Published online Sep 6, 2025. doi: 10.12998/wjcc.v13.i25.105028
Revised: April 20, 2025
Accepted: May 18, 2025
Published online: September 6, 2025
Processing time: 150 Days and 17 Hours
Idiopathic mesenteric phlebosclerosis (IMP) is a rare condition that causes ischa
We report the case of a 44-year-old woman with chief complaints of abdominal pain, vomiting and decreased defecation. One year prior, the patient was asym
IMP can present with symptoms of pseudoileus as initial complication. Clinicians can use CT and colonoscopy for differential diagnoses.
Core Tip: This case underscores the need for heightened awareness of idiopathic mesenteric phlebosclerosis as a differential diagnosis in patients presenting with symptoms of pseudoileus, particularly those with a history of long-term Chinese herbal medicine use. The characteristic features of colonoscopy and computed tomography scan can help in differential diagnosis when suspecting this disease.
- Citation: Hou XL, Chen J, Cui MH, Yang GB. Extensive idiopathic mesenteric phlebosclerosis presenting as intestinal pseudo-obstruction: A case report. World J Clin Cases 2025; 13(25): 105028
- URL: https://www.wjgnet.com/2307-8960/full/v13/i25/105028.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i25.105028
Idiopathic mesenteric phlebosclerosis (IMP) is a rare disease that causes ischaemic colitis. Since Koyama reported the first case in 1991[1] and Iwashita et al[2] officially named it in 2003, relatively few cases have been reported in the English literature. We describe the case of a patient who was initially misdiagnosed with Crohn’s disease and later diagnosed with IMP, which presented with symptoms of pseudoileus. The patient recovered well after conservative treatment.
A 44-year-old female presented with complaints of abdominal pain for seven days, accompanied by vomiting and decreased defecation for one day.
The patient presented to gastroenterology department with a one-week history of moderate lower abdominal pain and was subsequently referred for an abdominal computed tomography (CT) examination. Following the administration of mannitol and a large volume of water (2000 mL) for intestinal preparation for CT, her abdominal pain significantly worsened, and she began vomiting her gastric contents and defecating a small amount of loose stools. Ten months prior, her abdominal CT scan suggested inflammatory bowel disease based on characteristics similar to those of a diagnosed patient. However, at that time, she was asymptomatic and rejected further evaluation with colonoscopy.
The patient denied any history of hepatitis, tuberculosis, or other common infectious diseases, including amebiasis and schistosomiasis. Additionally, she had no prior history of surgery, trauma, or blood transfusions.
She had been consuming Chinese herbal tea for more than thirty years to alleviate her symptoms of constipation.
Her abdomen was swollen and slightly hard, with mild tenderness throughout but no rebound tenderness. Bowel sounds were decreased at three sounds per minute. Her body mass index was only 12.92 kg/m2.
Her admission laboratory test results were as follows: White blood cell count, 8.76 × 109/L; haemoglobin, 125 g/L; platelet count, 770 × 109/L; C-reactive protein, 148 mg/L; cancer antigen 125, 113.49 U/mL and a positive faecal occult blood test. The results of other laboratory tests, including blood biochemistry, pancreatic enzymes, routine urinalysis, coagulation function, etc., were all within the normal limits or unremarkable.
