Published online Sep 16, 2025. doi: 10.12998/wjcc.v13.i26.107748
Revised: May 4, 2025
Accepted: June 13, 2025
Published online: September 16, 2025
Processing time: 117 Days and 3.8 Hours
Pericarditis is the inflammation of the pericardial sac due to a variety of stimuli that ultimately trigger a stereotyped immune response. This condition accounts for up to 5% of emergency department visits for nonischemic chest pain in Western Europe and North America. The most common symptoms of clinical presentation are chest pain and shortness of breath with associated unique electrocardiographic changes. Acute pericarditis is generally self-limited. How
We present the case of a 62-year-old woman who sought medical attention at the emergency department (ED) due to a 5-day history of chest pain, shortness of breath, and subjective fevers. Laboratory findings in the ED were significant for leukocytosis and elevated erythrocyte sedimentation rate and C-reactive protein. A chest X-ray revealed a new focal density within the left lower lung base, and a bedside point-of-care ultrasound showed a pericardial fluid collection. The pa
This case report emphasizes a unique complication of community-acquired pneumonia. Purulent pericarditis due to streptococcus pneumonia occurs via intrathoracic spread of the organism to the pericardium. This condition is virtually fatal without the administration of antibiotics. Therefore, in the context of suspected pneumonia and a new pericardial fluid collection on imaging, clinicians should suspect purulent pericarditis until proven otherwise, which requires emergent intervention.
Core Tip: Purulent pericarditis is a rare, life-threatening localized infection of the pericardial space that is fatal if left untreated. It is most commonly caused by staphylococcus aureus and streptococcus pneumoniae species. Purulent pericarditis, particularly from community-acquired pneumonia, is a rare occurrence. Diagnosis is commonly obtained via an echocardiogram, and treatment includes pericardiocentesis and antibiotic therapy. This article presents a rare case of purulent pericarditis due to community-acquired pneumonia that was successfully treated.
- Citation: English K, Pick N, Schmitz A. Acute purulent pericarditis secondary to community-acquired streptococcus pneumonia: A case report. World J Clin Cases 2025; 13(26): 107748
- URL: https://www.wjgnet.com/2307-8960/full/v13/i26/107748.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i26.107748
Pericarditis involves the inflammation of the pericardiac sac surrounding the heart[1]. This condition can be classified as chronic, subacute, and acute, with recurrence occurring in up to 30% of cases[1,2]. It can be complicated by other peri
Chest pain, shortness of breath, and subjective fevers.
A 62-year-old female presented to the emergency department (ED) due to a 5-day history of pleuritic chest pain, shortness of breathing, subjective fevers, and weakness. She called her pulmonologist to report these symptoms, who subsequently recommended she visit the ED. Upon arrival at the ED, she was afebrile, tachycardic (122/min), and hypotensive (88/45 mmHg). All other vital signs, such as respiration and oxygen saturation, were within normal limits.
Her medical history included Hodgkin’s lymphoma, radiation-induced lung fibrosis, aortic stenosis, acquired hypothyroidism, osteopenia, and severe protein-calorie malnutrition.
No significant personal or family history.
Physical examination showed an ill-appearing cachectic woman in moderate distress who responded to questions appropriately. S1 and S2 sounds were present, as well as an ejection murmur and friction rub on cardiovascular examination. Lung auscultation revealed decreased breath sounds at the left lower lung base. The abdomen was soft and non-tender to palpation in all quadrants, and extremities were symmetric without pitting edema.
Routine laboratory tests in the ED revealed leukocytosis (white blood cells 19.9/mm3), hypercalcemia (10.5 mg/dL), hyperglycemia (151), hyponatremia (134 mmol/L), lactic acidosis (2.2 mmol/L), elevated troponin (53 ng/L, delta negative), erythrocyte sedimentation rate (126 mm/hr), and C-reactive protein (43.2 mg/dL). All other values, such as coagulation profile, blood gas, liver function tests, and bilirubin levels, were within normal limits.
