Published online Jul 26, 2025. doi: 10.12998/wjcc.v13.i21.106413
Revised: March 21, 2025
Accepted: April 3, 2025
Published online: July 26, 2025
Processing time: 61 Days and 2.5 Hours
Epulis fissuratum is an inflammatory fibrous hyperplasia characterized by pseu
A 56-year-old female patient with no significant medical history presented to the dental clinic with tissue over
The multidisciplinary management of epulis fissuratum resulted in precise clinical diagnosis, effective soft tissue management, and appropriate prosthetic adjustments, thereby ensuring favorable long-term outcomes for the patient.
Core Tip: The present clinical case described the multidisciplinary management of a patient with epulis fissuratum developed after 30 years of continuous use of a complete maxillary prosthesis without removal. The treatment was carried out in two phases: Surgical and prosthetic. In the surgical phase, the hyperplastic tissue was removed, and a vestibuloplasty with free gingival graft was performed. The prosthetic phase involved the fabrication of new complete prostheses to restore oral function and aesthetics. The comprehensive treatment, which combined surgical techniques and correct prosthetic rehabilitation, guarantees favorable long-term results.
- Citation: González Gómez LA, Guedea Preciado NE, Martínez Nieto M, Rodríguez Montaño R, Alarcón-Sánchez MA, Torres-Sánchez ED, Gómez Mireles JC, Acevedo Ambriz E, Lomelí Martínez SM. Multidisciplinary treatment of epulis fissuratum: A case report. World J Clin Cases 2025; 13(21): 106413
- URL: https://www.wjgnet.com/2307-8960/full/v13/i21/106413.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i21.106413
Epulis fissuratum (EF) is a condition that manifests as hyperplastic fibrous connective tissue over the soft tissues of the alveolar ridge or vestibular sulcus[1,2]. Typically, it occurs in middle-aged and older adults, with a marked predilection for females. Although it may arise in the maxilla and mandible, studies suggest a higher prevalence in the anterior region of the jaws, with a slight predilection for the maxilla in some populations[1,3]. The lesion often presents clinically as single or multiple folds of hyperplastic tissue that is firm and fibrous to the touch although erythematous or ulcerated forms have also been reported. Although it is typically asymptomatic in the early stages, EF may grow significantly and compromise denture retention and stability with occasional pain or ulceration[4,5]. The lesion is generally non-malignant. However, the differential diagnosis should consider squamous cell carcinoma or other neoplastic conditions especially when unusual clinical features are observed. Diagnosis is primarily clinical, and it is supported by histopathological analysis when necessary[6].
Different treatment modalities are available for EF. These treatments integrate conservative approaches and vary according to the dimensions of the disease and the condition of the patient[3]. Conservative management involves elimi
This case report aimed to describe a detailed procedure used in the multidisciplinary treatment of EF with a focus on its clinical presentation, etiology, diagnostic protocols, and treatment modalities. By integrating evidence-based practices and recent advancements in surgical and prosthetic techniques, this report is expected to guide clinicians in managing this condition effectively. It also illustrated the importance of a patient-centered approach that prioritizes functional and aesthetic rehabilitation while minimizing postoperative complications and recurrence.
A 56-year-old female patient with no significant medical history presented to the dental clinic with tissue overgrowth in the anterior maxilla and depression of the upper lip. She reported 30 years of continuous use of a complete maxillary denture without removal.
The patient mentioned wearing the same maxillary denture continuously without removal for three decades, and she reported progressive tissue changes in the upper jaw.
The patient stated that she had no systemic diseases or significant illnesses in the past and that she was not undergoing any medical treatments at the time of presentation.
No notable familial medical history was reported.
