Published online Sep 16, 2025. doi: 10.12998/wjcc.v13.i26.105486
Revised: April 19, 2025
Accepted: May 29, 2025
Published online: September 16, 2025
Processing time: 162 Days and 22.2 Hours
Acute pulmonary thromboembolism is a complication of venous thrombosis. Ex
This case report describes an extreme rescue process for a patient with a preset inferior vena cava (IVC) filter in a relatively economically underdeveloped area with an insufficient supply of consumables. In an emergency, veno-arterial ECMO was successfully initiated by intubation through the IVC filter to the right atrial opening without displacement of the filter during the entire process.
This study demonstrates that in resource-limited settings, femoral vein cannula
Core Tip: Managing pulmonary thromboembolism in critically ill patients with pre-positioned inferior vena cava filters poses significant challenges, especially in resource-limited settings. This case report describes the successful initiation of veno-arterial extracorporeal membrane oxygenation using femoral vein cannulation through a 32 mm inferior vena cava filter without complications. Careful pre-procedural evaluation ensured safe extracorporeal membrane oxygenation support and filter integrity. Our findings provide a feasible emergency strategy for intensive care physicians facing similar scenarios, offering a life-saving approach when conventional access is limited.
- Citation: Gao F, Ma S, Xiao X, Yang H, Qian MJ. Emergency veno-arterial extracorporeal membrane oxygenation cannulation through the femoral vein with a pre-positioned inferior vena cava filter: A case report. World J Clin Cases 2025; 13(26): 105486
- URL: https://www.wjgnet.com/2307-8960/full/v13/i26/105486.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i26.105486
Pulmonary thromboembolism (PTE) is a life-threatening condition often caused by lower extremity deep vein thrombosis (DVT), heart disease, and tumors. In less-developed regions, PTE rescue success rates remain low due to limited re
A 49-year-old female patient was diagnosed with gastric horn signet-ring cell carcinoma (cT3N1M0, stage IIIA). With no history of heart disease or contraindications to surgery, she underwent laparoscopic gastrectomy for gastric cancer, jejunojejunostomy, and abdominal chemical perfusion under general anesthesia. The surgery was performed at the gastrointestinal surgery department. The patient experienced dyspnea, sweating, tachycardia (132 beats per minute), hypoxemia (71%), and hemodynamic instability (73/42 mmHg) on the third postoperative day. The D-dimer level was 10.18 mg/L, which reference value was less than 0.5 mg/L. The patient was considered to be a high-risk PTE. Given the high risk of transport, computed tomography pulmonary angiography was abandoned. Instead, she was rushed to the interventional operating room for catheter-directed therapy. The main pulmonary artery and its distal branches were not shown by angiography (Figure 1).
A 49-year-old female patient, she underwent laparoscopic gastrectomy for gastric cancer, jejunojejunostomy, and abdominal chemical perfusion under general anesthesia. The surgery was performed at the gastrointestinal surgery department.
History with gastric horn signet-ring cell carcinoma (cT3N1M0, stage IIIA). The patient had no history of heart disease.
No family history.
The patient experienced dyspnea, sweating, tachycardia (132 beats per minute), hypoxemia (71%), and hemodynamic instability (73/42 mmHg) on the third postoperative day.
The D-dimer level was 10.18 mg/L, which reference value was less than 0.5 mg/L.
The main pulmonary artery and its distal branches were not shown by angiography (Figure 1).
Intraoperative evidence revealed thrombosis of the left main pulmonary artery and its branches, as well as DVT in both lower limbs (Figure 1).