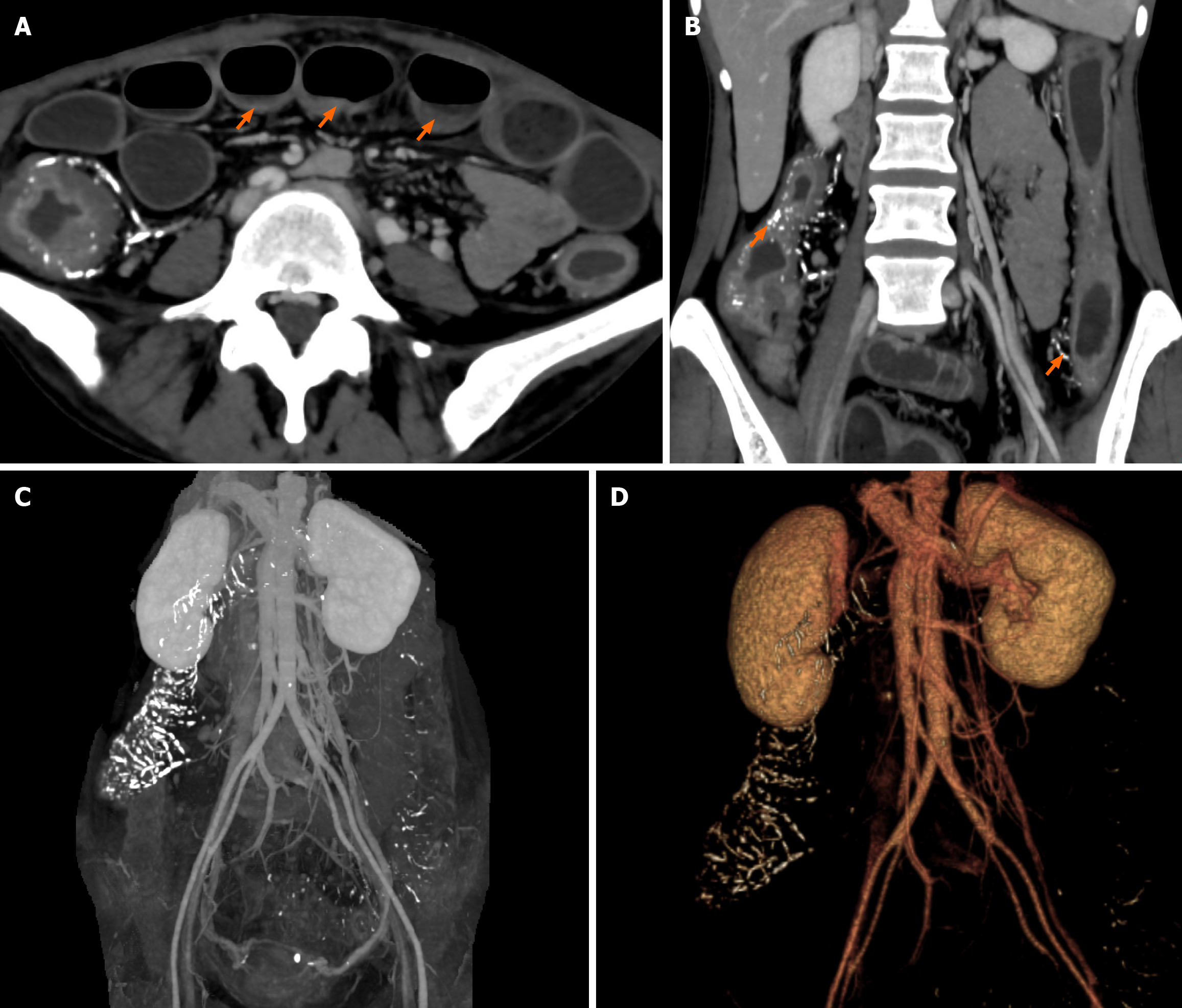
Figure 1 is abdominal CT images revealing remarkable dilatation and fluid collection in the small intestine (Figure 1A), calcification of the pericolonic vein, thickening of the entire colon wall and distal ileum (Figure 1B). And widespread calcification of the distal branches of the superior mesenteric vein and inferior mesenteric vein, among which the calcification of the superior mesenteric vein branches was more severe (Figure 1C and D).
