and infection. Patients with DM are at a high risk of infection, which could also be attributed to nutrition-related factors. Nutritional interventions for patients with diabetes are mainly based on a low-calorie diet, which can be achieved by adhering to a low-carbohydrate diet. However, dietary fiber supplementation is recommended to maintain the diversity of the gut microbiota. Furthermore, high-quality protein can prevent the increased risk of infection due to malnutrition. Supplementation of vitamins C, vitamins A, vitamins D, and folic acid improves blood sugar control and facilitates immune regulation. Mineral deficiencies augment the risk of infection, but the relationship with diabetes is mostly U-shaped and a good intake should be maintained.
Core Tip: Nutrition plays a key role in diabetic infections. Reducing the burden of infection via nutrition is required not only from the perspective of treatment but also to reduce expenses. For patients with diabetes, maintaining nutrient balance can effectively reduce inflammation and oxidative stress, thereby alleviating the risk of infection.
- Citation: Yu XL, Zhou LY, Huang X, Li XY, Wang MK, Yang JS. Role of nutrition in diabetes mellitus and infections. World J Clin Cases 2025; 13(3): 94389
- URL: https://www.wjgnet.com/2307-8960/full/v13/i3/94389.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i3.94389
Diabetes mellitus (DM) is a metabolic disease characterized by high levels of blood sugar and has a significant impact on the lives and well-being of individuals, families, and societies worldwide. Patients with diabetes are at a higher risk of infections, including bacterial, viral, and fungal infections of the respiratory cracked, urethra, gastrointestinal tract, skin and soft tissues, head and neck, and other systemic infections, when compared to the general population[1]. Insulin deficiency and hyperglycemia cause deficiencies in host defenses, which render the immune system incapable of fighting against invading pathogens and increase the risk of infection. The suppression of cytokine production; defects in leukocyte recruitment and pathogen recognition; neutrophil, macrophage, and monocyte dysfunction are some of the challenging issues in this direction[2,3]. Furthermore, DM is a risk factor for nosocomial infections[4] that may alter the clinical course or severity of certain infections, leading to a poor prognosis, and thereby exacerbating the financial burden of patients[3,5-7]. Several studies during coronavirus disease 2019 (COVID-19) pandemic have revealed that patients with diabetes are more susceptible to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and that high blood sugar can worsen the symptoms and increase the mortality[8-10].
Hyperglycemia is caused by a defect in insulin secretion or impaired biological action. Infections can also result in hyperglycemia[11,12]. Reports have been published on new-onset DM after influenza and dengue infection[13,14]. The global prevalence of DM in people aged 20–79 years has increased from 9.3% (463 million) in 2019[15] to 10.5% (536.6 million) in 2021[16]. This increase can predominantly be attributed to the increase in obesity rates, which is also affected by the COVID-19 pandemic. The pancreas is one of the organs targeted by SARS-CoV-2, and reversible β cell damage and transient hyperglycemia occur after the infection, especially in patients with DM, who are prone to pancreatic damage and even acute pancreatitis[9,17-20]. The entry of the virus triggers the release of proinflammatory cytokines, which reduces angiotensin-converting enzyme 2 receptor levels and also leads to insulin resistance and inadequate insulin secretion[21].
In the recent issue of World Journal of Clinical Cases, Liu et al[22] published an interesting article entitled “Chronic infectious unilateral giant thyroid cyst related to DM: A case report”. This paper describes a special case of a unilateral giant benign thyroid cyst with chronic infection. Infections are intricately linked to DM but usually occur in the setting of extreme metabolic disorders[23]. The patient had a 40-year history of slow-progressing thyroid nodules and a 7-year history of DM with good glycemic control. The authors have reasoned that DM leads to a decrease in systemic and local immunity, thereby affecting the progression of thyroid nodules and the onset of autoinfection. Several complex factors have influenced the progression of the disease in this patient. The patient also had mild iron (Fe) deficiency anemia and hypoproteinemia at the time of admission, which could be ascribed to the nutrient depletion resulting from recurrent chronic infections caused by the thyroid cyst. Malnutrition increases the likelihood of acute attacks of infection, which prompts us to contemplate the role of nutrition in infections in patients with diabetes.
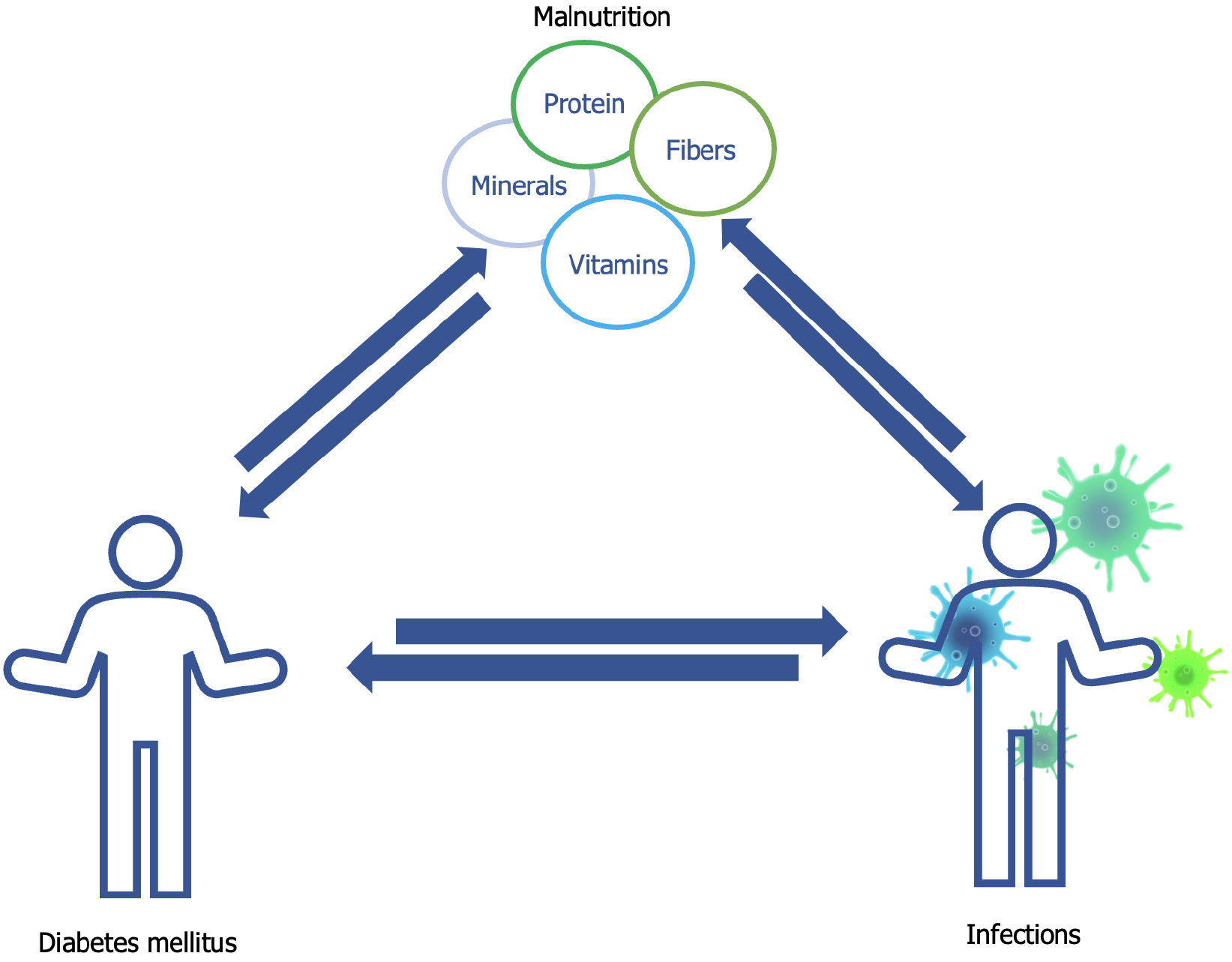
Strategies to manage DM usually include strict medications, regular exercise, and a healthy diet. Of these, nutritional intervention generally necessitates controlling the calories in the diet, consuming low-glycemic index foods, and increasing the fiber content. Good nutritional status is an important basis for a healthy immune system and the prevention of infections. DM itself alters the body’s nutritional status, resulting in micronutrient and antioxidant deficiencies[24] (Figure 1). Malnutrition can lead to a decrease in the number of immune cells, thereby affecting viral replication and pathogenicity, increasing the susceptibility to infections, and making infections more severe and even fatal[25]. Prevention, diagnosis, and treatment of malnutrition and evidence-based nutritional therapy based on reasonable and indexed nutritional evaluation should be recommended in the management of infectious patients[26]. Several studies have focused on the correlation between inflammatory markers and DM and its complications and have observed that inflammation may be both the cause and the effect of DM and its resultant complications. Inflammatory markers are therefore a potential therapeutic target[27,28]. Therefore, more attention needs to be paid to the association among nutrition, inflammation, and oxidative stress in patients with diabetes.
Whether for the general population or patients with type 2 DM (T2DM), total fat should contribute < 30%–35%, carbohydrates should contribute 45%–55%, and protein should contribute the remaining 15%–20% of the total energy intake[29]. Weight control is important in DM. Low-fat diets are preferred for weight management owing to the high energy density of fat. Low-carbohydrate diets have also become popular in recent years. A recent study has shown that consuming a diet low in energy to control weight in patients with T2DM did not rely on any specific macronutrients[30].
Low-carbohydrate diets have been definitively supported by the American Dietetic Association’s dietary guidelines for patients with diabetes in 2019[31]. Carbohydrate selection should consider the type (starch, sugar, or fiber), degree of processing (whole grains vs refined grains), glycemic response (glycemic index and load), and food structure (solid or liquid form) after consumption, all of which exert varying health effects[23]. For example, highly processed whole grain products and products made from finely ground whole grains have limited adaptability to stable blood glucose trajectories as they may cause rapid postprandial blood sugar spikes. Dietary fibers, which are the main source of energy for gut bacteria, can considerably affect the diversity of gut microbiota[32]. A diet high in fat and low in fiber may lead to the loss of beneficial and protective microorganisms, thereby promoting dysbiosis of the gut microbiota and leading to insulin resistance and a hyperglycemic state[32]. Dietary fiber exerts anti-inflammatory effects via the fermentation of the gut microbiota and the subsequent formation of metabolic compounds. These may be important in the overall homeostasis of inflammation and oxidative stress before and/or during acute infection[33].
Dietary proteins are the key modulators of glucose metabolism. Of the patients in long-term care facilities, 25%–85% exhibit protein undernutrition, which can lead to impaired immunity[34]. The risk of infection is higher in economically deprived areas which has reported incidences of protein malnutrition[33]. Total and animal protein intake have been reported to be positively correlated with the risk of T2DM[35]. Recent prospective cohort studies have documented that isocaloric substitution of animal protein with plant protein can reduce the risk of T2DM and that the beneficial association is mainly mediated by obesity-related inflammation[36]. The pro-inflammatory properties of proteins from animal sources and the anti-inflammatory features of those from plants have been recognized[33]. Amino acids regulate metabolism and immune function, such as glutamine, which is required for the expression of several genes in the immune system[33]. An adequate supply of essential amino acids and synthesizable amino acids (the so-called nutritional non-essential amino acids) can thus improve insulin sensitivity[34].
Evidence supports that the substitution of saturated fatty acids with monounsaturated or polyunsaturated fatty acids has a protective effect on the prevention of coronary heart diseases[37]. Foods rich in long-chain omega-3 fatty acids, such as oily fish, nuts, and seeds, are preferred for the prevention and treatment of cardiovascular diseases[38]. Moreover, fat quality may affect insulin sensitivity and accentuate the risk of T2DM[37]. Fatty acids can significantly alter the immune response, including changing the cellular lipid organization and interactions with nuclear receptors[33]. In addition, trans fatty acid intake, especially from processed foods such as fries and potato chips, is thought to have pro-inflammatory effects. However, naturally occurring trans fatty acids, such as those found in dairy products and beef, have been linked to a reduced risk of DM [33,38].
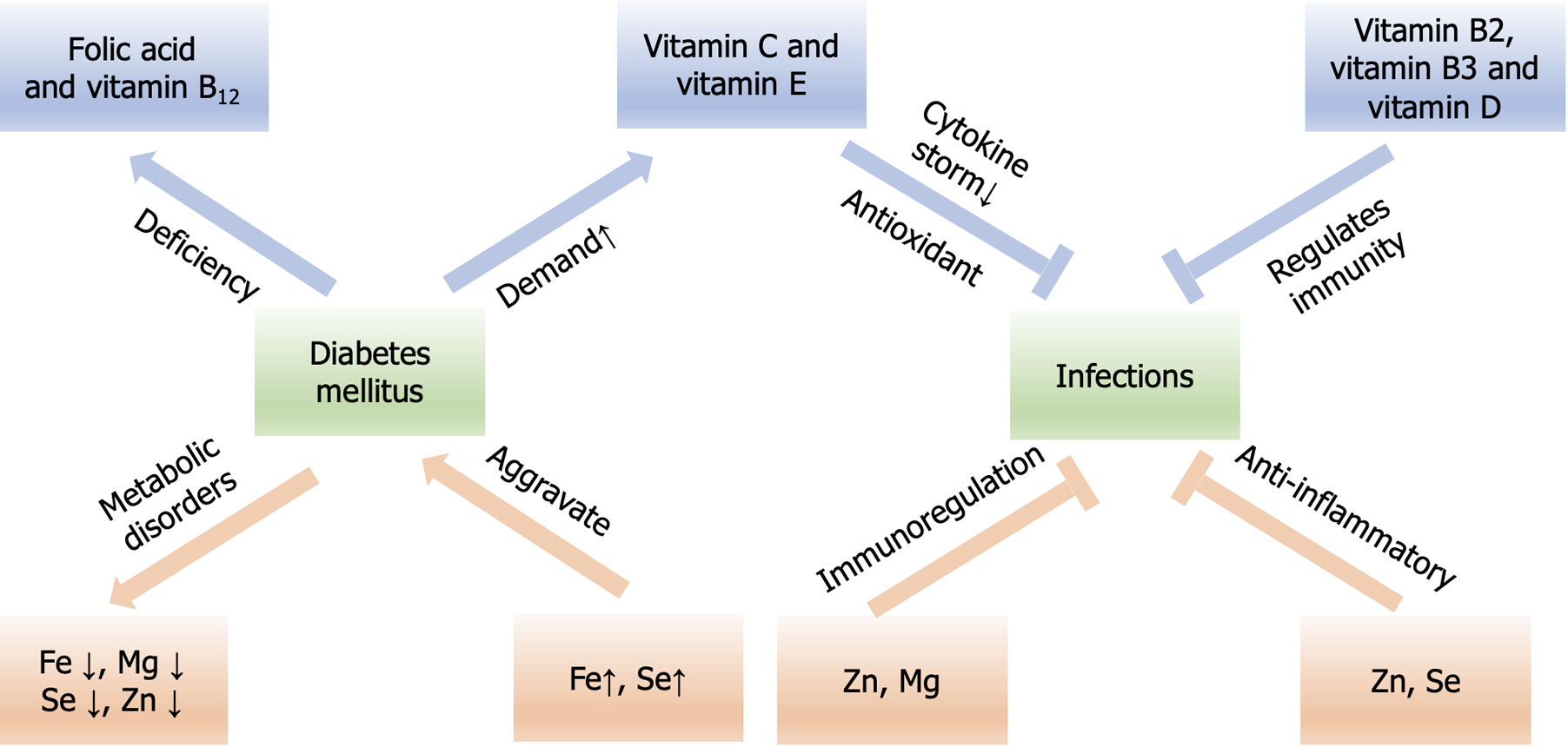
DM induces oxidative stress, and antioxidant supplementation can alleviate the resulting damage (e.g., coronary artery and cardiovascular diseases, retinopathy, and nephropathy) (Figure 2). A meta-analysis of interventional studies has demonstrated that vitamin C supplementation can improve glycemic control in patients with T2DM[39]. Although the efficacy of vitamin C in the treatment of patients with respiratory tract infections and critical illness remains controversial, its role as an antioxidant and a cofactor in various biosynthetic pathways related to immune regulation during infection is unquestionable[40]. Adequate dietary intake of vitamin C can aid in the prevention and treatment of respiratory and systemic infections[41]. Both vitamin C and folic acid can maintain the integrity of the immune barrier and support the functions of various immune cells, including phagocytes, natural killer cells, T cells, and B cells. This beneficial function has been recognized by the European Food Safety Authority[42]. Patients with diabetes on prolonged use of metformin face folate and vitamin B12 deficiencies, which results in hyperhomocysteinemia[43]. Most of the B vitamins, such as B1, B6, and B12, are associated with the development of T2DM and its complications[43]. Vitamin B deficiency substantially impairs cellular and immune system functions and induces inflammation due to hyperhomocysteinemia[44].
Vitamin A is considered an anti-inflammatory vitamin and plays a pertinent role in maintaining both innate and acquired immunity, promoting clearance of primary infections, and reducing the risk of secondary infections[45]. Vitamin A is vital for maintaining the morphology of the epithelium and is involved in its keratinization, stratification, differentiation, and functional maturation, which constitutes the first line of resistance to pathogens[33]. Being one of the world’s most serious micronutrient deficiencies, people with DM should maintain adequate vitamin A intake and concentration reserves. This precaution is necessary despite the lack of direct clinical evidence linking vitamin A to enhanced resistance to infection, especially in countries with low protein and meat intake[33,43]. Several studies have established an association between vitamin D deficiency and diabetes, which may be linked to the role of this vitamin in maintaining β cell function of the pancreas, regulating the insulin resistance pathway, and alleviating systemic inflammation[43]. Vitamin D supplementation has a potentially positive effect in improving the prognosis of infection, possibly because 25-hydroxyvitamin D stimulates the production of protective peptides in response to any viral or bacterial infection. The vitamin D receptor is expressed on several immune cells, and calcitriol, its activated form, can decrease proinflammatory cytokines and increase anti-inflammatory cytokines[46]. A meta-analysis of 25 randomized controlled trials involving 11321 participants indicated that vitamin D supplementation significantly reduced the risk of acute respiratory infections by 12% in the overall population[47]. Furthermore, vitamin E has been shown to possess antioxidant and anti-inflammatory activities and act as an immunomodulator to reduce the risk of infection. However, studies on the prevention or control of DM have yielded conflicting results[48,49]. Investigations have confirmed the protective effect of vitamin C and vitamin E against DM when used in combination. Nonetheless, the integration of vitamin E alone may not be sufficient to restore the physiological redox balance, probably because the body’s antioxidant system involves multiple interrelated components[49].
The relationship between minerals, such as Fe, zinc (Zn), and selenium (Se), and DM is U-shaped, and potential damage can occur in case of inadequate or excessive intake[24]. In addition, minerals play a potential role in fighting infections (Figure 2). Diabetes affects Zn homeostasis, and studies have confirmed that patients with diabetes have significantly lower levels of Zn in their whole blood[50]. This mineral is involved in insulin synthesis and signal transduction[51], and its deficiency exacerbates insulin resistance by inhibiting the Akt-mediated glucose metabolism pathway, leading to the loss of insulin sensitivity[52]. According to the 2015 China Nutrition Transformation Cohort Survey, 31% of Chinese adults are at a high risk of Zn deficiency owing to inadequate intake of the mineral[53]. Long-term low-dose Zn supplementation can significantly improve metabolic parameters in patients with T2DM[54]. Zn participates in immune function by acting as an anti-inflammatory agent and a signaling molecule in the immune system and protecting the tissue barrier from viral entry[55]. Zn deficiency increases the susceptibility to various infections, but consuming too much Zn can also weaken the local immune response and augment the susceptibility to infections[56].
Fe is a strong prooxidant that exacerbates the risk of T2DM by elevating the levels of oxidative stress, leading to decreased insulin secretion, insulin resistance, and increased gluconeogenesis in the liver[57]. A Chinese Health and Nutrition Survey cohort study reported that Fe excess (high serum ferritin and transferrin saturation) indirectly induces insulin resistance via liver injury and abnormal lipid metabolism[58]. A bidirectional relationship has been observed between Fe metabolism and glucose homeostasis. In a survey of 820 patients with diabetes with long-term follow-up, nearly 23% had unidentified anemia, which was 2–3 times higher than those with impaired kidney function[59]. Fe is an essential trace metal for almost all infectious microorganisms and exhibits a U-shaped relationship with infection. The overload of this mineral can result in increased susceptibility to infections, such as severe infections with siderophilic bacteria (e.g., Vibrio vulnificus and Yersinia enterocolitis)[60]. Patients with chronic infectious or inflammatory diseases typically develop normocytic anemia with characteristic hypoferremia[60]. In a cohort study involving 61852 individuals who were followed up for 15 years, an increased risk of bloodstream infections was observed in patients with low Fe status[61].
Se, a structural component of glutathione peroxidase, exerts an antioxidant effect. The link between Se levels and the risk of diabetes is difficult to determine, and both low and high levels of the mineral in the plasma appear to have adverse effects[38]. Decreased glutathione peroxidase activity has been noted in patients with diabetes, which could possibly be attributed to decreased Se levels[55]. In hospitalized patients with COVID-19, the association between Se and the immune system was further confirmed by its inhibition of the enzyme disulfide isomerase, which prevents viral entry into the cells[62].
Magnesium plays a role in the cellular activity of insulin. Hypomagnesemia is a common feature in patients with diabetes. The deficiency of this mineral inhibits cellular defenses against oxidative damage, exacerbates insulin resistance, and accelerates the development of diabetes-related complications[55]. Furthermore, this deficiency increases oxidative stress and cytokine storms, exacerbating the course of the infection[46].