The interventional doctor performed IVC filter implantation and pulmonary artery internal tube hemolysis. After systemic administration of 3000 U heparin, an IVC filter (WXF-32 IIIicium® vena cava filter system) with a diameter of 32 mm was implanted at 0.5 cm from the renal vein opening. A catheter was then placed into the pulmonary artery thrombus, and 30 wu of urokinase was slowly injected locally after mechanical balloon thrombolysis. The patient was transferred to the ICU for further treatment including active anticoagulation, optimized use of vasoactive drugs, mechanical ventilation, and continuous renal replacement therapy. The doctor first administered an intravenous infusion of 20 wu urokinase first after 16 hours, followed by continuous intravenous infusion of 20 wu urokinase. However, hemodynamics remained unstable and the patient remained in critical condition with persistent pulmonary hypertension and unstable vital signs. It was not possible to re-transport for filter removal.
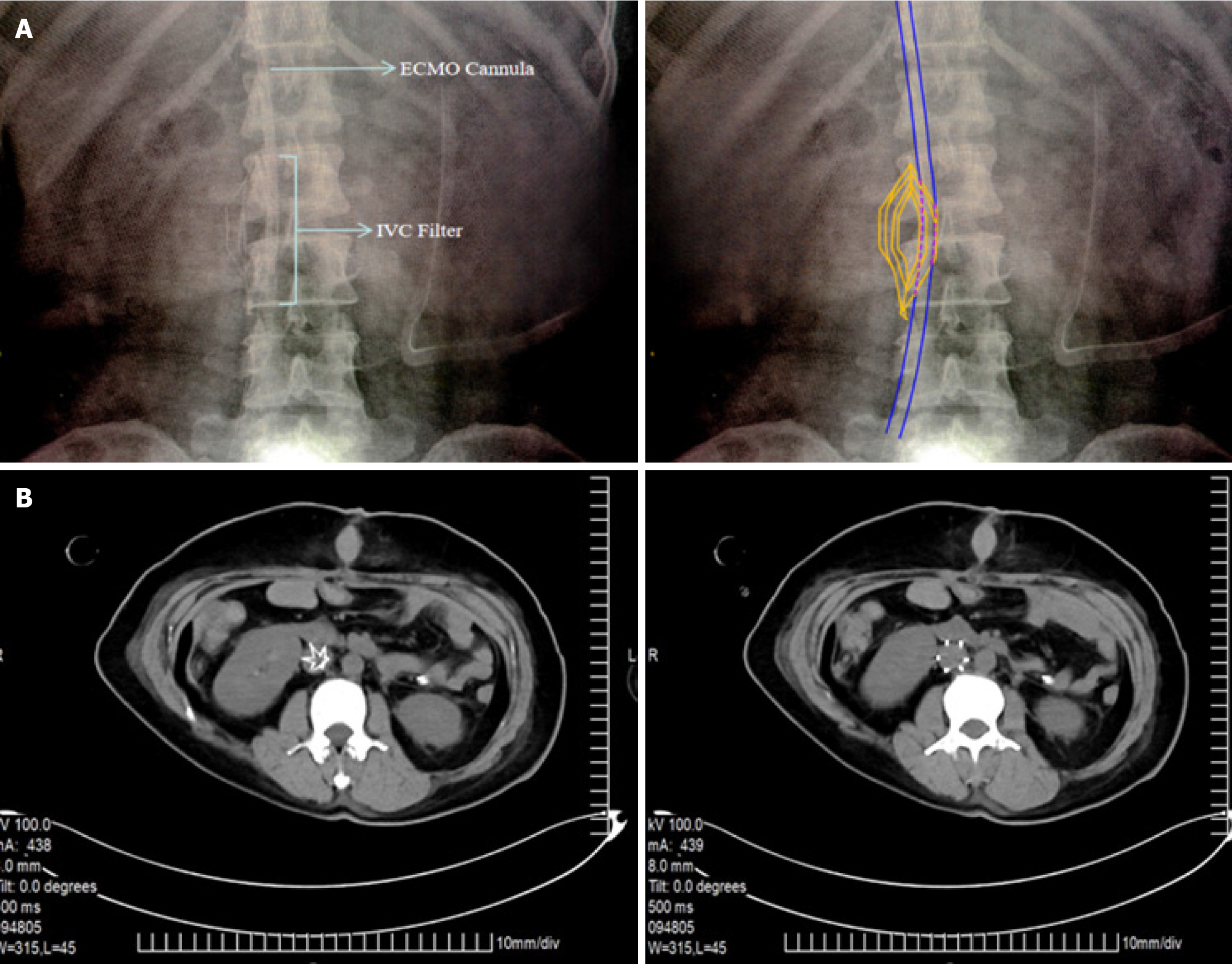
To save her life, after repeatedly confirming the absence of new thrombi around the filter and careful evaluation of the inherent physical conditions of the drainage cannula by bedside color Doppler ultrasonography, the ICU doctor chose the right femoral vein to insert a 20 Fr single-stage, disposable extracorporeal circulation femoral vein catheter at the 20th hour from the patient’s onset (Changzhou Longlefu Medical Materials Co., Ltd.). The 45 cm intubation successfully reached the right atrial opening (Figure 2A), and ipsilateral femoral artery cannulation was successful. Rescue VA-ECMO was successfully initiated. Subsequently, vasoactive drugs were quickly stopped, and arterial oxygen partial pressure increased. Anticoagulation with low molecular weight heparin was given after ECMO withdrawal. Oral rivaroxaban was given for 3 months after discharge.
