Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.103729
Revised: February 21, 2025
Accepted: February 25, 2025
Published online: July 16, 2025
Processing time: 132 Days and 1.8 Hours
Clinical bladder evaluation is a cost-effective, non-invasive method for diagnosing and managing urinary dysfunction, particularly in patients with neurogenic bladder or other impairments. This process aims to assess bladder capacity, sto
Core Tip: Clinical bladder evaluation is a cost-effective, non-invasive, and practical method for diagnosing and managing urinary dysfunction, particularly in low-resource settings. It avoids instrumentation-related risks, aligns with real-life patient conditions, and provides essential insights into bladder function, enabling tailored management strategies like self-catheterization, fluid intake adjustment, and use of bladder diaries. This approach is especially beneficial for patients with neurogenic bladder or those in economically disadvantaged regions, offering a feasible alternative to urodynamic studies.
- Citation: Swarnakar R, Yadav SL. Clinical bladder evaluation: A new, cost-effective, clinical method for neurogenic bladder evaluation and rehabilitation. World J Clin Cases 2025; 13(20): 103729
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/103729.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.103729
Clinical bladder evaluation is a clinical procedure in diagnosing and managing urinary dysfunction, particularly in patients with neurogenic or other forms of bladder impairment. This assessment aims to understand the bladder's capacity, storage, and voiding functions, enabling healthcare providers to identify underlying abnormalities and tailor management strategies. The evaluation often involves a series of steps, including monitoring urine leaks, assessing post-void residual (PVR), and measuring total bladder capacity. These steps help differentiate between types of bladder dysfunction, such as upper motor neuron (UMN) and lower motor neuron (LMN) bladder, each with distinct characteristics and management requirements. By providing insights into the bladder's behavior during storage and voiding phases, clinical bladder evaluation plays a vital role in preventing complications such as urinary tract infections, kidney damage, and incontinence, while also improving the patient’s quality of life through individualized treatment planning. We have described it steps by steps. It starts from history taking to final interpretation.