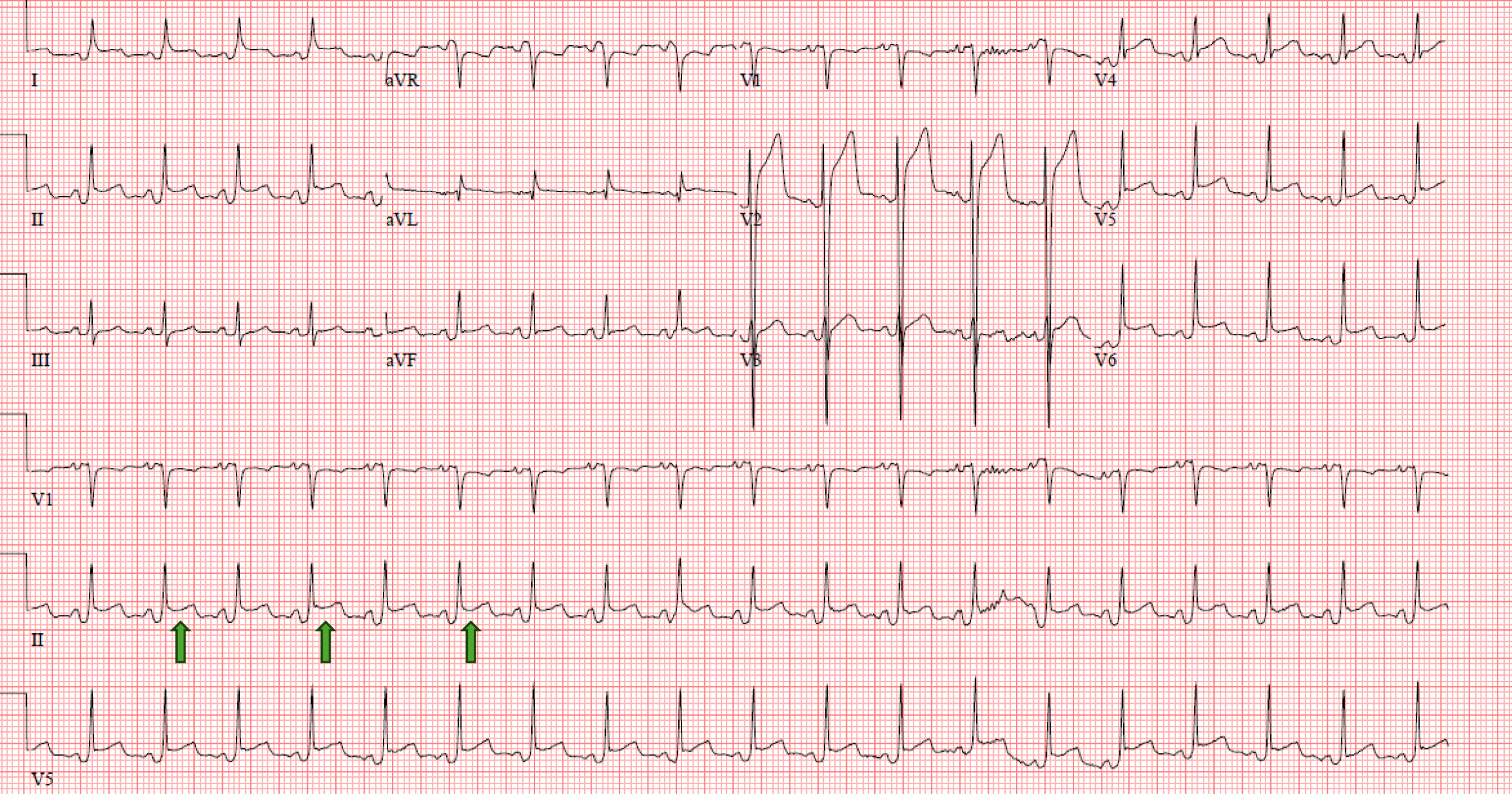
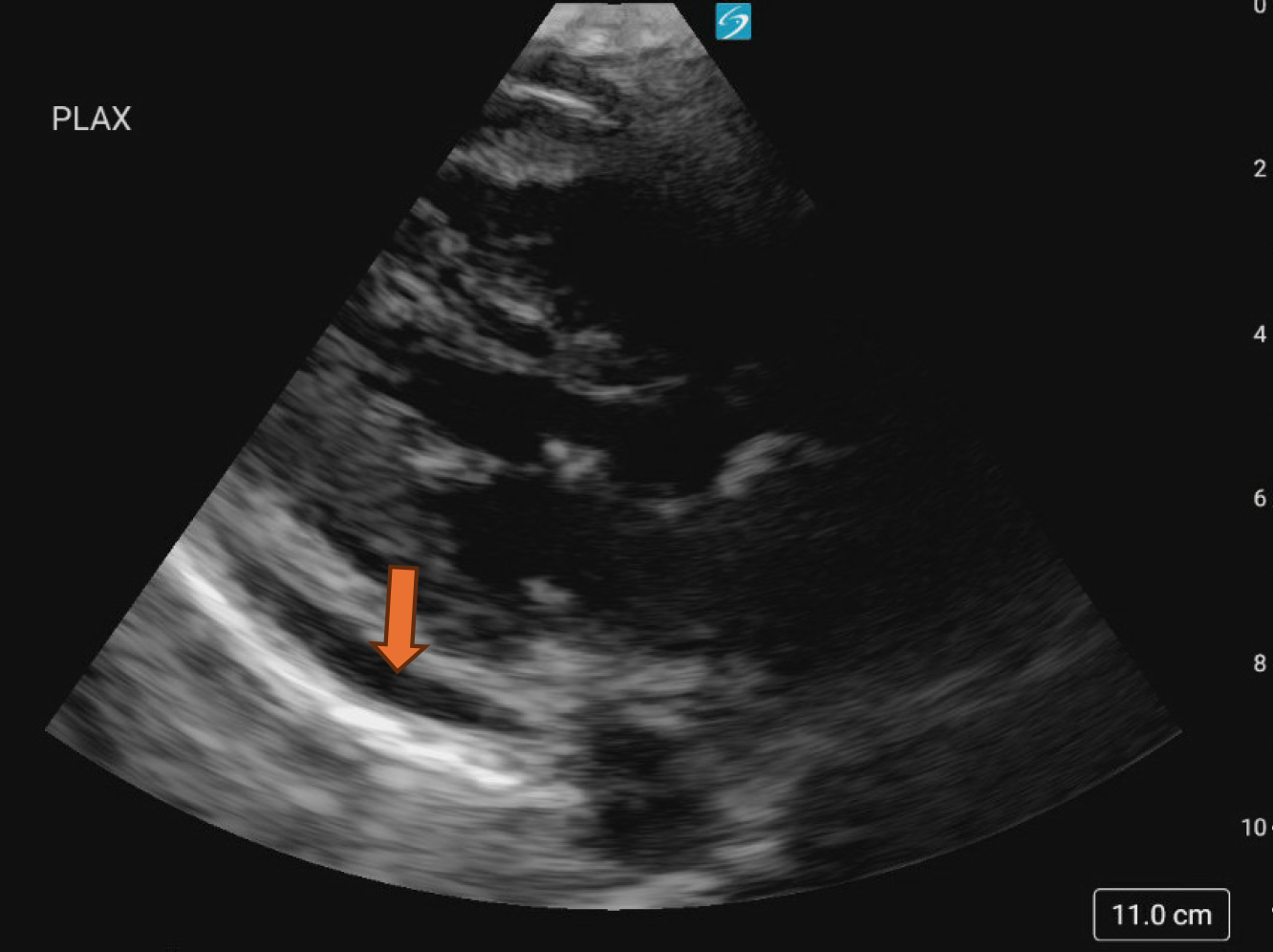
A chest X-ray was done, which showed bilateral pleural calcifications and an increased focal density within the left lower lung base (Figure 1). An electrocardiogram (EKG) was subsequently performed which revealed sinus tachycardia and widespread ST-segment elevation (Figure 2). A bedside point-of-care ultrasound (POCUS) showed a moderate-sized pericardial effusion without evidence of right ventricle or right atrium compression (Figure 3, Video). A computed tomography scan of the chest subsequently revealed similar findings on a bedside echocardiogram. Cardiology was consulted, who recommended admission to Internal Medicine for further management.
