Published online Sep 6, 2025. doi: 10.12998/wjcc.v13.i25.106587
Revised: April 6, 2025
Accepted: May 26, 2025
Published online: September 6, 2025
Processing time: 116 Days and 17.4 Hours
Endoscopic retrograde appendicitis therapy (ERAT) is an emerging technique. However, its efficacy remains uncertain, and postoperative complications often exacerbate inflammation, thereby increasing the difficulty of surgery. The use of ERAT in appendicitis remains contentious, prompting the presentation of this case report.
We report the case of a 43-year-old female patient presenting with intermittent right lower abdominal pain for one day. The patient had undergone ERAT six months previously. Examination revealed stent impaction in the appendix, leading to exacerbated inflammation. Subsequently, a solo single-incision laparoscopic appendectomy (SSLA) was performed. The ERAT-related complications increased surgical difficulty and prolonged the operation time. Post-SSLA, the patient was hospitalized for one day and showed favorable recovery upon follow-up.
This case highlights the risks of ERAT. Thorough preoperative assessment, proper stent placement during surgery and regular postoperative follow-up are crucial in preventing complications, as their occurrence can increase surgical difficulty. Compared to ERAT, SSLA remains more widely used in clinical practice. Both techniques require further clinical data and research to optimize their application.
Core Tip: We report the case of appendicitis where post-endoscopic retrograde appendicitis therapy (ERAT) stent impaction worsened inflammation. Ultimately, the novel solo single-incision laparoscopic appendectomy (SSLA) technique successfully removed the appendix. As ERAT is still in its early stages, inadequate technical proficiency, postoperative complications and improper postoperative management can exacerbate the patient's condition and increase surgical difficulty. This case prompts further reflection on the choice between ERAT and SSLA, encouraging the refinement of both techniques. This report emphasizes the importance of preoperative assessment, stent placement, and postoperative management for ERAT, while confirming SSLA's advantages in addressing ERAT complications and healing appendicitis.
- Citation: Ma TT, Lyu HR. Post-endoscopic retrograde appendicitis therapy stent impaction leading to exacerbation of appendicitis: A case report. World J Clin Cases 2025; 13(25): 106587
- URL: https://www.wjgnet.com/2307-8960/full/v13/i25/106587.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i25.106587
Appendicitis, as a common acute abdominal condition, primarily results from fecalith obstruction of the appendix lumen, leading to ischemia, bacterial migration and subsequent infection, necessitating surgical intervention[1]. The standard treatment remains laparoscopic appendectomy (LA). With the advancement of technology, LA has evolved, and endoscopic retrograde appendicitis therapy (ERAT) has emerged as alternative techniques. single-incision LA (SILA), a variant of LA, enhances the advantages of traditional LA, offering faster recovery and less tissue trauma, along with better aesthetic outcomes, although it requires longer operation time[2]. ERAT involves transanal colonoscopy to access the cecum, allowing imaging, decompression, irrigation, and fecalith removal using guidewires, catheters, and retrieval balloons, followed by plastic stent placement for drainage, making it a viable technique for treating uncomplicated acute appendicitis[3].
However, ERAT is still in the exploratory phase, with uncertain efficacy and postoperative complications such as stent impaction, displacement, or dislodgement, which can exacerbate inflammation and increase surgical difficulty[4]. This case report highlights the risks associated with ERAT and the challenges posed by stent impaction. Subsequently, the patient underwent solo SILA (SSLA), a technique pioneered by our center, and recovered well postoperatively. Additionally, it discusses the advantages of SSLA as an innovative surgical method and a feasible approach for managing ERAT-related complications. A literature review of PubMed, using keywords such as “ERAT”, “appendicitis”, “stent impaction”, and “SILA” was conducted to provide a broader context for understanding the clinical significance of this case.
We present the case of a 43-year-old female patient who underwent ERAT six months previously and developed exacerbated appendicitis due to stent impaction, requiring a more complex surgical intervention. This case underscores the importance of perioperative management in ERAT to improve surgical outcomes and reduce complications. It aims to stimulate discussion on the selection of treatment modalities for appendicitis in the new era, offering new insights into the application of SSLA and ERAT in appendicitis management.
A 43-year-old female patient presented to the emergency department with a one-day history of paroxysmal pain in the right lower abdomen.
The patient experienced sudden onset of paroxysmal pain in the right lower abdomen one day previously, accompanied by mild abdominal distension. During the course of the illness, she did not exhibit nausea, vomiting, fever, or chills, and her bowel movements and flatus remained normal.