Relevant history should be taken: (1) Age; (2) Sex; (3) Illness type and duration; (4) Fluid intake; (5) Urine output; (6) History of any co-morbidities; (7) Surgical history; (8) Medication history; (9) History of tobacco/alcohol use or other additions; and (10) How activities of daily living getting affected by current illness. Assessment of symptoms including details of urinary incontinence, urgency, frequency, retention, and nocturia should be done.
Complete neurological, musculoskeletal examination and genitourinary examination (local and systemic) including abdominal examination need to be done systematically.
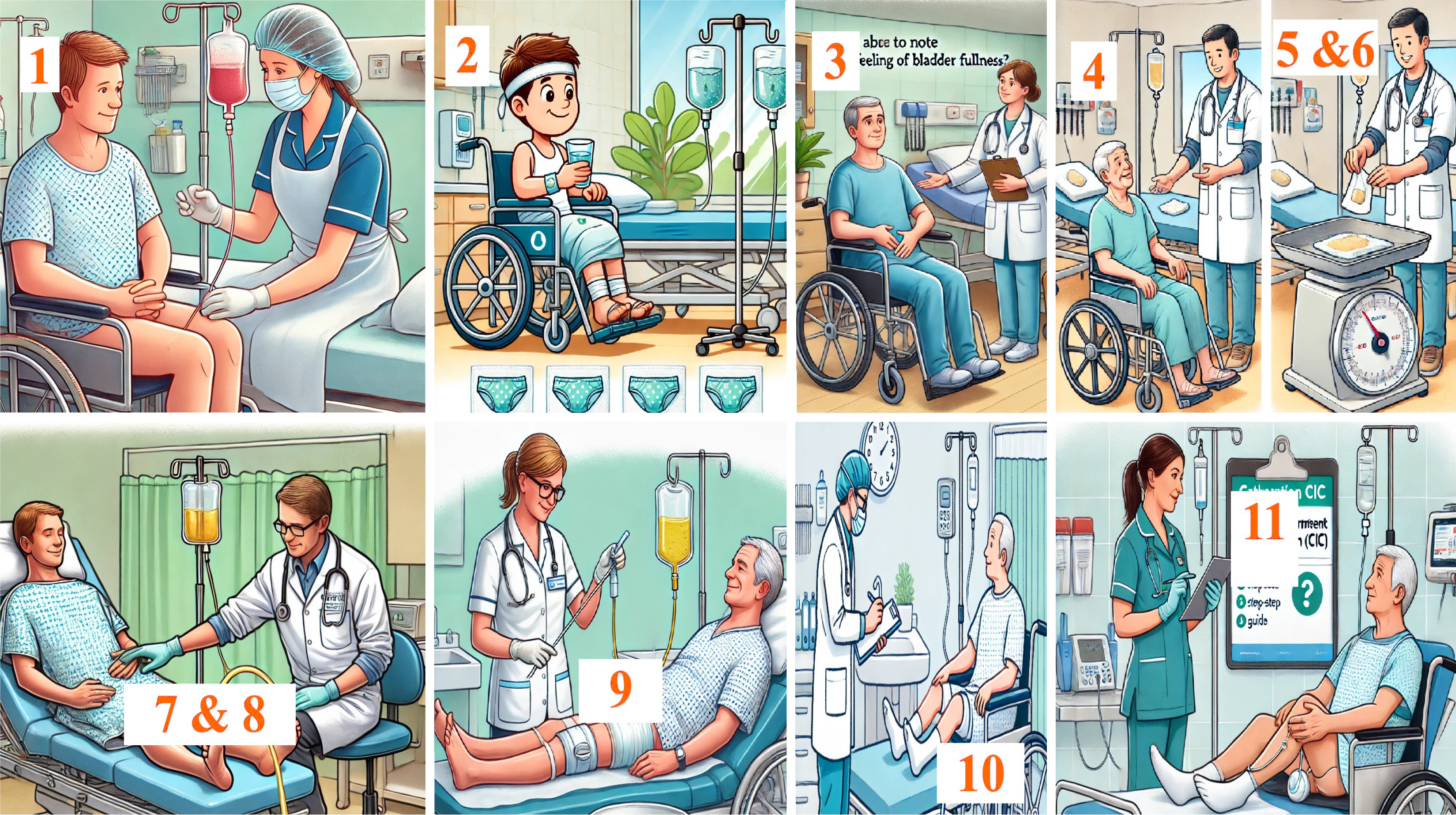
A good explanation, counselling and written informed consent regarding procedure are the most important steps before commencing the evaluation process (Figure 1, Table 1)[1,2].
| STEPS (note time and amount) | Explanation | |
| 1 | Removal of catheter/make empty the bladder | Starting of procedure to get an emptied bladder |
| 2 | Ask to take water as he/she usually takes it at home. Give multiple gauge pieces near genitalia to hold leaks of urine | Water intake varies among individuals, patient’s water intake at home would reflect his daily life and would give a better idea of leakage and further management |
| 3 | Ask to note the feeling of bladder fullness (if any) | Some may have a feeling of fullness as in normal bladder, which would help in better management in terms of the timing of self-CIC |
| 4 | Ask to note any leaks (numbers, amount and time) | Gives an idea on upper motor neuron vs lower motor neuron bladder and further management. First leak time gives idea about holding time |
| 5 | Weighing dry and wet gauge pieces/pad | To get an idea about volume of leaked urine |
| 6 | Weighing soaked gauge pieces (equivalent to urine volume, mg to mL) | Calculate urine volume after conversion = (weight soaked–weight of dry gauges) |
| 7 | Apply stimulus to lower abdomen (reflex voiding) and measure leaks of urine | Calculate reflex voiding |
| 8 | Ask to self-void, measure amount | Check self-voiding (voluntary efforts) |
| 9 | Catheterize the bladder (PVR) | Check PVR, transurethral catheterization is the gold standard for PVR measurements |
| 10 | Calculate total bladder capacity | All leaks + reflex voiding + self-voiding + PVR |
| 11 | Check eligibility of self- CIC | Decision making and planning for further management |
After a clinical bladder assessment, the interpretation focuses on key parameters to guide diagnosis and management. First, the type of bladder dysfunction is identified—whether it is an UMN or LMN bladder. UMN bladder is typically spastic with overactive detrusor muscles, leading to reflex voiding and frequent, small leaks, while LMN bladder is flaccid and underactive, often resulting in overflow incontinence and absent reflex voiding. