Published online Sep 6, 2025. doi: 10.12998/wjcc.v13.i25.104134
Revised: March 4, 2025
Accepted: May 24, 2025
Published online: September 6, 2025
Processing time: 200 Days and 20.6 Hours
Occult intraocular foreign bodies (IOFBs) can present with atypical symptoms and clinical signs, making diagnosis challenging. We describe a case of an undetected IOFB that was missed on both computed tomography and B-ultrasound, ulti
A 55-year-old male patient presented to our clinic reporting a one-month history of right ocular discomfort and progressive visual deterioration. The patient had previously received a glaucoma diagnosis at a local healthcare facility. His ocular history included blunt trauma to the affected eye five years prior to presentation. Slit-lamp examination revealed corneal and iris lesions in the right eye. Pupillary dilation facilitated the identification of traumatic lens opacities. Diagnostic imaging modalities, including B-scan ultrasonography and computed tomo
Awareness of IOFBs in individuals who work in high-risk occupations and prompt referral to a retinal surgeon are very important.
Core Tip: Occult intraocular foreign bodies can lead uncommon symptoms and signs. We report a case of an occult intraocular foreign body which computed tomography and B-ultrasound were not detected causing ocular siderosis and secondary glaucoma.
- Citation: Xu LX, Kong YC. Ocular siderosis secondary to occult intraocular foreign body causing secondary glaucoma: A case report. World J Clin Cases 2025; 13(25): 104134
- URL: https://www.wjgnet.com/2307-8960/full/v13/i25/104134.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i25.104134
Occult intraocular foreign bodies (IOFBs) represent a substantial proportion (18%-41%) of penetrating ocular trauma cases[1]. These retained objects significantly elevate the risk of severe ocular sequelae, including endophthalmitis, lens opacification, detachment of retinal tissue, and elevated intraocular pressure (IOP). Prompt identification is crucial in clinical management, as diagnostic oversight may result in irreversible vision loss[2]. We describe a patient who developed siderosis bulbi and secondary glaucoma secondary to an undetected metallic intraocular foreign body. This condition manifests through characteristic iron-induced degenerative changes in ocular tissues. While computed tomography (CT) imaging and ultrasound examinations are generally reliable for IOFB detection, they failed to identify the foreign material in this particular case, creating significant diagnostic difficulties[3,4]. This report highlights the potential for false-negative results in IOFB diagnosis and the catastrophic consequences of missed cases[5]. The patient ultimately achieved favorable visual outcomes following successful surgical extraction of the retained metallic fragment, underscoring the importance of maintaining clinical suspicion even when imaging studies prove inconclusive[6].
A man complaint right eye pain about 5 days.
A 55-year-old construction worker sought evaluation at our facility due to acute visual impairment and discomfort in his right eye.
A 55-year-old male employed in construction sustained an ocular injury five years ago when he noticed a foreign particle entering his right eye. Despite this incident, his visual acuity remained largely unaffected. Initial evaluations at a nearby medical facility, including CT and ultrasonography, revealed no IOFBs. Subsequently, approximately one year before presentation, he became aware of progressive vision deterioration. Upon further assessment at a local clinic, he was diagnosed with cataracts, and repeat imaging via CT showed no evidence of retained foreign material.
The patient reports no significant medical comorbidities, including hypertension, diabetes, or cardiovascular conditions. He also has no known history of transmissible infections or familial genetic abnormalities. Five years ago, he sustained a traumatic ocular injury involving a foreign body entering his right eye.