Six months ago, the patient was evaluated at our hospital for appendicitis with appendicolith but declined surgical treatment. Seeking an alternative approach, she presented to another institution, where she underwent ERAT, appendiceal cavity lavage, and stent placement on July 19, 2024. The procedure involved advancing the endoscope to the appendiceal orifice, followed by guidewire placement into the appendiceal lumen for contrast imaging, which revealed a 4-mm appendiceal lumen with a length of 5–6 cm, exhibiting a U-shaped tortuous configuration. Sand-like appendicoliths were observed within the lumen. After thorough irrigation with normal saline, repeat contrast imaging confirmed satisfactory clearance, and a removable plastic stent [Cook, 5 French (Fr) × 5 cm] was placed in an optimal position and secured with metal clips. The patient had an uneventful postoperative recovery and was discharged on oral cefditoren pivoxil therapy.
The patient stated no family history of hereditary diseases.
The patient's vital signs were as follows: (1) Body temperature: 36.6°C; (2) Blood pressure: 114 mmHg/80 mmHg; (3) Heart rate: 67 beats/minute; and (4) Respiratory rate: 13 breaths/minute. Physical examination revealed a flat abdomen without visible intestinal peristalsis or peristaltic waves. Notably, there was marked tenderness at McBurney's point in the right lower quadrant, accompanied by mild localized abdominal muscle tension. No tenderness or rebound tenderness was observed in other abdominal regions.
Laboratory tests revealed a mild elevation in white blood cell count to 10.64 × 109/L, with a neutrophil percentage of 86.0% and an absolute neutrophil count of 9.15 × 109/L. Hemoglobin was 114 g/L, and no other abnormalities were detected in the remaining laboratory parameters.
An unenhanced abdominal and pelvic computed tomography scan revealed the presence of an indwelling stent within the cecum and appendix (Figure 1A). The appendix appeared enlarged, with a maximal diameter of approximately 1.6 cm, and exhibited mild wall thickening. Two nodular hyperdense shadows were observed within the appendiceal lumen (Figure 1B and C). The surrounding and pelvic fat spaces appeared blurred, and the adjacent peritoneum exhibited mild thickening, suggesting inflammation involving the appendix and surrounding tissues. Additionally, a sizable appendicolith remained within the appendiceal lumen, indicating incomplete removal.
Acute recurrence of chronic appendicitis following ERAT.
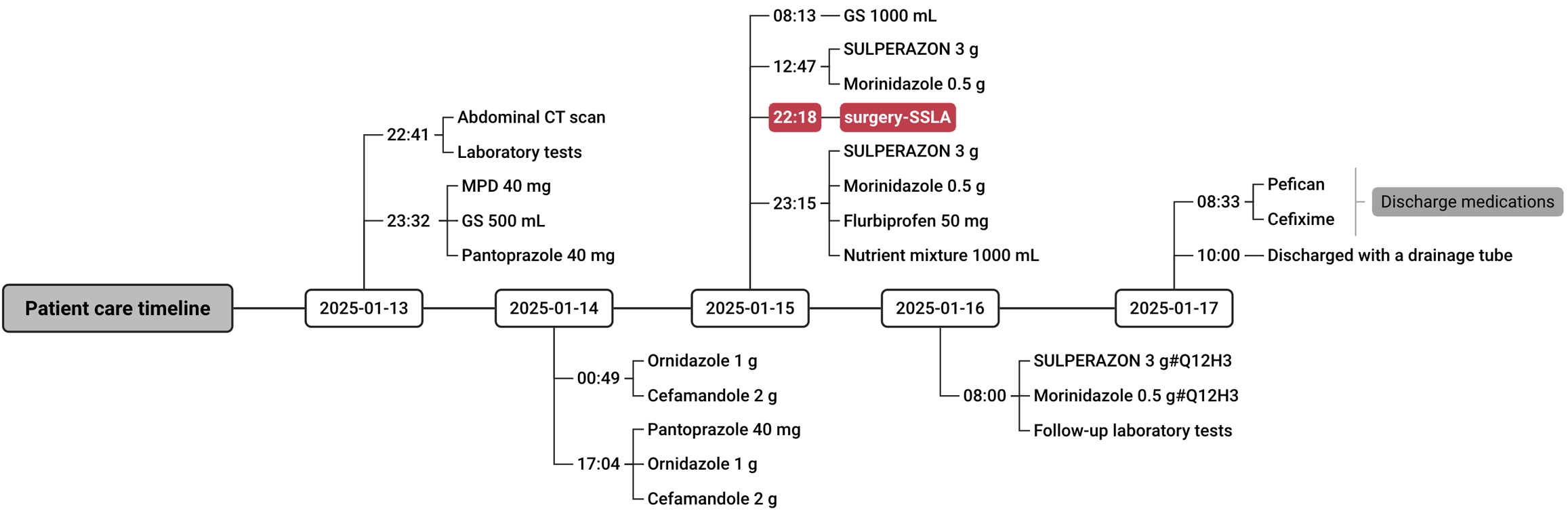
After discussion with the patient, SSLA was performed. Perioperative medication details are shown in Figure 2.