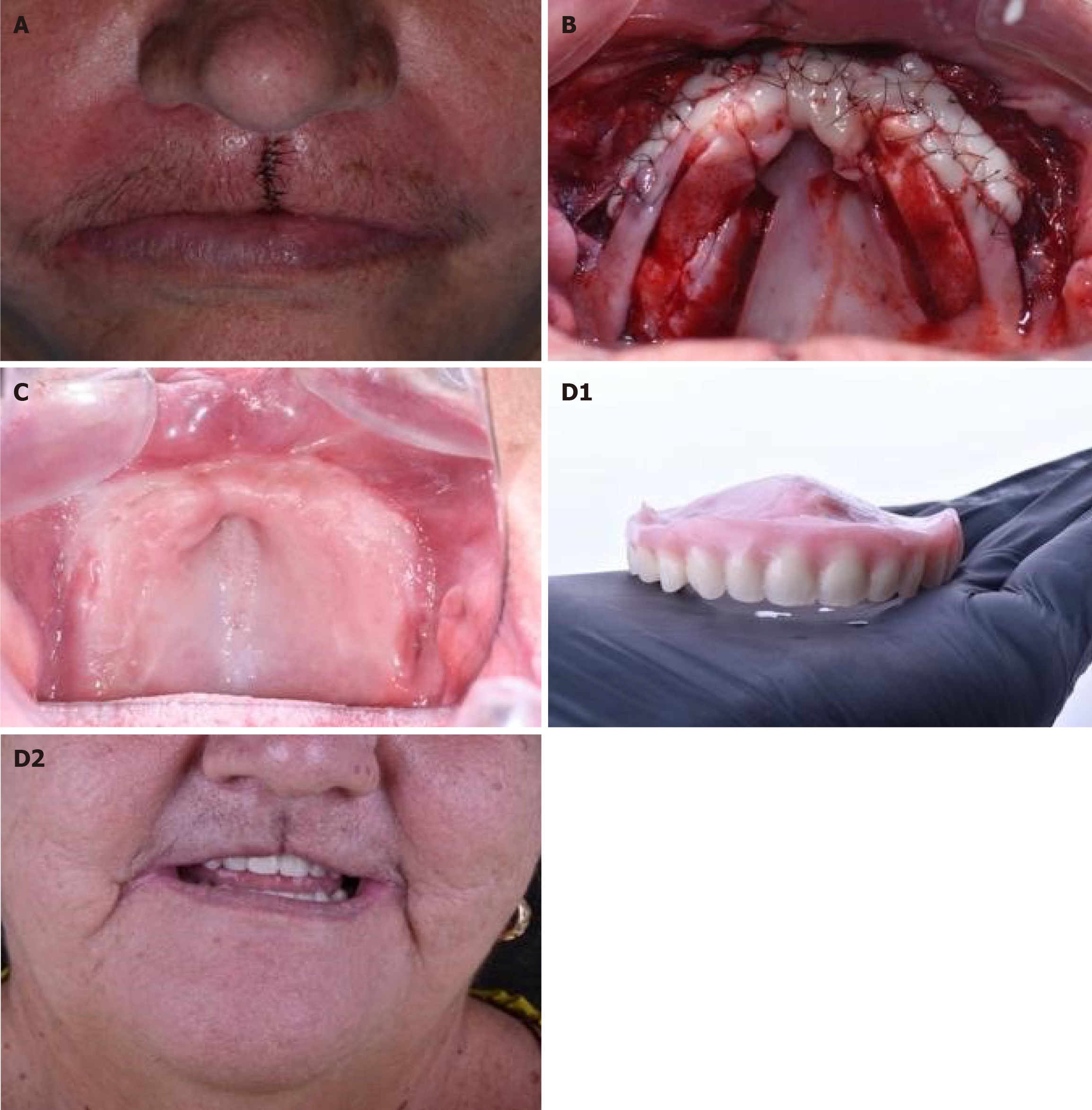
During the clinical examination, a significant tissue overgrowth was observed in the anterior maxillary vestibular area along with a marked depression of the upper lip. The mucosa was hyperplastic, and the non-tender denture appeared ill-fitting and heavily worn (Figure 1).
No laboratory tests were conducted as the patient’s medical history and systemic status did not necessitate them.
Imaging was not performed as the clinical findings were sufficient to guide treatment planning.
An interdisciplinary team of specialists in periodontics and prosthodontics collaborated to devise a treatment plan for the lesion. Given the patient’s extended history of denture use and the severity of tissue changes, a phased approach was used in order to optimize treatment outcomes. The team emphasized the need for surgical intervention so as to correct the soft tissue condition and enhance subsequent prosthetic rehabilitation.
Histopathological analysis confirmed the diagnosis of EF characterized by hyperplastic fibrous tissue caused by chronic irritation from the ill-fitting denture. The specimen revealed a segment of gingival mucosa with squamous epithelium showing acanthosis, irregular hyperkeratosis, and erosion areas. The underlying fibrous stroma exhibited chronic lym
The patient was given prior explanations of the procedures involved in the study, and after obtaining informed consent, the surgical procedures were performed. The first phase began with thorough asepsis and antisepsis. Then, 4% articaine was administered with maxillary block techniques. Using a 15c scalpel blade, the excess fibrous tissue in the anterior vestibular area was carefully excised. Once the gingival tissue was removed, focus was shifted to the upper lip where fibrous tissue was excised resulting in a V-shaped defect. The gingival wound was closed using 4-0 polyglycolic acid sutures with simple interrupted stitches thereby ensuring proper closure of the keratinized gingival tissue and reducing the vestibular depth so as to facilitate primary wound healing. The upper lip was sutured in layers, with the dermis closed using polyglycolic acid sutures, while the epidermis was closed with 6-0 nylon sutures (Figure 2A). Postoperative care involved a regimen of antibiotics and analgesics, with instructions for a follow-up visit and suture removal after 15 days.
The second phase, which was performed 6 weeks later, was aimed at enhancing vestibular depth for improved adaptation of a new complete denture. Following administration of 4% articaine using maxillary block techniques, a partial-thickness flap was created in the anterior maxillary vestibular area. Two free gingival grafts, each approximately 18 mm in length and 5 mm in height, were excised from the hard palate on both sides. Collagen sponges and cross sutures were placed at the donor sites to ensure hemostasis. The grafts were prepared and sutured to form a single composite graft measuring approximately 36 mm in length and 5 mm in height (Figure 2B). This graft was carefully secured in the recipient bed using 6-0 nylon sutures with simple interrupted and cross-stitch techniques. Postoperative care was performed using antibiotics and analgesics as well as a scheduled follow-up appointment 7 days after the procedure. After the last surgical follow-up, appointments were arranged at post-surgery days 7, 15, and 30 so as to evaluate healing, stability of the gingival grafts, and the absence of infection. During each follow-up, mild cleaning was conducted, and various oral hygiene-based recommendations were emphasized. No significant complications such as graft dehiscence and infection were observed.
The prosthetic phase began 3 months following the surgical stage (Figure 2C). The fabrication of a traditional full denture requires a sequence of well-organized clinical and laboratory steps aimed at providing functional and aesthetic prosthetic rehabilitation. Initial impressions were made for the creation of individual trays, and definitive impressions were captured using polyvinylsiloxane. Thereafter, bases and rims were developed in order to establish centric relation and vertical dimension. Then, shade guides tailored to the patient’s age and skin color were utilized to guide selection of acrylic teeth with the most suitable anatomical features. The models were secured in an articulator with the facebow so as to precisely communicate the craniomandibular relationships.
Subsequently, a clinical trial was conducted to assess alignment, phonetics, aesthetics, and stability. Then, the teeth were modified in wax, based on the patient’s aesthetic and functional requirements. The prosthetics were produced with thermocurable acrylic and composite teeth in line with all the documentation. Optimally-fitted prostheses were provided, and occlusal modifications were performed in order to ensure correct operation (Figure 2D). Postoperative guidelines for the initial weeks were discussed and included minimizing solid food intake and rinsing with 0.12% chlorhexidine thereby ensuring a proper hygienic environment for the prosthesis. A follow-up was scheduled 24-48 h later to evaluate pressure points and make necessary adjustments.
After a 5-month follow-up period, optimal healing was evident with adequate tissue integration of the grafts and proper soft tissue restoration. There were no signs of residual inflammation, infection, or associated complications. This reflected the effectiveness of the postoperative measures implemented. Additionally during the follow-up visits, the stability of the grafts and the adaptation of the new prosthesis were assessed so as to corroborate the absence of recurrent hyperplasia or any indication of recurrence of the lesion. The optimal response of the oral tissues and the patient’s adherence to the postoperative measures contributed significantly to these favorable outcomes.
EF is a reactive hyperplastic lesion that arises in response to chronic irritation of the soft tissues of the oral cavity. The etiology, development, and progression of EF are multifactorial, and they are influenced by several local and systemic factors[1]. The local factors comprise poorly fitted dentures, chronic mechanical irritation, nocturnal use of dentures, and inadequate oral hygiene. The primary cause of EF is a poorly-fitted prosthesis due to the fact that the overextended flanks exert continuous pressure on the tissues, thereby generating microtraumas and chronic inflammatory response. Moreover, old prostheses with significant wear are associated with a loss of adaptive capacity[4].
In the present case, it may be suggested that repeated and excessive friction on soft tissues by the prosthesis generated compensatory proliferation of connective and epithelial tissues thereby resulting in the hyperplasia typically associated with the injury[1,6]. Constant use of a prosthesis, particularly at night, reduces the periods of rest for oral tissues and promotes sustained and cumulative damage[4].