Patients with diabetes require personalized nutrition counseling by professionals for long-term weight management. While consuming either a low-fat or low-carbohydrate diet, it is important to be mindful of high-quality protein intake to prevent malnutrition as it can increase the susceptibility to infections. Vitamins, especially those with antioxidant and anti-inflammatory effects, are beneficial for patients with diabetes, and minerals should also be maintained at appropriate levels. Maintaining a balance of these nutrients can help alleviate inflammation and oxidative stress, thereby streng
| 1. | Casqueiro J, Casqueiro J, Alves C. Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab. 2012;16 Suppl 1:S27-S36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 377] [Cited by in RCA: 539] [Article Influence: 38.5] [Reference Citation Analysis (0)] |
| 2. | Berbudi A, Rahmadika N, Tjahjadi AI, Ruslami R. Type 2 Diabetes and its Impact on the Immune System. Curr Diabetes Rev. 2020;16:442-449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 241] [Cited by in RCA: 593] [Article Influence: 98.8] [Reference Citation Analysis (0)] |
| 3. | Gupta S, Koirala J, Khardori R, Khardori N. Infections in diabetes mellitus and hyperglycemia. Infect Dis Clin North Am. 2007;21:617-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 104] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Yu XL, Zhou LY, Huang X, Li XY, Pan QQ, Wang MK, Yang JS. Urgent call for attention to diabetes-associated hospital infections. World J Diabetes. 2024;15:1683-1691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (4)] |
| 5. | Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of Infection in Type 1 and Type 2 Diabetes Compared With the General Population: A Matched Cohort Study. Diabetes Care. 2018;41:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 444] [Article Influence: 55.5] [Reference Citation Analysis (0)] |
| 6. | Jia Q, Zhao X, Wang C, Wang Y, Yan Y, Li H, Zhong L, Liu L, Zheng H, Zhou Y, Wang Y. Diabetes and poor outcomes within 6 months after acute ischemic stroke: the China National Stroke Registry. Stroke. 2011;42:2758-2762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 118] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Nitzan O, Elias M, Chazan B, Saliba W. Urinary tract infections in patients with type 2 diabetes mellitus: review of prevalence, diagnosis, and management. Diabetes Metab Syndr Obes. 2015;8:129-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 8. | Han D, Peng C, Meng R, Yao J, Zhou Q, Xiao Y, Ma H. Estimating the release of inflammatory factors and use of glucocorticoid therapy for COVID-19 patients with comorbidities. Aging (Albany NY). 2020;12:22413-22424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 9. | Liu JW, Huang X, Wang MK, Yang JS. Diabetes and susceptibility to COVID-19: Risk factors and preventive and therapeutic strategies. World J Diabetes. 2024;15:1663-1671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (5)] |
| 10. | Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, Khare S, Srivastava A. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr. 2020;14:535-545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 401] [Cited by in RCA: 465] [Article Influence: 77.5] [Reference Citation Analysis (0)] |
| 11. | Riyaten P, Salvadori N, Traisathit P, Ngo-Giang-Huong N, Cressey TR, Leenasirimakul P, Techapornroong M, Bowonwatanuwong C, Kantipong P, Nilmanat A, Yutthakasemsunt N, Chutanunta A, Thongpaen S, Klinbuayaem V, Decker L, Le Cœur S, Lallemant M, Capeau J, Mary JY, Jourdain G. New-Onset Diabetes and Antiretroviral Treatments in HIV-Infected Adults in Thailand. J Acquir Immune Defic Syndr. 2015;69:453-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Palepu S, Prasad GV. New-onset diabetes mellitus after kidney transplantation: Current status and future directions. World J Diabetes. 2015;6:445-455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 76] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 13. | Krishna SV, Sunil K, Prasad RD, Modi KD. Precipitation of new onset diabetes by H1N1 infection. Indian J Endocrinol Metab. 2012;16:S438-S440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Sudulagunta SR, Sodalagunta MB, Kumbhat M, Bangalore Raja SK. New Onset Diabetes Mellitus in Dengue Shock Syndrome. J Assoc Physicians India. 2018;66:104. [PubMed] |
| 15. | Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract. 2019;157:107843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5345] [Cited by in RCA: 6401] [Article Influence: 914.4] [Reference Citation Analysis (12)] |
| 16. | Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, Stein C, Basit A, Chan JCN, Mbanya JC, Pavkov ME, Ramachandaran A, Wild SH, James S, Herman WH, Zhang P, Bommer C, Kuo S, Boyko EJ, Magliano DJ. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3033] [Cited by in RCA: 5797] [Article Influence: 1449.3] [Reference Citation Analysis (37)] |
| 17. | Hariharan R, Odjidja EN, Scott D, Shivappa N, Hébert JR, Hodge A, de Courten B. The dietary inflammatory index, obesity, type 2 diabetes, and cardiovascular risk factors and diseases. Obes Rev. 2022;23:e13349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 243] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 18. | Boddu SK, Aurangabadkar G, Kuchay MS. New onset diabetes, type 1 diabetes and COVID-19. Diabetes Metab Syndr. 2020;14:2211-2217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 125] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 19. | Khunti K, Del Prato S, Mathieu C, Kahn SE, Gabbay RA, Buse JB. COVID-19, Hyperglycemia, and New-Onset Diabetes. Diabetes Care. 2021;44:2645-2655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 195] [Article Influence: 39.0] [Reference Citation Analysis (0)] |