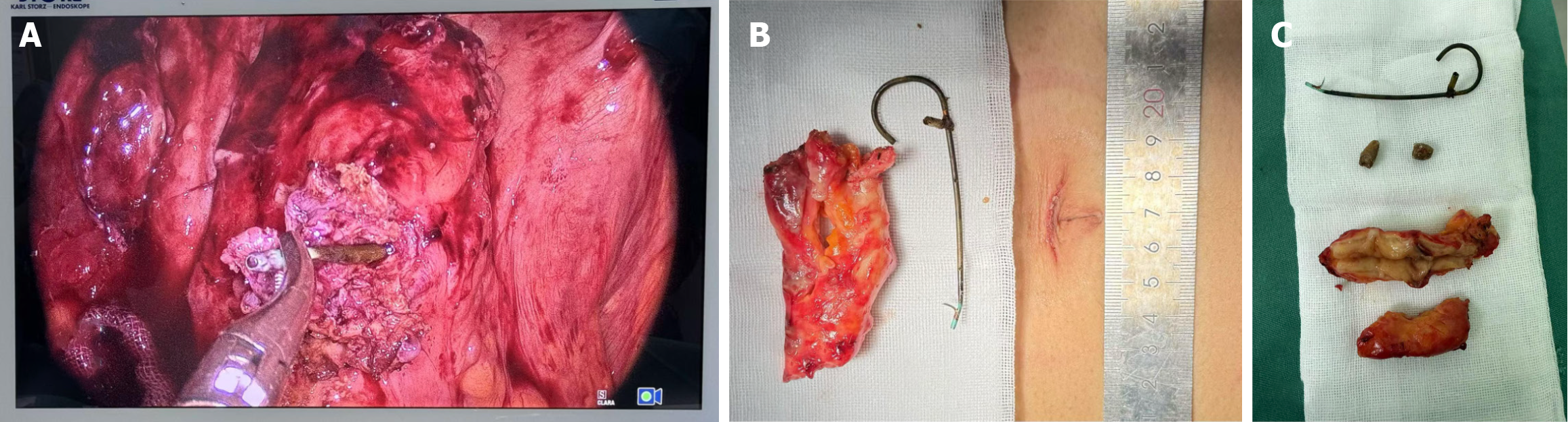
A transumbilical incision was made to access the abdominal cavity, revealing grayish-white purulent fluid and fibrinous exudates in the paracolic gutter, interloop spaces, and pelvic cavity. These were irrigated, aspirated, and cleared. Adhesiolysis of the cecum was performed, exposing a significantly swollen appendix with thickened walls and purulent discharge. The mesoappendix appeared edematous. Upon incision of the appendiceal wall, the previously placed stent was visualized within the lumen (Figure 3A), showing dense fibrotic adhesion with the appendiceal mucosa, making separation difficult. Consequently, a 1-cm incision was made at the cecal base, allowing complete removal of the stent from within the cecum. The appendix was then excised, and the cecal incision was closed with a continuous V-lock suture, reinforced at the seromuscular layer. Meticulous hemostasis was achieved, and a 20-Fr drainage tube was placed at the right anterior axillary line at the umbilical level. The operation lasted 84 minutes, with an intraoperative blood loss of 30 mL.
The excised appendix was markedly swollen, and upon sectioning, two appendicoliths were identified (Figure 3B and C). Histopathological examination confirmed acute appendicitis with periappendicitis, while a separate pathological analysis of the appendiceal base revealed chronic enteritis with acute inflammation.
On postoperative day 1, a repeat complete blood count showed normalization of the white blood cell level. At the two-week follow-up, the patient reported pain relief and had resumed normal daily activities and dietary intake.