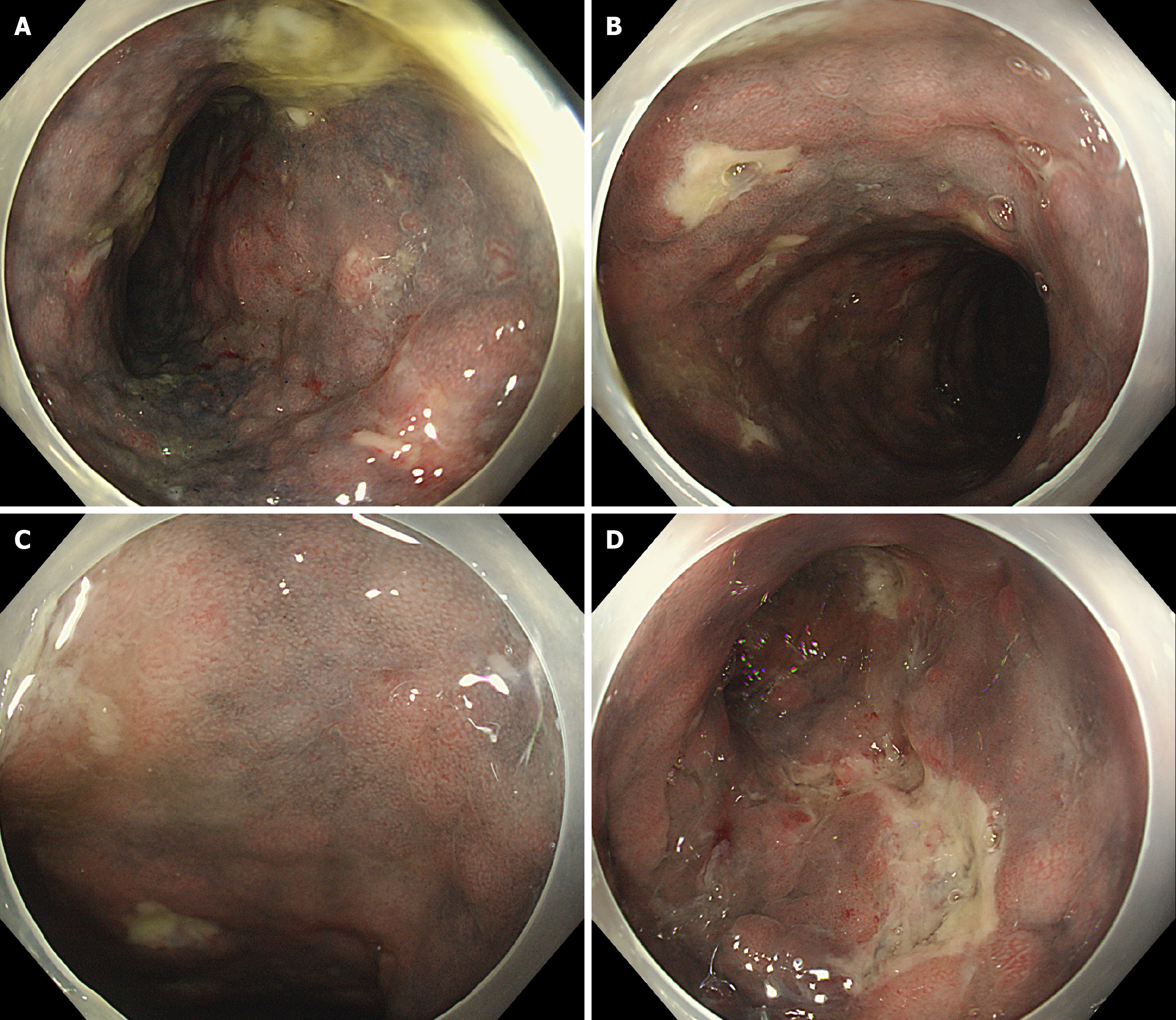
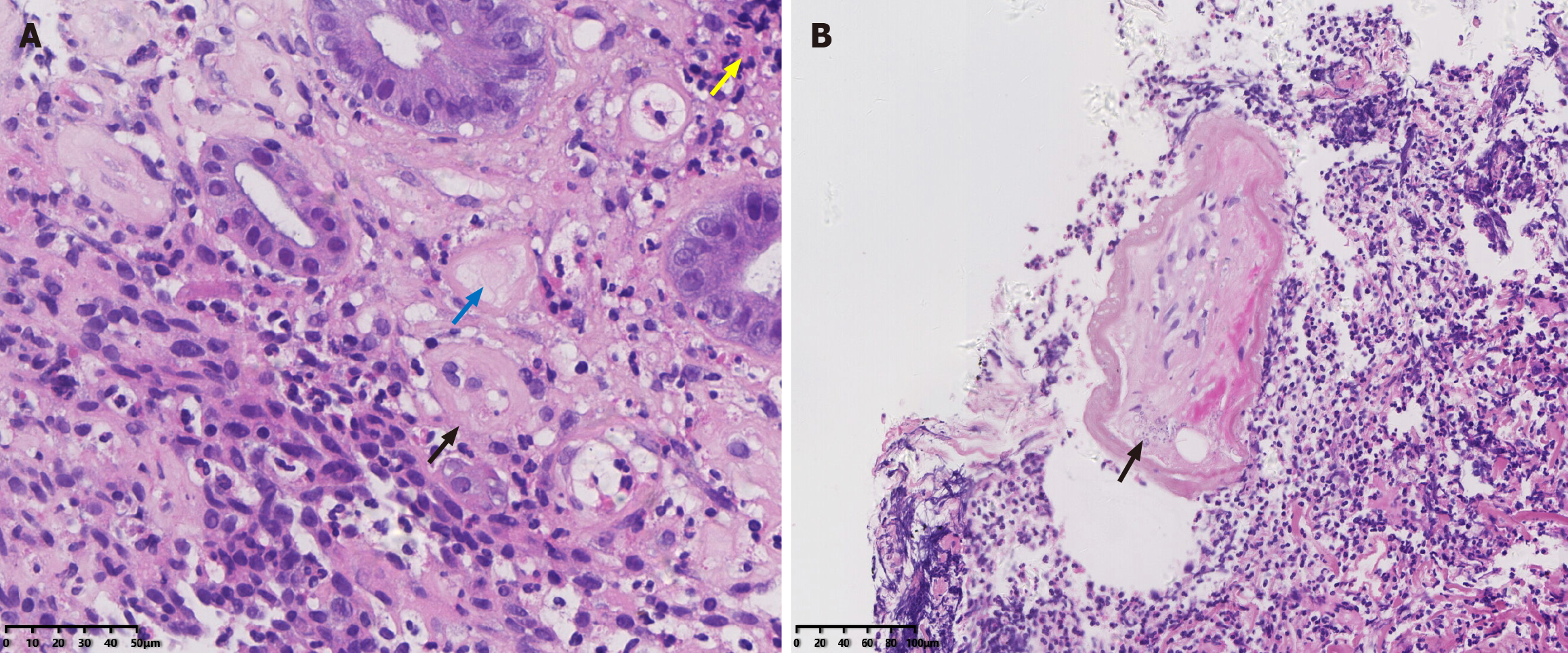
Figure 2 is colonoscopy images revealing dark purple mucosal surfaces with ulcerations of various sizes in the transverse colon (Figure 2A), descending colon (Figure 2B), sigmoid colon (Figure 2C) and rectum (Figure 2D). Figure 3 is endoscopic biopsy samples of the left colon. Endoscopic biopsy pathology images showing inflammatory cell infiltration and the deposition of powdery fibrin in the lamina propria (yellow arrow) (Figure 3A, × 400), fibrous thickening of the wall (black arrow) (Figure 3A, × 400) of small vessels, a cellulose-like substance (blue arrow) (Figure 3A, × 400) in the submucosa, and calcification surrounding the mesenteric vein (black arrow) (Figure 3B, × 200).