The patient’s hemodynamics returned to normal following the above intervention. A bedside abdominal X-ray showed that the filter remained at the L2 level without displacement and that the venous drainage catheter was running through the hollow area of the filter. After 5 days of VA-ECMO support, the patient was successfully removed from the machine. Computed tomography revealed no thrombosis in the IVC. No displacement was observed in the filter (Figure 2B). The extubation process did not affect the filter. The patient was transferred out of the ICU without tracheal intubation on the third day after VA-ECMO removal. After 6 months of follow-up, the patient was in good living conditions without complications.
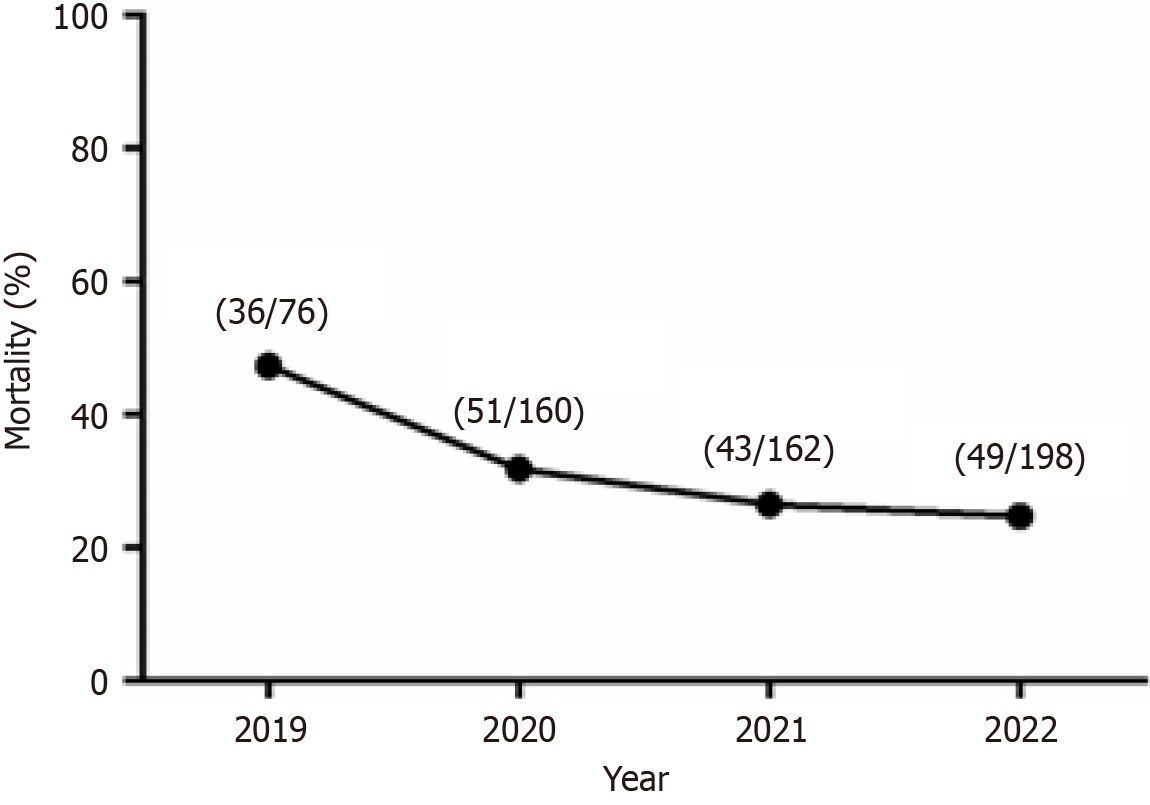
The diagnosis and treatment of PTE have improved with the development of the global economy. It has been reported that the mortality rate of PTE in the Asian population has decreased in general[11]. The all-cause mortality rate of PTE in China also showed a significant downward trend from 2009 to 2015[12]. The northern part of Guizhou is characterized by heavy terrain, inconvenient transportation, and a relatively underdeveloped economy. In recent years, the rapid deve
This case is of a female who has lived in the plateau area for a long time, an environment that might increase the risk of VTE formation[13]. In contrast, solid gastric tumors increase the risk of PTE. After confirming PTE diagnosis, active thrombolysis and catheter-directed therapy were administered; however, both were ineffective. Continuous right ventricular failure caused hemodynamic failure. Extracorporeal cardiopulmonary support needed to be initiated as soon as possible, but the patient’s preset filter system in the IVC increased the concern of the critical care physician. Careful evaluation revealed that ECMO femoral vein intubation and the extubation process did not cause migration of the filter or thrombus, which successfully saved her life. The rescue process used in this case may provide a feasible reference for critical care physicians when performing ECMO intubation in patients with preset IVC filters.