Purulent pericarditis secondary to community-acquired pneumonia.
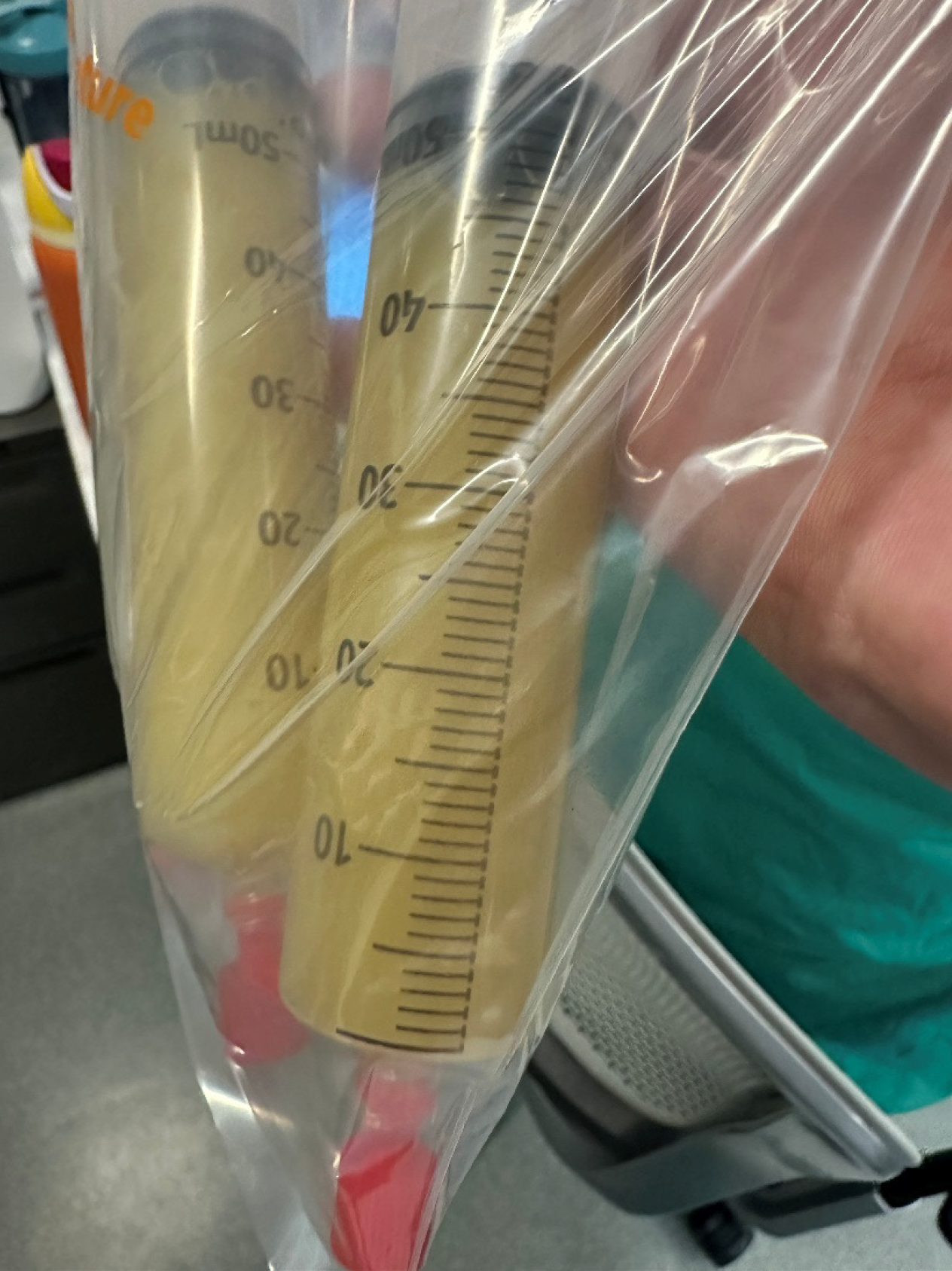
The patient was hospitalized, where she was initiated on ibuprofen and colchicine. She subsequently underwent emergent pericardiocentesis 7 hours later, yielding 480 mL of purulent yellow fluid (Figure 4). The patient was started on broad-spectrum antibiotics (vancomycin and ceftriaxone) immediately after her procedure. Fluid analyses were sent where cultures grew S. pneumoniae within two hours.
She developed septic shock and atrial fibrillation that required a brief stint in the intensive care unit (ICU) after pericardiocentesis. The patient was transitioned back to the medical floor, where antibiotics were deescalated to ceftriaxone. She was discharged in stable condition on amoxicillin, ibuprofen, and colchicine, with the advice of cardiology and infectious disease follow-up.
Acute pericarditis is a condition that involves inflammation of the pericardial sac and accounts for up to 5% of ED visits for non-ischemic chest pain in Western Europe and North America[7]. The incidence in the Western world is approximately 27.7 cases per 100000 people annually[8]. Physical examination can demonstrate findings such as pulsus paradoxus and friction rub[7,8]. However, these are found in less than 50% of patients presenting with an effusion[9]. Laboratory findings such as elevated inflammatory markers can be seen, and EKG findings will show diffuse ST-segment elevation, electrical alternans, PR depression, or low voltage criteria[10]. Risk factors for pericarditis include viral infections, cardiac surgery, connective tissue disorders, renal failure, and neoplasms[9,10]. Rare causes of acute pericarditis include pneumonia, which can induce purulent pericarditis, also known as pyopericarditis[11].