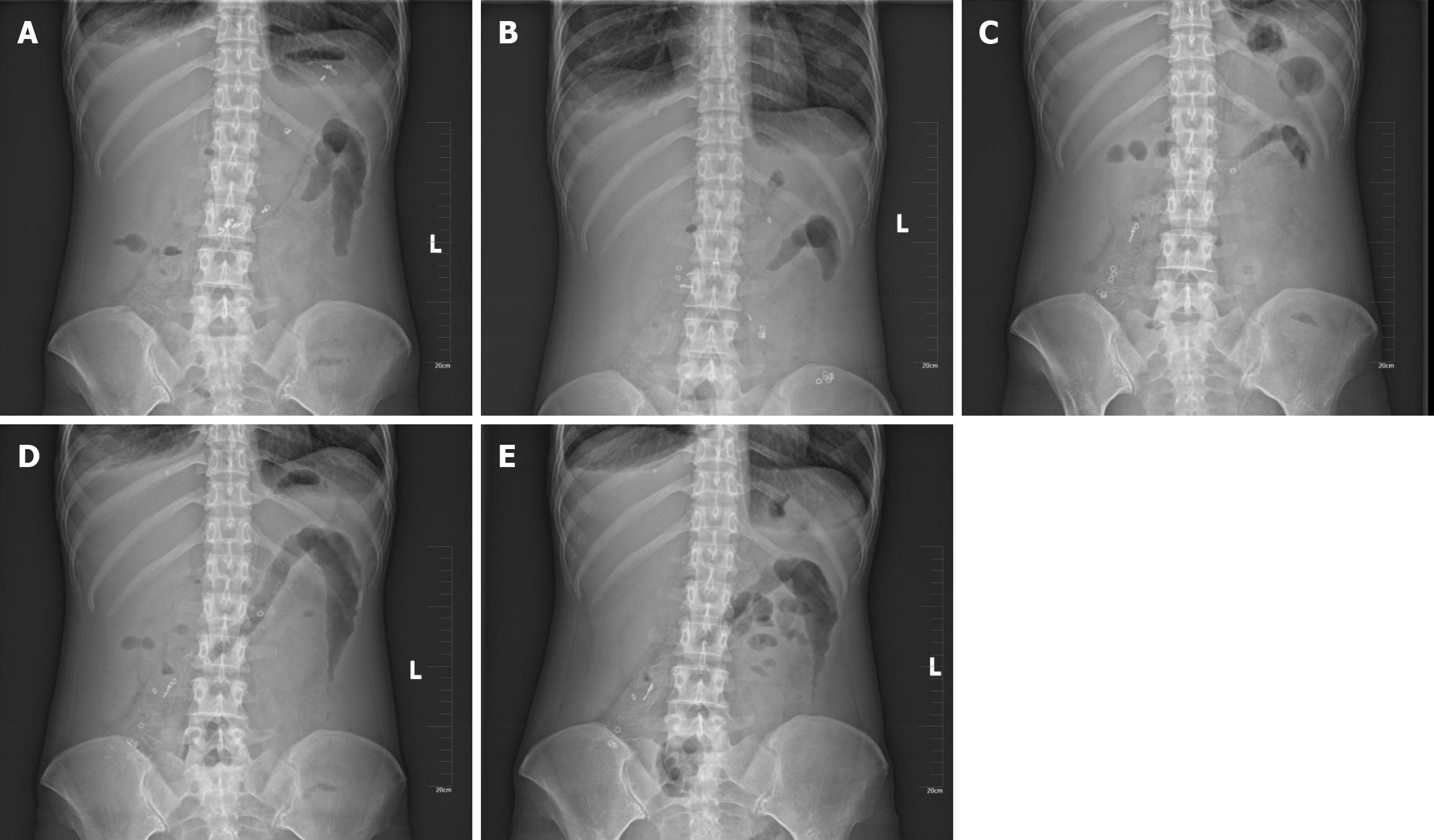
Figure 4 is abdominal X-ray of gastrointestinal marker capsules at 3, 6, 24, 48, and 72 hours after collection. Eleven markers remained in the ascending colon after 72 hours, and minimal movement of the markers was observed from 24 to 72 hours. Figure 5 is patient’s facial features. The patient had a bronze complexion, similar to the colour of her intestinal mucosa.
The final diagnosis was IMP.
The patient was advised to discontinue Chinese herbal tea consumption. Oral intake was prohibited, and conservative medical treatment, including gastrointestinal decompression and parenteral nutritional support was initiated.
The patient’s abdominal pain gradually resolved, and she was able to defecate autonomously. She subsequently resumed oral intake and was discharged thereafter. At the one-year outpatient follow-up, the patient did not report any abdominal pain or other discomfort, such as nausea or vomiting, except for loose, watery stools every day since the discontinuation of Chinese herbal tea consumption.