There were some risks when the venous drainage cannula was routed through the IVC filter, including failed pass, displacement of the filter and vascular injury. In order to avoid these risks, it is necessary to evaluate the diameter of the filter aperture and the ECMO drainage cannula before operation. In this case, the aperture of the filter was 10 mm, and the outer diameter of the drainage cannula was 6.67 mm. The distance from the femoral vein puncture point to the filter was measured. During the operation, when the drainage catheter reached the filter, if it was blocked, it was withdrawn by 5 cm, adjusting the direction and slowly advancing the cannula again. After operation, the position of the filter was checked by ultrasound again.
We showed some key points of successful operation: (1) Adequate preoperative evaluation: Ultrasound evaluation of the diameter of the IVC, the location of the filter, and the absence of new thrombosis around the filter. Evaluation of the drain line outer and filter diameter, ensuring drain line Fr < IVC filter aperture; (2) Intraoperative attention points: Forcing through filters is not recommended. Encountering resistance, it is necessary to withdraw the catheter by 5 cm or more, adjust the direction and push the catheter again; and (3) Postoperative evaluation: The position of the filter was reviewed by bedside ultrasound and X-ray after operation.
In resource-limited areas, for patients with a pre-installed IVC filter but requiring initiation of rescue ECMO, a 20 Fr femoral vein catheter can reach the right atrial opening through the 32 mm diameter filter in the IVC, as confirmed by careful ICU evaluation. ECMO intubation and weaning had minimal effects on the filter. Our findings may provide a feasible reference for critical care physicians when performing ECMO intubation in this patient group.