The ERAT technique is a relatively new minimally invasive surgical method that has demonstrated potential in the treatment of appendiceal diseases, particularly appendicitis caused by appendicoliths[5]. This endoscopic approach offers the benefits of reduced surgical trauma and shorter postoperative recovery times compared with traditional open surgery[6]. Compared with antibiotic monotherapy, patients receiving ERAT combined with antibiotics exhibited a lower recurrence rate[4]. However, while ERAT effectively addresses the obstructive etiology of appendicitis, it does not eliminate the risk of residual appendicoliths migrating into the lumen. Moreover, ERAT is not recommended for patients with pericecal abscesses or perforated appendicitis. As its use becomes more widespread, attention has increasingly focused on postoperative complications. If these complications are not managed promptly and appropriately, the inflammation may persist or worsen, frequently necessitating subsequent surgical appendectomy. Such interventions are often complicated by significant adhesions, thereby increasing the technical difficulty of the surgery[4].
Although ERAT offers significant advantages in terms of minimal invasiveness, the technique remains in its developmental phase, is technically demanding, and requires extensive operator experience. Accurate preoperative assessment of the appendiceal lumen and the extent of inflammation are critical for the success of the procedure, while meticulous intraoperative management—such as the appropriate placement of the appendiceal stent—directly influences the occurrence of postoperative complications. Stent displacement and impaction are potential complications associated with ERAT[7], and their incidence is closely related to the precision of the operator's technique[6]. Although the use of an appendiceal stent can effectively alleviate luminal obstruction or inflammatory reactions, improper placement during the procedure may lead to stent displacement or impaction, which can further cause luminal narrowing, exacerbate the symptoms of appendicitis, and even result in appendiceal perforation.
In this case, the patient underwent ERAT, but complete clearance of the appendicoliths from the appendiceal lumen was not achieved, and postoperative follow-up was not performed in a timely manner. Consequently, stent impaction occurred with a secondary exacerbation of appendicitis, highlighting the challenges in the perioperative management of ERAT. Although ERAT reduces surgical trauma and shortens recovery time, it demands rigorous postoperative monitoring. Delayed follow-up may result in missed opportunities for timely intervention, leading to the worsening of complications and adversely affecting the outcomes of subsequent surgical treatments. In particular, for patients with acute appendicitis complicated by complex conditions, complications such as stent infection, impaction, or periappendiceal inflammation can substantially increase the technical difficulty of subsequent procedures. Therefore, ERAT patients require more stringent postoperative follow-up and monitoring to promptly detect and address any issues. In this case, severe fibrotic adhesion between the stent and the appendiceal lumen rendered removal challenging, ultimately necessitating a 1-cm incision in the cecal wall at the appendiceal base for successful retrieval. This measure increased surgical complexity and prolonged postoperative recovery time.
The standard treatment for acute appendicitis remains LA. As a variant of this procedure, SILA has been widely adopted, with its efficacy and safety being well validated[8,9]. Building on this, our center pioneered an innovative technique—SSLA—which retains the advantages of SILA while further eliminating restrictions related to surgical staffing and resolving the instrument interference issues between the assistant and the surgeon typically encountered in SILA. Di Saverio et al[10], in the 2020 Jerusalem guidelines, noted that for complicated appendicitis cases such as appendiceal abscess, appendicoliths, ascites, or intestinal obstruction, traditional multiport laparoscopic surgery may be a safer option. However, with advancements in technology and increasing operator proficiency, SSLA can be safely and effectively employed even in cases of complicated appendicitis. SSLA is generally performed through a small periumbilical abdominal wall incision (approximately 2 cm). Compared to conventional multiport LA, SSLA results in less trauma, faster recovery, and superior cosmetic outcomes. In contrast to ERAT, SSLA does not require the placement of a stent, thereby avoiding complications such as stent impaction due to improper positioning. Moreover, SSLA involves complete excision of the appendix, eliminating the possibility of recurrent appendicitis due to residual inflammation. Additionally, owing to its minimally invasive nature, patients can typically be discharged within 1–2 days postoperatively and resume early mobilization. Although ERAT is minimally invasive, the presence of a stent and the necessity for prolonged postoperative observation may extend the recovery period[4,6]. In the present case, following stent impaction after ERAT, the patient promptly underwent SSLA, which allowed complete removal of the inflamed appendix and extraction of the indwelling stent. The patient was discharged one day after surgery, with the incision healing well; at the two-week follow-up, the patient’s diet and daily activities had returned to normal, and the cosmetic outcome was excellent.