Although IMP is rare, it can be identified during CT and colonoscopy. The typical CT characteristics of IMP include thickening of the colon wall and calcification of the small mesenteric veins and their intramural branches. Colonoscopy reveals abnormal dark purple or bronze coloured mucosa in nearly all IMP patients[3]. Other endoscopic findings may include reduced distensibility, ulcerations and stenosis. Endoscopic biopsy pathology of the mucosa typically reveals collagen deposition in the lamina propria and thickening of venous walls.
In our patient, colonoscopy revealed an abnormal dark purple left colon with irregular ulcerations, stiffness and stenosis. Although colonoscopy could not be completed because of the stiffness of the enteric cavity, the condition of the right half of the colon was expected to be similar to that of the left half. Endoscopic biopsy pathology of the mucosa of the left colon revealed collagenous fibrin deposition and fibrous thickening and calcification of the venous lumen of the mesenteric vein. IMP predominantly affects the right colon, which is supplied by the superior mesenteric vein. However, in rare cases, the entire colon is involved. Shimizu et al[4] summarized the endoscopic features of IMP in 206 patients who underwent total colonoscopy and reported that 3.9% of patients had rectum involvement, 7.3% had terminal ileum involvement, and 100% had ascending colon involvement. In our patient, CT revealed diffuse thickening of the wall of both the entire colon and distal ileum, in addition to corresponding calcification in the distal tributaries of both the superior and inferior mesenteric veins. Notably, calcification of the superior mesenteric vein branches supplying the right colon was more prominent.
The specific pathogenesis of IMP remains unclear. Most patients diagnosed with IMP have a history of long-term traditional Chinese medicine use. More cases have been reported in Asia than in both Europe and America, likely due to the widespread use of traditional Chinese medicines in Asia. The underlying pathogenesis may involve the absorption of a certain substance into the mesenteric veins following oral intake, resulting in diffuse chronic intestinal ischaemia and changes in the color of the intestinal mucosa[5]. In previous reports, researchers have suggested a possible relationship between IMP and the long-term use of traditional Chinese medicines, such as Sanshishi and Angelica sinensis[6-10], among which the former has been reported the most frequently. In our case, the main ingredients in the “laxative tea” consumed by the patient were oolong tea, Tuo tea, Kuding tea, senna leaves, lotus leaves, Cassia seeds, and stevia, none of which were mentioned above. This finding suggested that other traditional Chinese medicines may be associated with IMP[11]. Additionally, some case reports have revealed that adaptive changes in portal hypertension may play an important role in the pathogenesis of IMP, whereas other studies have refuted this notion[12]. In our patient, no evidence supported portal hypertension.
Clinically, IMP often presents latently at first but later develops with symptoms such as abdominal pain, abdominal distension, nausea, vomiting, stool abnormalities and intestinal obstruction[13]. Abdominal pain is the most common symptom reported. However, relatively few cases involve intestinal obstruction[4,13,14]. In our patient, abdominal CT revealed remarkable dilatation and fluid accumulation in the small intestine, indicating intestinal obstruction. The gastrointestinal capsule marker test revealed minimal movement of approximately half of the markers from 24 to 72 hours after intake, indicating a decrease in colon motility. Decreased colonic motility and the intake of a large amount of liquid lead to intestinal obstruction. Given the absence of mechanical factors known to cause intestinal obstruction, pseudointestinal obstruction is considered.
Conservative therapy is recommended over surgical treatment for intestinal obstruction in patients with IMP unless a severe intestinal obstruction cannot be resolved with conservative therapy[15]. In this case, the symptoms of pseudo-obstruction in our patient resolved after conservative therapy without surgery. To date, no cases of colon cancer linked to IMP have been reported, and IMP patients seem to have a relatively good prognosis. However, further studies are needed to elucidate the pathogenesis and prognosis of IMP. Interestingly, the patient was observed to have a bronze complexion for more than ten years, resembling the color of her intestinal mucosa, but this particular change has rarely been reported. Whether facial changes are related to IMP is currently unclear.