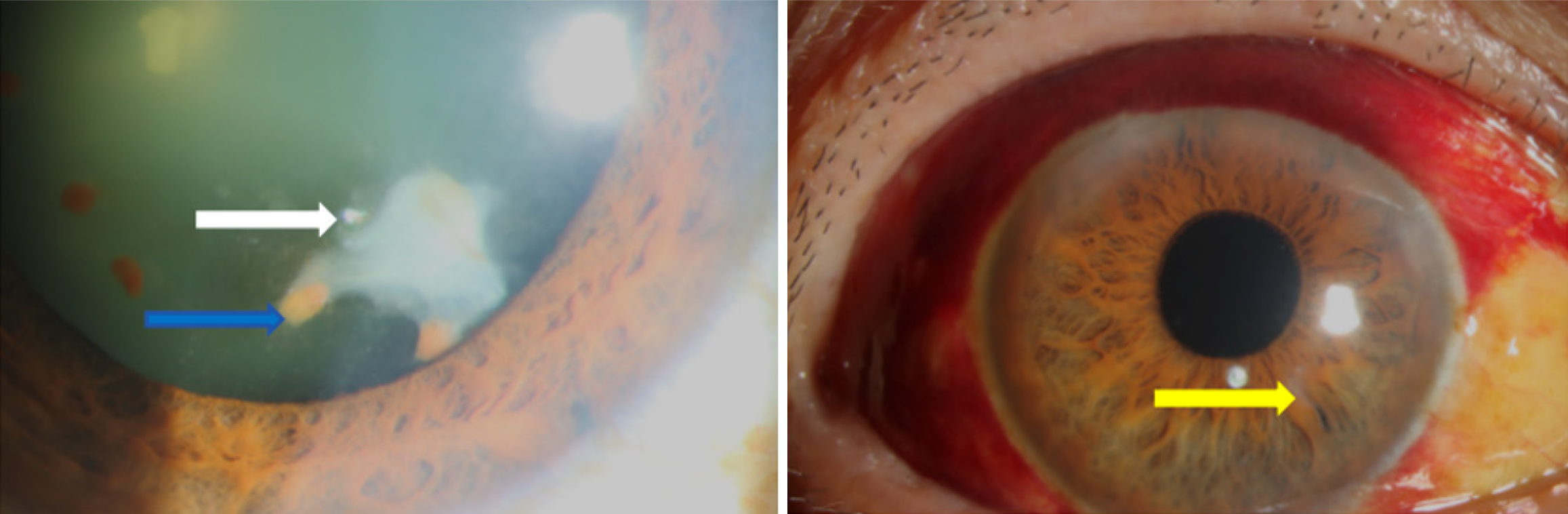
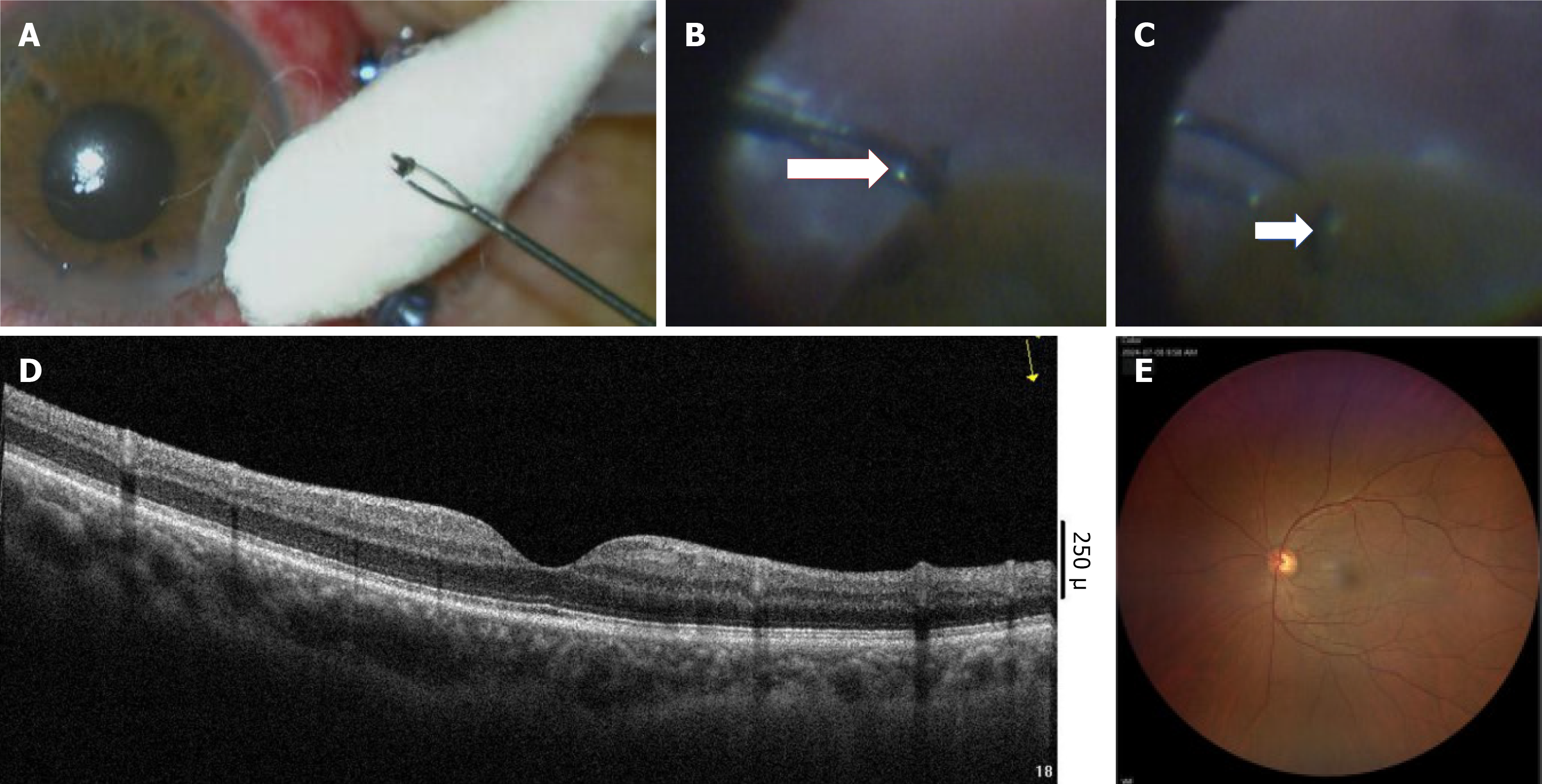
Visual acuity testing demonstrated 20/60 in the right eye and 6/6 in the left. Slit-lamp evaluation of the right eye showed an inferior temporally located oblique corneal scar, which appeared well-healed, along with an adjacent iris defect underlying the scar. The pupil was mydriatic, with a brunescent cataract and pigmented deposits evident on the anterior lens capsule (Figure 1).
IOP was measured at 48 mmHg with a Goldmann applanation tonometer.
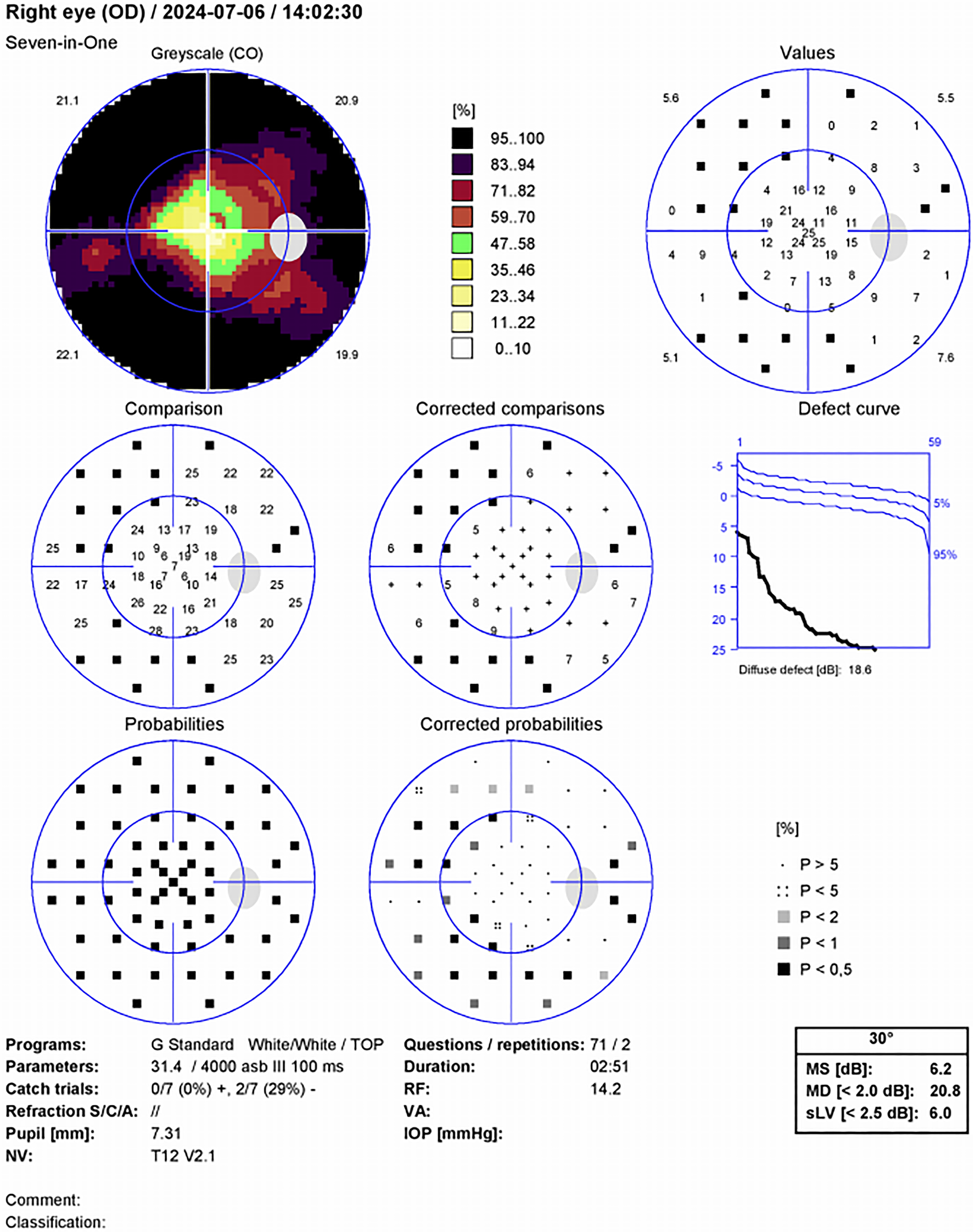
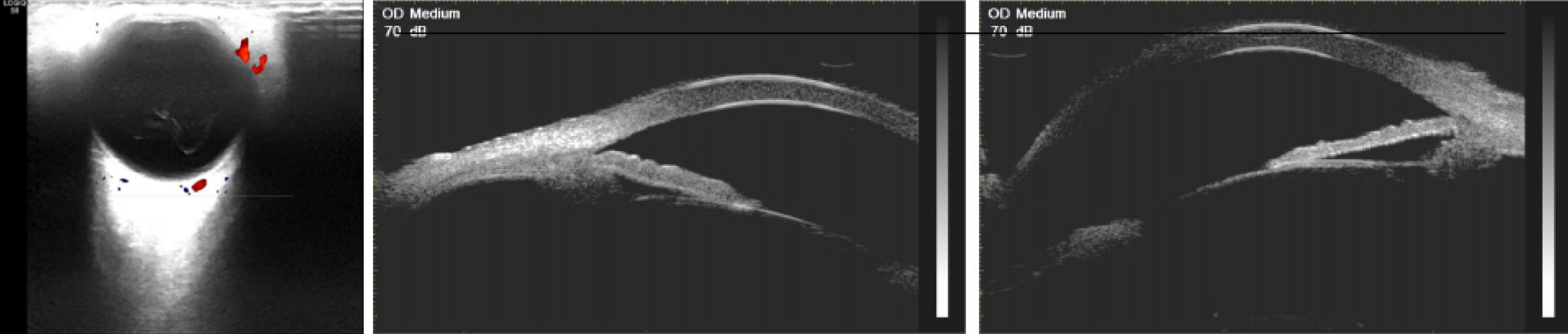
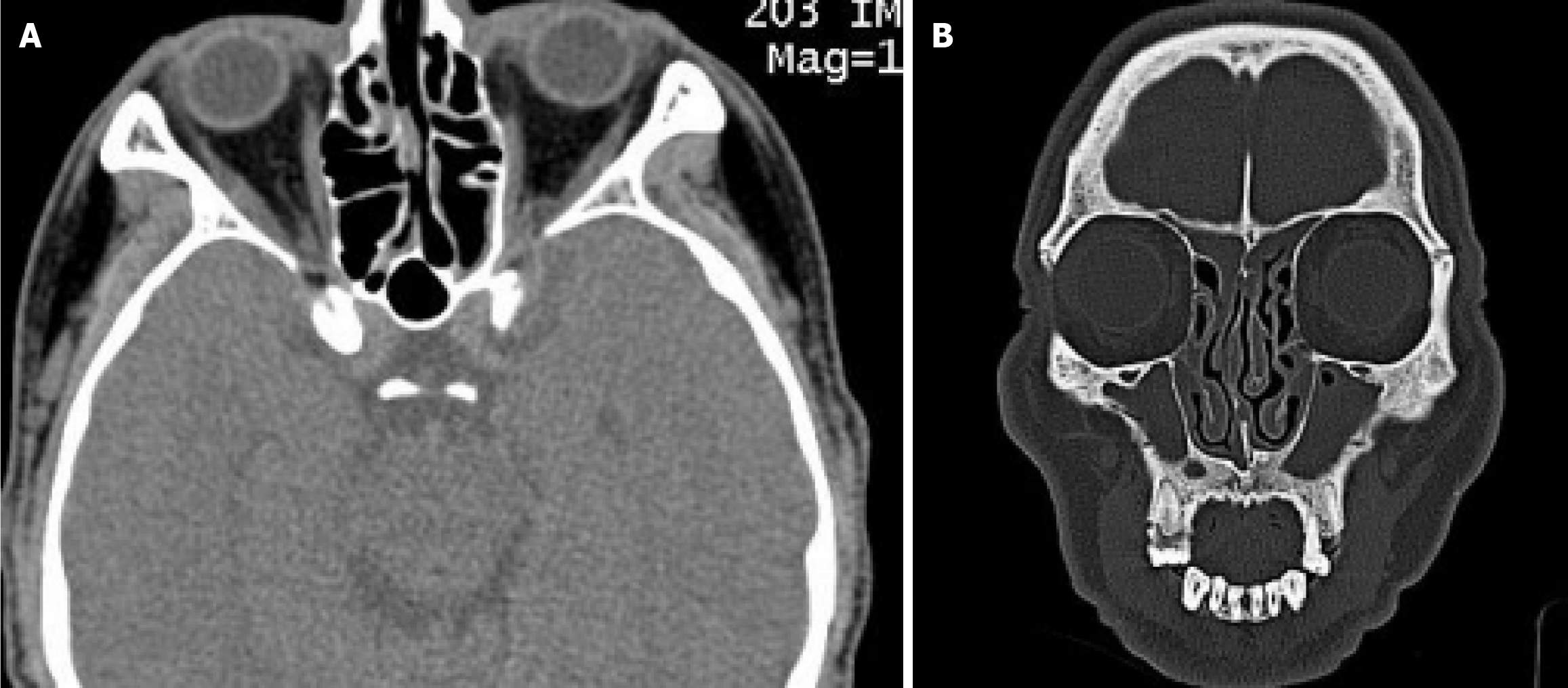
Perimetry demonstrated concentric constriction of the visual field in the right eye (Figure 2). B-scan ultrasonography showed an optically clear vitreous humor with attached retina. Ultrasonic