| 20. | Wang MK, Yue HY, Cai J, Zhai YJ, Peng JH, Hui JF, Hou DY, Li WP, Yang JS. COVID-19 and the digestive system: A comprehensive review. World J Clin Cases. 2021;9:3796-3813. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (3)] |
| 21. | Yonekawa A, Shimono N. Clinical Significance of COVID-19 and Diabetes: In the Pandemic Situation of SARS-CoV-2 Variants including Omicron (B.1.1.529). Biology (Basel). 2022;11:400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Liu JB, Zhang SL, Jiang WL, Sun HK, Yang HC. Chronic infectious unilateral giant thyroid cyst related to diabetes mellitus: A case report. World J Clin Cases. 2024;12:1497-1503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (6)] |
| 23. | Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007;23:3-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 357] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 24. | Abiri B, Guest PC, Vafa M. Experience in Nutrition Management of Diabetes-Affected COVID-19 Patients. Adv Exp Med Biol. 2021;1321:69-80. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Silverio R, Gonçalves DC, Andrade MF, Seelaender M. Coronavirus Disease 2019 (COVID-19) and Nutritional Status: The Missing Link? Adv Nutr. 2021;12:682-692. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 26. | Wang MK, Yu XL, Zhou LY, Si HM, Hui JF, Hou DY, Li WP, Yang JS. COVID-19 and liver dysfunction: What nutritionists need to know. World J Gastroenterol. 2022;28:1526-1535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 27. | Aulich J, Cho YH, Januszewski AS, Craig ME, Selvadurai H, Wiegand S, Jenkins AJ, Donaghue KC. Associations between circulating inflammatory markers, diabetes type and complications in youth. Pediatr Diabetes. 2019;20:1118-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 28. | Duncan BB, Schmidt MI, Pankow JS, Ballantyne CM, Couper D, Vigo A, Hoogeveen R, Folsom AR, Heiss G; Atherosclerosis Risk in Communities Study. Low-grade systemic inflammation and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes. 2003;52:1799-1805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 796] [Cited by in RCA: 788] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 29. | Forouhi NG. Embracing complexity: making sense of diet, nutrition, obesity and type 2 diabetes. Diabetologia. 2023;66:786-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 30. | Churuangsuk C, Hall J, Reynolds A, Griffin SJ, Combet E, Lean MEJ. Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission. Diabetologia. 2022;65:14-36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 117] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 31. | Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, Mitri J, Pereira RF, Rawlings K, Robinson S, Saslow L, Uelmen S, Urbanski PB, Yancy WS Jr. Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report. Diabetes Care. 2019;42:731-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 708] [Cited by in RCA: 847] [Article Influence: 121.0] [Reference Citation Analysis (0)] |
| 32. | Ojo O. Recent Advances in Nutrition and Diabetes. Nutrients. 2021;13:1573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 33. | Iddir M, Brito A, Dingeo G, Fernandez Del Campo SS, Samouda H, La Frano MR, Bohn T. Strengthening the Immune System and Reducing Inflammation and Oxidative Stress through Diet and Nutrition: Considerations during the COVID-19 Crisis. Nutrients. 2020;12:1562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 485] [Cited by in RCA: 475] [Article Influence: 79.2] [Reference Citation Analysis (0)] |
| 34. | Wu G. Dietary protein intake and human health. Food Funct. 2016;7:1251-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 348] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 35. | Malik VS, Li Y, Tobias DK, Pan A, Hu FB. Dietary Protein Intake and Risk of Type 2 Diabetes in US Men and Women. Am J Epidemiol. 2016;183:715-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 177] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 36. | Li J, Glenn AJ, Yang Q, Ding D, Zheng L, Bao W, Beasley J, LeBlanc E, Lo K, Manson JE, Philips L, Tinker L, Liu S. Dietary Protein Sources, Mediating Biomarkers, and Incidence of Type 2 Diabetes: Findings From the Women's Health Initiative and the UK Biobank. Diabetes Care. 2022;45:1742-1753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 37. | Telle-Hansen VH, Gaundal L, Myhrstad MCW. Polyunsaturated Fatty Acids and Glycemic Control in Type 2 Diabetes. Nutrients. 2019;11:1067. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 38. | Klammer C, Schindler K, Bugl R, Plazek D, Vötter M, Kirchner T, Martino C, Klammer-Martin J, Brix J, Dämon S, Hoppichler F, Kautzky-Willer A, Kruschitz R, Toplak H, Clodi M, Ludvik B. [Nutrition for diabetic patients (Update 2023)]. Wien Klin Wochenschr. 2023;135:62-77. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 39. | Ashor AW, Werner AD, Lara J, Willis ND, Mathers JC, Siervo M. Effects of vitamin C supplementation on glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr. 2017;71:1371-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 40. | Milani GP, Macchi M, Guz-Mark A. Vitamin C in the Treatment of COVID-19. Nutrients. 2021;13:1172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 41. | Carr AC, Maggini S. Vitamin C and Immune Function. Nutrients. 2017;9:1211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 662] [Cited by in RCA: 1071] [Article Influence: 119.0] [Reference Citation Analysis (0)] |