The systemic factors associated with the etiology of EF are systemic health conditions (diabetes mellitus, arterial hyper
EF occurs more frequently in elderly patients than in younger patients due to physiological modifications such as decreased keratinized epithelium, which increases susceptibility to prosthesis-induced lesions, and alveolar ridge atrophy[1]. Nutritional deficiencies, particularly inadequate intake of vitamin B complex and vitamin C, compromise the quality and integrity of the oral mucosa, thereby diminishing its capacity to respond to irritation caused by prosthesis[5]. Additionally, behavioral factors, such as smoking and poor prosthetic maintenance without regular check-ups, are associated with the development and progression of EF[1,5]. These systemic factors compromise healing capacity and increase susceptibility to infectious conditions, exacerbate the inflammatory response, and promote tissue proliferation[1,7].
The persistent irritation linked to chronic mechanical trauma on the soft oral tissues of EF induces pathophysiological changes at the cellular and tissue levels. Due to excessive pressure and friction from the flanks of the prosthesis, chronic mechanical irritation generates microtrauma in the oral mucosa, thereby triggering epithelial injury and fibroblast stimulation[2]. Continuous chronic trauma results in inflammation, which is characterized by the release of proinflammatory cytokines such as IL-1 and TNF-α, as well as cellular infiltration along with the presence of lymphocytes and plasma cells in the connective tissue[8,9]. This inflammatory process is linked to a constant irritating stimulus, and it leads to tissue adaptive changes that are manifested as gingival hyperplasia in which the basal cells of the epithelium proliferate excessively and thicken the affected tissue and generating folds. Moreover, fibrous tissue is formed through the accumulation of collagen and elastic fibers by fibroblasts, resulting in a firm and fibrous entity characteristic of the lesion[1,5]. If EF is not managed, the growth of this entity progresses and increases the extent of fibrous tissue and compromises oral function. In some situations this leads to malignant transformations (e.g., squamous cell carcinoma)[6].
Histopathological findings such as acanthosis, irregular hyperkeratosis, and areas of squamous epithelial erosion are indicative of adaptive responses to chronic irritation caused by the poor-fitting prosthesis. Chronic lymphoplasmacytic inflammatory infiltrates in the underlying fibrous stroma were also observed along with congested capillaries and foci of hemorrhage, which may suggest an inflammatory picture with reactive vascular components. Additionally, the presence of fibroblast proliferation and excessive accumulation of collagen and elastic fibers favor the formation of hyperplastic tissue characteristic of EF. This fibrous response and the dense architecture of the analyzed specimen may be attributed to fibroblast activation, most likely by proinflammatory mediators such as IL-1 and TNF-α[1,7]. The histopathological findings indicate adequate differential diagnosis by differentiating EF from other reactive hyperplastic and neoplastic pathologies. Fortunately, the absence of cellular atypia in the histological sections, in addition to the circumscribed nature of the condition, reiterates the benign nature of the case analyzed.
The treatment of EF encompasses various modalities that integrate conservative and surgical approaches. Implemen
Indeed, Widad et al[1] demonstrated that early management of EF with tissue conditioning using provisional prostheses in combination with adequate oral hygiene and proper prosthetic rehabilitation allows for satisfactory clinical results without the need for surgical intervention. In this context, Mohan et al[6] achieved healing of EF by applying analgesics to the affected area in addition to fabrication of a new prosthesis for the patient.
Chronic or extensive lesions require surgical management that is aimed at restoring functional anatomy by removing the fibrous tissue. The techniques for this surgical management involve scalpel excision, electrosurgery, and laser-assisted surgery, each with distinct characteristics. Scalpel excision remains the traditional method and allows for precise removal of fibrous tissue. However, it requires sutures, which leads to longer healing times and loss of vestibule depth. Several vestibuloplasty options such as submucous vestibuloplasty, secondary epithelialization, and vestibuloplasty with free gingival grafts, have been described[4]. The latter option may be performed alongside excision of the EF to restore vestibular depth, create an adequate band of keratinized gingiva, and enhance prosthetic integration. Although auto
In the present clinical case, EF excision in combination with vestibuloplasty using a free gingival graft was performed so as to optimize prosthetic integration by increasing the height of the alveolar ridge and generating an adequate band of keratinized gingiva. Vestibuloplasty expands the support area of the prosthesis, thereby decreasing the load on the prosthesis per square unit of supporting bone and reducing the bone resorption caused by the transfer of occlusal forces. After proper healing, a new prosthesis is fabricated.