biomicroscopic evaluation meticulously assessed all meridians, with particular attention to the inferotemporal quadrant adjacent to the corneal scar and its contralateral region, but detected no IOFBs (Figure 3). Multiplanar orbital CT imaging (axial, sagittal, and coronal reconstructions) confirmed the absence of radiopaque intraocular foreign material (Figure 4).
Intraocular foreign body, ocular siderosis, secondary glaucoma, cataract, ocular trauma.
Following successful IOP stabilization, the patient underwent phacoemulsification with pars plana vitrectomy. Intraoperative exploration unexpectedly revealed a previously undetected intraocular foreign body, which was carefully extracted (Figure 5). Postoperative management included topical hypotensive medications, maintaining stable pressure at 14 mmHg. Secondary intraocular lens implantation was successfully performed seven days later, with the lens securely positioned within the capsular bag.
Postoperatively, the patient’s IOP was 13 mmHg, and his visual acuity was 50/60.
Siderosis is a distinct clinical entity caused by iron deposition in intraocular tissues, primarily affecting structures such as the iris and lens. Common manifestations include iris heterochromia (58.33%) and cataract formation (95.83%)[7], while retinal pigmentary degeneration occurs in 58.33% of cases[4,7,8].
Siderotic glaucoma, a rare but vision-threatening complication, often results from retained iron IOFBs. We present a case of a 55-year-old man with medically unresponsive secondary open-angle glaucoma, later linked to a self-sealed corneal wound from penetrating trauma five years prior. Despite CT and B-scan ultrasound failing to detect the occult metallic IOFB, clinical findings confirmed siderosis bulbi. Surgical removal of the foreign body normalized IOP and improved vision, underscoring the need for detailed slit-lamp and fundus examinations in trauma cases. Early surgical intervention and long-term monitoring are critical to prevent irreversible vision loss[3].
Retained intraocular iron induces toxicity through oxidative stress, particularly in ectoderm-derived tissues. This process disrupts cellular enzymes, damages membranes, and generates lipid peroxides, culminating in vision loss. Onset varies widely (18 days to decades post-injury)[9,10], and delayed presentation often leads to missed diagnoses. Prognosis depends on the timing of foreign body detection and removal, emphasizing the need for prompt recognition and management to preserve visual function.