| 42. | Miles EA, Calder PC. Effects of Citrus Fruit Juices and Their Bioactive Components on Inflammation and Immunity: A Narrative Review. Front Immunol. 2021;12:712608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 110] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 43. | Valdés-Ramos R, Guadarrama-López AL, Martínez-Carrillo BE, Benítez-Arciniega AD. Vitamins and type 2 diabetes mellitus. Endocr Metab Immune Disord Drug Targets. 2015;15:54-63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 112] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 44. | Shakoor H, Feehan J, Mikkelsen K, Al Dhaheri AS, Ali HI, Platat C, Ismail LC, Stojanovska L, Apostolopoulos V. Be well: A potential role for vitamin B in COVID-19. Maturitas. 2021;144:108-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 89] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 45. | Huang Z, Liu Y, Qi G, Brand D, Zheng SG. Role of Vitamin A in the Immune System. J Clin Med. 2018;7:258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 306] [Cited by in RCA: 319] [Article Influence: 39.9] [Reference Citation Analysis (0)] |
| 46. | DiNicolantonio JJ, O'Keefe JH. Magnesium and Vitamin D Deficiency as a Potential Cause of Immune Dysfunction, Cytokine Storm and Disseminated Intravascular Coagulation in covid-19 patients. Mo Med. 2021;118:68-73. [PubMed] |
| 47. | Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Griffiths CJ, Janssens W, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S Jr, Stelmach I, Kumar GT, Urashima M, Camargo CA Jr. Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. BMJ. 2017;356:i6583. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1094] [Cited by in RCA: 1243] [Article Influence: 138.1] [Reference Citation Analysis (0)] |
| 48. | Shakoor H, Feehan J, Al Dhaheri AS, Ali HI, Platat C, Ismail LC, Apostolopoulos V, Stojanovska L. Immune-boosting role of vitamins D, C, E, zinc, selenium and omega-3 fatty acids: Could they help against COVID-19? Maturitas. 2021;143:1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 49. | Ciarcià G, Bianchi S, Tomasello B, Acquaviva R, Malfa GA, Naletova I, La Mantia A, Di Giacomo C. Vitamin E and Non-Communicable Diseases: A Review. Biomedicines. 2022;10:2473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 27] [Reference Citation Analysis (0)] |
| 50. | Zhao XH, Zhang ZH. Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020;53:102353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 216] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 51. | Zhao T, Huang Q, Su Y, Sun W, Huang Q, Wei W. Zinc and its regulators in pancreas. Inflammopharmacology. 2019;27:453-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 52. | Cruz KJC, de Oliveira ARS, Morais JBS, Severo JS, Mendes PMV, de Sousa Melo SR, de Sousa GS, Marreiro DDN. Zinc and Insulin Resistance: Biochemical and Molecular Aspects. Biol Trace Elem Res. 2018;186:407-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 53. | Wang Y, Jia XF, Zhang B, Wang ZH, Zhang JG, Huang FF, Su C, Ouyang YF, Zhao J, Du WW, Li L, Jiang HR, Zhang J, Wang HJ. Dietary Zinc Intake and Its Association with Metabolic Syndrome Indicators among Chinese Adults: An Analysis of the China Nutritional Transition Cohort Survey 2015. Nutrients. 2018;10:572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 54. | Skalny AV, Aschner M, Tinkov AA. Zinc. Adv Food Nutr Res. 2021;96:251-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 55. | Dubey P, Thakur V, Chattopadhyay M. Role of Minerals and Trace Elements in Diabetes and Insulin Resistance. Nutrients. 2020;12:1864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 218] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 56. | Giovane RA, Di Giovanni-Kinsley S, Keeton E. Micronutrients for potential therapeutic use against COVID-19; a review. Clin Nutr ESPEN. 2021;46:9-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 57. | Harrison AV, Lorenzo FR, McClain DA. Iron and the Pathophysiology of Diabetes. Annu Rev Physiol. 2023;85:339-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 96] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 58. | Gao H, Yang J, Pan W, Yang M. Iron Overload and the Risk of Diabetes in the General Population: Results of the Chinese Health and Nutrition Survey Cohort Study. Diabetes Metab J. 2022;46:307-318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 59. | Thomas MC, MacIsaac RJ, Tsalamandris C, Power D, Jerums G. Unrecognized anemia in patients with diabetes: a cross-sectional survey. Diabetes Care. 2003;26:1164-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 226] [Cited by in RCA: 239] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 60. | Ganz T. Iron and infection. Int J Hematol. 2018;107:7-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 196] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 61. | Mohus RM, Paulsen J, Gustad L, Askim Å, Mehl A, DeWan AT, Afset JE, Åsvold BO, Solligård E, Damås JK. Association of iron status with the risk of bloodstream infections: results from the prospective population-based HUNT Study in Norway. Intensive Care Med. 2018;44:1276-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 62. | Detopoulou P, Demopoulos CA, Antonopoulou S. Micronutrients, Phytochemicals and Mediterranean Diet: A Potential Protective Role against COVID-19 through Modulation of PAF Actions and Metabolism. Nutrients. 2021;13:462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/