This surgical technique is similar to the one successfully applied by Khalifa et al[6] and Ibrahim et al[5]. Laser-assisted surgeries, particularly carbon dioxide lasers, have gained popularity due to their numerous benefits such as a high degree of precision, low postoperative pain, limited scarring, and non-requirement for conventional suturing. They are also able to seal blood vessels, control bleeding, and accelerate healing, thereby reducing the risk of bacterial contamination[3,10].
The selection of a free gingival graft was considered due to its potential to restore the depth of the vestibule and generate an adequate band of keratinized gingiva. This is essential for optimal long-term stability and the prevention of recurrence[5,6]. Although laser-assisted techniques and cryosurgery are characterized by certain significant advantages, they have limitations regarding the depth and extent of the affected tissue. These limitations compromise their effectiveness in clinical cases of extensive fibrous hyperplasia such as the one presented in this study.
In studies by Samir et al[11], de Arruda Paes-Junior et al[8], and Monteiro et al[9], this surgical modality produced favorable results in pre-prosthetic surgery by maintaining the depth of the vestibule necessary for future prosthetic stability. In recent years cryosurgery with liquid nitrogen has also emerged as a promising alternative. This procedure is characterized by excellent hemostasis, minimal edema, and a reduced degree of postoperative pain. However, its implementation is still restricted to particular clinical scenarios such as the case reported by Vyasarayani et al[7].
Thus, there is a need for more extensive studies before validating the use of cryosurgery with liquid nitrogen in the management of EF. Despite being less invasive, the conservative approach tends to be less effective in cases of extensive and fibrous entities, and it requires prolonged treatments[1]. In contrast, the surgical approach compromises prosthetic stability due to its associated side effects such as vestibular shortening and alveolar bone atrophy. In spite of its multiple advantages, the use of lasers is limited by cost considerations and the need for specialized training[1,3].
On the other hand, there is still controversy about balancing prosthetic restoration with the results obtained. Although graft vestibuloplasty increases mucosal quality and prosthetic fit, it may not mitigate the biomechanical challenges of highly resorbed ridges[1,8]. Correct treatment of EF requires a multidisciplinary approach that accounts for the biological and mechanical factors underlying its formation and development. While conservative approaches emphasize soft tissue preservation and patient comfort, surgical approaches are aimed at restoring optimal oral function and stability[8,12,13].
The controversy over the ideal treatment strategy underscores the need for individualized management plan and continued research for the generation of more therapeutic findings and mitigation of existing limitations. The recurrence of EF represents a significant challenge, particularly in cases where etiological factors are not eliminated[1,14,15]. Therefore, recurrence rates are often associated with poor denture fit following surgical or conservative treatment. Indeed, some studies suggest that recurrence is more frequent when sharp, overextended, or poor-fitting prosthetic edges persist and lead to chronic irritation[4]. Thus, the implementation of proper adjustments to existing prostheses or fabrication of new ones, is recommended to guarantee optimal design and eradicate excessive pressure and traumatic contact[1,8,14,15]. Within the same framework, it is essential to promote adequate oral and prosthetic hygiene and to avoid nocturnal use of prostheses as well as to arranging periodic check-ups to assess their condition.
It is essential to establish strategies for preventing the recurrence of EF including patient education and regular follow-up visits. It is necessary to implement instructions on the proper use of dentures by emphasizing the need to avoid using them at night and oral hygiene guidelines to reduce the risk of chronic soft tissue irritation. Moreover, there is a need to design a personalized follow-up protocol that may include scheduled check-ups at postoperative weeks 2, 4, and 12 to carry out clinical evaluations aimed at identifying early signs of recurrence and making necessary prosthetic adjustments. Long-term periodic check-ups are relevant not only for analyzing the conditions of oral tissues but also for reinforcing preventive recommendations and motivating the maintenance of effective self-care practices.
The main challenge in the present study was its single-case design, which limited the generalization of the findings to a broader population. Despite the detailed approach that provides valuable clinical perspectives on the multidisciplinary management of EF, it is imperative to emphasize that the findings should be interpreted with caution. Consequently, further studies with more robust designs such as prospective controlled trials or case series, are needed for the validation of the therapeutic interventions described here. We suggest future lines of research based on comparative evaluation of various surgical modalities (free gingival grafting, laser-assisted surgery, and cryosurgery) using a representative sample. The research should entail detailed analysis not only of the immediate clinical results but also long-term recurrence rates. Within this framework, we consider it relevant to study the impact of ongoing educational programs and personalized follow-up consultations on the reduction of recurrence of EF.