Further refinement and standardization of the ERAT technique necessitate the accumulation of more clinical experience and robust scientific data. Continuous optimization of the surgical procedure and precise preoperative evaluation to minimize complications will facilitate the broader adoption of this approach. Future investigations should focus on the early detection and intervention of postoperative complications and the development of standardized postoperative management protocols, thereby enhancing the safety of ERAT and improving patient outcomes.
This case highlights the risks of ERAT. Thorough preoperative assessment, proper stent placement during surgery and regular postoperative follow-up are crucial in preventing complications, as their occurrence can increase surgical difficulty. Compared to ERAT, SSLA remains more widely used in clinical practice. Both techniques require further clinical data and research to optimize their application.
We extend our heartfelt gratitude to everyone who has contributed to the care of this exceptional patient and the preparation of this article.
| 1. | Moris D, Paulson EK, Pappas TN. Diagnosis and Management of Acute Appendicitis in Adults: A Review. JAMA. 2021;326:2299-2311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 208] [Article Influence: 41.6] [Reference Citation Analysis (112)] |
| 2. | Cai YL, Xiong XZ, Wu SJ, Cheng Y, Lu J, Zhang J, Lin YX, Cheng NS. Single-incision laparoscopic appendectomy vs conventional laparoscopic appendectomy: systematic review and meta-analysis. World J Gastroenterol. 2013;19:5165-5173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Yang B, Kong L, Ullah S, Zhao L, Liu D, Li D, Shi X, Jia X, Dalal P, Liu B. Endoscopic retrograde appendicitis therapy versus laparoscopic appendectomy for uncomplicated acute appendicitis. Endoscopy. 2022;54:747-754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (116)] |
| 4. | Zhang A, Fan N, Zhang X, Guo H, Zhou Y, Zeng L, Lin Y, Jiang X. Endoscopic retrograde appendicitis therapy. Therap Adv Gastroenterol. 2024;17:17562848241275314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 5. | Ma LY, Hu JW, Cai XL, Liu ZQ, Zhong YS, Lin SL, Chen TY, Cai SL, Zhang YQ, Chen WF, Ma LL, Cai MY, Qin WZ, Ma X, Li QL, Zhou PH. Endoscopic retrograde appendicitis therapy for management of chronic fecalith appendicitis. Surg Endosc. 2025;39:409-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 6. | Khan S, Ali FS, Ullah S. Endoscopic Retrograde Appendicitis Therapy: Is it Really a Need of the Hour? Ann Surg. 2023;277:e1-e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Li M, Kong L, Liu B. Missing Plastic Stent, An Unreported Complication of Endoscopic Retrograde Appendicitis Therapy. Gastroenterology. 2022;162:e10-e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 8. | Kang SI, Woo IT, Bae SU, Yang CS. Single-Incision Versus Conventional Laparoscopic Appendectomy: A Multi-Center Randomized Controlled Trial (SCAR trial). Int J Surg Protoc. 2021;25:201-208. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Han Y, Yuan H, Li S, Wang WF. Single-incision versus conventional three-port laparoscopic appendectomy for acute appendicitis: A meta-analysis of randomized controlled trials. Asian J Surg. 2024;47:864-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Di Saverio S, Podda M, De Simone B, Ceresoli M, Augustin G, Gori A, Boermeester M, Sartelli M, Coccolini F, Tarasconi A, De' Angelis N, Weber DG, Tolonen M, Birindelli A, Biffl W, Moore EE, Kelly M, Soreide K, Kashuk J, Ten Broek R, Gomes CA, Sugrue M, Davies RJ, Damaskos D, Leppäniemi A, Kirkpatrick A, Peitzman AB, Fraga GP, Maier RV, Coimbra R, Chiarugi M, Sganga G, Pisanu A, De' Angelis GL, Tan E, Van Goor H, Pata F, Di Carlo I, Chiara O, Litvin A, Campanile FC, Sakakushev B, Tomadze G, Demetrashvili Z, Latifi R, Abu-Zidan F, Romeo O, Segovia-Lohse H, Baiocchi G, Costa D, Rizoli S, Balogh ZJ, Bendinelli C, Scalea T, Ivatury R, Velmahos G, Andersson R, Kluger Y, Ansaloni L, Catena F. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 697] [Cited by in RCA: 693] [Article Influence: 115.5] [Reference Citation Analysis (109)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/