Purulent pericarditis has an incidence rate of approximately 0.005%[5]. It remains a lethal condition due to complications such as septic shock and cardiac tamponade[12]. This form of pericarditis is virtually fatal without treatment with antibiotics. Mortality rates are as high as 100% if left untreated and 40% in treated patients[6,13]. Purulent pericarditis represents a minority of cases, with staphylococcus aureus being the most common isolated organism, followed by S. pneumoniae, Haemophilus influenza, and anaerobes[14]. Intrathoracic spread of the organism to the pericardium in the context of pneumonia is the most common mechanism[5,15]. However, purulent pericarditis secondary to pneumonia is still exceedingly rare, with an approximate incidence of 9% over the past few decades[16,17]. Purulent pericarditis can also occur via hematogenous spread from non-radiologically significant pneumonia or other occult infection[5,14,15].
In this case, our patient had a previous community-acquired pneumonia that likely resulted in the translocation of the bacteria into the pericardium, resulting in her purulent pericarditis. Bedside POCUS immediately identified her pericardial effusion, which was drained promptly. Pericardial fluid cultures were sent, and broad-spectrum intravenous antibiotics were initiated immediately. Although the patient developed septic shock, requiring a brief stint in the ICU, she was discharged in stable condition. The clinical outcome of this case underscores the importance of prompt identification and intervention of suspected purulent pericarditis that is universally fatal if delayed or left untreated. Providers should maintain a high index of clinical suspicion of purulent pericarditis for patients with fever and pericardial effusion on bedside POCUS, as early intervention is crucial to obtain good clinical outcomes.