Multidisciplinary treatment of EF is essential for ensuring favorable long-term results. The present study illustrated how a comprehensive approach that combines surgical removal of tissue with vestibuloplasty using a free gingival graft and subsequent adequate hyperplastic prosthetic rehabilitation not only restored oral function and esthetics but also decreased the risk of EF recurrence. Furthermore, it is crucial to identify and correct etiological factors (e.g., poor-fitting prostheses) to prevent future complications. Periodic check-up appointments, oral hygiene maintenance, and proper prosthesis adaptation are essential pillars in the follow-up of EF treatment. This comprehensive approach addresses the oral health and quality of life of the patient with EF by establishing an efficient, adequate, and sustainable clinical mana
| 1. | Widad EG, Nadia M, Jihane SH. Prosthetic management of an epulis fissuratum with simple conditioning tissue: A case report. Int J Surg Case Rep. 2024;122:110130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Chybicki D, Słowik M, Torbicka G, Białkowska-Głowacka J, Janas-Naze A. Dental implant displacement complicated by epulis fissuratum and extraoral fistula in a patient with senile dementia of Alzheimer's type. Clin Case Rep. 2021;9:e04440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Karimi A, Sobouti F, Torabi S, Bakhshandehfard A, Amirian A, Shariati M, Morshedi E, Barati M. Comparison of Carbon Dioxide Laser With Surgical Blade for Removal of Epulis Fissuratum. A Randomized Clinical Trial. J Lasers Med Sci. 2016;7:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Khalifa C, Bouguezzi A, Sioud S, Hentati H, Selmi J. An innovative technique to treat epulis fissuratum: A case report. SAGE Open Med Case Rep. 2021;9:2050313X211063135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Ibrahim AH, Merzouk N, Abdelkoui A. Prosthetic and surgical management of a sizeable epulis fissuratum: a case report. Pan Afr Med J. 2022;41:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Mohan RP, Verma S, Singh U, Agarwal N. Epulis fissuratum: consequence of ill-fitting prosthesis. BMJ Case Rep. 2013;2013:bcr2013200054. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Vyasarayani P, Madhumietha A, Gundlapalle P. Management of geriatric patient with epulis fissuratum using liquid nitrogen cryosurgery: a case report. J Indian Prosthodont Soc. 2014;14:115-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | de Arruda Paes-Junior TJ, Cavalcanti SC, Nascimento DF, Saavedra Gde S, Kimpara ET, Borges AL, Niccoli-Filho W, Komori PC. CO(2) Laser Surgery and Prosthetic Management for the Treatment of Epulis Fissuratum. ISRN Dent. 2011;2011:282361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Monteiro LS, Mouzinho J, Azevedo A, Câmara MI, Martins MA, La Fuente JM. Treatment of epulis fissuratum with carbon dioxide laser in a patient with antithrombotic medication. Braz Dent J. 2012;23:77-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Eroglu CN, Tunç SK, Elasan S. Removal of epulis fissuratum by Er,Cr:YSGG laser in comparison with the conventional method. Photomed Laser Surg. 2015;33:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Samir ER, Hasnae R, Oumkeltoum E. Diode laser surgery for the treatment of denture-induced fibrous hyperplasia: a case report. Pan Afr Med J. 2024;47:105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Hasnaoui JS, Stri Z, Chkoura A, Sefrioui A, Merzouk N. Key Steps to Optimize Management of Epulis Fissuratum induced by a Total Denture: A Case Report. Asian Pac J Health Sci. 2017;4:213-219. [DOI] [Full Text] |
| 13. | El Assraoui K, Oubbaih A, Kaoun K, Bellemkhannate S. Management of Denture-induced Hyperplasia. Eur J Dent Oral Health. 2023;4:23-26. [DOI] [Full Text] |
| 14. | Sharma S, Ravi Kiran S, Shankar R. Rehabilitation of Flabby Ridges for Denture Fabrication: An Enigma for Dental Professionals. Cureus. 2024;16:e62345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Ozdede M, Dere KA. Ascher Syndrome: Acquired Double Lower Lip Combined With Epulis Fissuratum. J Craniofac Surg. 2020;31:e563-e565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/