Widespread venous sclerosing colitis can decrease intestinal motility, causing intestinal obstruction, particularly after excessive water intake. Owing to the extremely low incidence of IMP and the absence of symptoms in the early stages, it is often misdiagnosed. Thus, clinicians should consider the possibility of IMP in patients who present with intestinal obstruction and have a history of long-term Chinese herbal medicine use. Clinicians should be vigilant in recognizing the specific imaging and colonoscopy characteristics, as these characteristics can facilitate an early and accurate diagnosis.
We thank the Department of Pathology, Aerospace Center Hospital for their guidance of detailed interpretation of the pathological aspects of this case.
| 1. | Koyama N, Koyama H, Hanajima T. A case of right-sided constrictive ischemic colitis presenting with a chronic course. Stom Intest. 1991;26:455-460. |
| 2. | Iwashita A, Yao T, Schlemper RJ, Kuwano Y, Yao T, Iida M, Matsumoto T, Kikuchi M. Mesenteric phlebosclerosis: a new disease entity causing ischemic colitis. Dis Colon Rectum. 2003;46:209-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 28] [Reference Citation Analysis (0)] |
| 3. | Ding J, Zhang W, Wang L, Zhu Z, Wang J, Ma J. Idiopathic mesenteric phlebosclerosis: clinical and CT imaging characteristics. Quant Imaging Med Surg. 2021;11:763-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Shimizu S, Kobayashi T, Tomioka H, Ohtsu K, Matsui T, Hibi T. Involvement of herbal medicine as a cause of mesenteric phlebosclerosis: results from a large-scale nationwide survey. J Gastroenterol. 2017;52:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Shimada Y. Adverse Effects of Kampo Medicines. Intern Med. 2022;61:29-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 6. | Wen Y, Chen YW, Meng AH, Zhao M, Fang SH, Ma YQ. Idiopathic mesenteric phlebosclerosis associated with long-term oral intake of geniposide. World J Gastroenterol. 2021;27:3097-3108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Hiramatsu K, Sakata H, Horita Y, Orita N, Kida A, Mizukami A, Miyazawa M, Hirai S, Shimatani A, Matsuda K, Matsuda M, Ogino H, Fujinaga H, Terada I, Shimizu K, Uchiyama A, Ishizawa S, Abo H, Demachi H, Noda Y. Mesenteric phlebosclerosis associated with long-term oral intake of geniposide, an ingredient of herbal medicine. Aliment Pharmacol Ther. 2012;36:575-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Lu Q, Jiang Y, Mei J, Chen D. Consumption of Acanthopanax gracilistylus wine leads to dark purple intestine. Gastroenterol Nurs. 2023;46:253-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Sze SF, Lam PWY, Lam JTW, Chung CCC, Lee YT. Idiopathic mesenteric phlebosclerosis: A rare cause of chronic diarrhea. JGH Open. 2020;4:769-770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 10. | Young Chuah Y, Yeh Lee Y. Geniposide Causes Idiopathic Mesenteric Phlebosclerosis. Turk J Gastroenterol. 2023;34:890-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 11. | Nagata Y, Watanabe T, Nagasaka K, Yamada M, Murai M, Takeuchi S, Murase M, Yazaki T, Murase T, Komatsu K, Kaizuka M, Sano M, Asano K, Ando C, Taniuchi N. Total dosage of gardenia fruit used by patients with mesenteric phlebosclerosis. BMC Complement Altern Med. 2016;16:207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Chen MT, Yu SL, Yang TH. A case of phlebosclerotic colitis with involvement of the entire colon. Chang Gung Med J. 2010;33:581-585. [PubMed] |
| 13. | Chou JW, Chang CH, Wu YH, Chang KC, Cheng KS, Huang PJ. Idiopathic Mesenteric Phlebosclerosis: A Single-Institute Experience in Taiwan. Turk J Gastroenterol. 2023;34:483-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (1)] |
| 14. | Shan J, Chen F, Yu P. Intestinal obstruction due to idiopathic mesenteric phlebosclerosis colitis: A case report. Front Surg. 2022;9:969154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 15. | Sakurai Y, Watanabe K, Hayashi T, Sato K, Sugano I. Widespread mesenteric phlebosclerosis presenting as intestinal obstruction due to stenosis of the right-sided colon. Clin J Gastroenterol. 2022;15:717-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/