In summary, we report an extremely rare case of purulent pericarditis secondary to community-acquired pneumonia. This case report highlights the attention that should be given to patients who clinically present with fever and a pericardial effusion on bedside ultrasound. Immediate intervention can result in good clinical outcomes in a virtually fatal condition if left untreated.
| 1. | Lazarou E, Tsioufis P, Vlachopoulos C, Tsioufis C, Lazaros G. Acute Pericarditis: Update. Curr Cardiol Rep. 2022;24:905-913. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 2. | Imazio M, Trinchero R. Triage and management of acute pericarditis. Int J Cardiol. 2007;118:286-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 53] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 3. | Kloos JA. Characteristics, Complications, and Treatment of Acute Pericarditis. Crit Care Nurs Clin North Am. 2015;27:483-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | de Leau MM, Kuipers RS. Cardiovascular complications of Streptococcus pneumoniae bacteraemia. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Pankuweit S, Ristić AD, Seferović PM, Maisch B. Bacterial pericarditis: diagnosis and management. Am J Cardiovasc Drugs. 2005;5:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 114] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Lee ES, Lin C, Pizula J, Pandya KA, Mehra AO, Van Herle H. Purulent Bacterial Pericarditis: Rare Yet Lethal. JACC Case Rep. 2024;29:102282. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Cremer PC, Klein AL, Imazio M. Diagnosis, Risk Stratification, and Treatment of Pericarditis: A Review. JAMA. 2024;332:1090-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 29] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 8. | Vecchié A, Chiabrando JG, Dell MS, Bonaventura A, Mauro AG, Wohlford G, Van Tassell BW, Berrocal DH, Montecucco F, Beutler A, Paolini JF, Gal TS, Abbate A. Clinical Presentation and Outcomes of Acute Pericarditis in a Large Urban Hospital in the United States of America. Chest. 2020;158:2556-2567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Khan MS, Khan Z, Banglore BS, Alkhoury G, Murphy L, Georgescu C. Primary purulent bacterial pericarditis due to Streptococcus intermedius in an immunocompetent adult: a case report. J Med Case Rep. 2018;12:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Masek KP, Levis JT. ECG diagnosis: acute pericarditis. Perm J. 2013;17:e146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Cronier P, Eugène B, Passefort S, Gryman R. A pneumococcal purulent pericarditis revealing a pneumonia and complicated by an acute cardiac tamponade. J Cardiol Cases. 2012;5:e61-e64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Green K, Rothweiler S, Attarha B, Seeram VK. Purulent pericarditis, an unusual cause of cardiac arrest. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Ferreira dos Santos L, Moreira D, Ribeiro P, Rodrigues B, Correia E, Nunes L, Sequeira M, Albuquerque A, Barros I, Saraiva JP, Santos O. [Purulent pericarditis: a rare diagnosis]. Rev Port Cardiol. 2013;32:721-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Bhaduri-McIntosh S, Prasad M, Moltedo J, Vázquez M. Purulent pericarditis caused by group a streptococcus. Tex Heart Inst J. 2006;33:519-522. [PubMed] |
| 15. | Sabanci R, Saeed Al-Asad K, Saaed M, Geunwon Kim A, Martinez A, Banga S, Abela G. A Rare Case of Streptococcus pneumoniae Complicated With Pericardial Abscess. Cureus. 2023;15:e47780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Goodman LJ. Purulent Pericarditis. Curr Treat Options Cardiovasc Med. 2000;2:343-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Sagristà-Sauleda J, Barrabés JA, Permanyer-Miralda G, Soler-Soler J. Purulent pericarditis: review of a 20-year experience in a general hospital. J Am Coll Cardiol. 1993;22:1661-1665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 186] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/