Secondary open-angle glaucoma is a frequent complication, developing two months to 30 years post-trauma[11,12]. Proposed mechanisms include: Trabecular meshwork obstruction by iron-laden macrophages or particles, impairing aqueous humor outflow. Albuminous aqueous production by the ciliary body, elevating IOP. Direct iron toxicity, causing trabecular fibrosis and further outflow dysfunction[3,11,12].
While CT is the gold standard for IOFB detection[4], its efficacy depends on scanner resolution, foreign body size, and location. In our case, a 2 mm slice thickness and possible iron dissolution over time likely contributed to the false-negative imaging results. B-scan ultrasound, though useful, is operator-dependent and less reliable for chronic iron IOFBs due to metallic degradation[4,13].
Early IOP monitoring, optic nerve assessment, and visual field testing are vital for at-risk patients. A high index of suspicion, coupled with multimodal imaging and timely intervention, can mitigate vision loss in siderosis-related glaucoma.
In this case, pars plana vitrectomy achieved successful IOFB removal, resolving symptoms and improving visual acuity. This outcome highlights the importance of timely diagnosis and surgical intervention in managing this rare complication. Siderosis bulbi, though uncommon, poses significant vision-threatening risks due to retained iron-containing IOFBs. Early detection and extraction of IOFBs are critical to preventing irreversible ocular damage and preserving visual function[8]. Advanced imaging (CT, B-scans) and electrophysiologic testing enhance diagnostic accuracy and inform treatment strategies. A multidisciplinary approach integrating ophthalmologists, radiologists, and surgeons is essential for optimal patient outcomes. Overall, collaborative care ensures comprehensive evaluation, precise intervention, and long-term monitoring to mitigate complications.
I would like to thank the anesthesiologists and nurses as well as the doctors in the central examining room.
| 1. | Al-Dwairi R, Msallam M. Unilateral Ocular Siderosis Bulbi Due to Missed Metallic Intraocular Foreign Body Masquerading as Anisocoria of Neurological Origin: A Case Report. Am J Case Rep. 2021;22:e930504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 2. | Lapira M, Karl D, Murgatroyd H. Siderosis bulbi as a consequence of a missed intraocular foreign body. BMJ Case Rep. 2014;2014:bcr2013202904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Ballantyne JF. Siderosis bulbi. Br J Ophthalmol. 1954;38:727-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Wu TT, Kung YH, Sheu SJ, Yang CA. Lens siderosis resulting from a tiny missed intralenticular foreign body. J Chin Med Assoc. 2009;72:42-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Koutsonas A, Plange N, Roessler GF, Walter P, Mazinani BA. A case of siderosis bulbi without a radiologically detectable foreign body. Can J Ophthalmol. 2013;48:e9-e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Elgin U, Eranil S, Simsek T, Batman A, Ozdamar Y, Ozkan SS. Siderosis bulbi resulting from an unknown intraocular foreign body. J Trauma. 2008;65:942-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Zhu L, Shen P, Lu H, Du C, Shen J, Gu Y. Ocular Trauma Score in Siderosis Bulbi With Retained Intraocular Foreign Body. Medicine (Baltimore). 2015;94:e1533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Bloom WR, Ramsey JK, Ohr MP. Ocular Siderosis Secondary to Retained Intraocular Foreign Body: A Case Report. Cureus. 2019;11:e4660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Asencio-Duran M, Vázquez-Colomo PC, Armadá-Maresca F, Fonseca-Sandomingo A. [Siderosis bulbi. Clinical presentation of a case of three years from onset]. Arch Soc Esp Oftalmol. 2012;87:182-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Ding J, Yoganathan P, Fernando-Sieminski S. Resolution of siderosis glaucoma from chronic intraocular foreign body without glaucoma surgery. Can J Ophthalmol. 2015;50:e82-e85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Sangermani C, Mora P, Mancini C, Vecchi M, Gandolfi SA. Ultrasound biomicroscopy in two cases of ocular siderosis with secondary glaucoma. Acta Ophthalmol. 2010;88:e1-e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Hope-Ross M, Mahon GJ, Johnston PB. Ocular siderosis. Eye (Lond). 1993;7 (Pt 3):419-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Huang Y, Ye Z, Li Z. Siderotic glaucoma without detectable intraocular foreign body in a pseudophakic eye: a case report. BMC Ophthalmol. 2020;20:417. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/