The authors thank the patient and her family for their assistance.
| 1. | Jung YJ, Seo HS, Park CH, Jeon HM, Kim JI, Yim HW, Song KY. Venous Thromboembolism Incidence and Prophylaxis Use After Gastrectomy Among Korean Patients With Gastric Adenocarcinoma: The PROTECTOR Randomized Clinical Trial. JAMA Surg. 2018;153:939-946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Sørensen HT, Mellemkjaer L, Olsen JH, Baron JA. Prognosis of cancers associated with venous thromboembolism. N Engl J Med. 2000;343:1846-1850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1128] [Cited by in RCA: 1204] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 3. | Tanizawa Y, Bando E, Kawamura T, Tokunaga M, Makuuchi R, Iida K, Nanri K, Yoneyama M, Terashima M. Prevalence of deep venous thrombosis detected by ultrasonography before surgery in patients with gastric cancer: a retrospective study of 1140 consecutive patients. Gastric Cancer. 2017;20:878-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Corsi F, Lebreton G, Bréchot N, Hekimian G, Nieszkowska A, Trouillet JL, Luyt CE, Leprince P, Chastre J, Combes A, Schmidt M. Life-threatening massive pulmonary embolism rescued by venoarterial-extracorporeal membrane oxygenation. Crit Care. 2017;21:76. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 110] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (1)] |
| 5. | Elbadawi A, Mentias A, Elgendy IY, Mohamed AH, Syed MH, Ogunbayo GO, Olorunfemi O, Gosev I, Prasad S, Cameron SJ. National trends and outcomes for extra-corporeal membrane oxygenation use in high-risk pulmonary embolism. Vasc Med. 2019;24:230-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Kucher N, Rossi E, De Rosa M, Goldhaber SZ. Massive pulmonary embolism. Circulation. 2006;113:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 483] [Article Influence: 24.2] [Reference Citation Analysis (0)] |
| 7. | Konstantinides SV, Meyer G, Becattini C, Bueno H, Geersing GJ, Harjola VP, Huisman MV, Humbert M, Jennings CS, Jiménez D, Kucher N, Lang IM, Lankeit M, Lorusso R, Mazzolai L, Meneveau N, Ní Áinle F, Prandoni P, Pruszczyk P, Righini M, Torbicki A, Van Belle E, Zamorano JL; ESC Scientific Document Group. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41:543-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1251] [Cited by in RCA: 2935] [Article Influence: 587.0] [Reference Citation Analysis (1)] |
| 8. | Tahir UA, Carroll B, Pinto DS. Massive pulmonary embolism: embolectomy or extracorporeal membrane oxygenation? Curr Opin Crit Care. 2019;25:630-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Pau D, Kasal J, Plisco M. Venovenous ECMO cannulation in a patient with a pre-existing IVC filter. Intensive Care Med. 2018;44:1573-1574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Le NM, Dang UT, Vu HV, Nguyen HL. Bicaval dual lumen cannula placement using transthoracic echocardiography in COVID-19 scenario: pearls and pitfalls. BMJ Case Rep. 2022;15:e249195. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 11. | Lee LH, Gallus A, Jindal R, Wang C, Wu CC. Incidence of Venous Thromboembolism in Asian Populations: A Systematic Review. Thromb Haemost. 2017;117:2243-2260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 128] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 12. | Zhai Z, Wang D, Lei J, Yang Y, Xu X, Ji Y, Yi Q, Chen H, Hu X, Liu Z, Mao Y, Zhang J, Shi J, Zhang Z, Wu S, Gao Q, Tao X, Xie W, Wan J, Zhang Y, Zhang S, Zhen K, Zhang Z, Fang B, Wang C; China pUlmonary thromboembolism REgistry Study (CURES) investigators. Trends in risk stratification, in-hospital management and mortality of patients with acute pulmonary embolism: an analysis from the China pUlmonary thromboembolism REgistry Study (CURES). Eur Respir J. 2021;58:2002963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 13. | Algahtani FH, AlQahtany FS, Al-Shehri A, Abdelgader AM. Features and incidence of thromboembolic disease: A comparative study between high and low altitude dwellers in Saudi Arabia. Saudi J Biol Sci. 2020;27:1632-1636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/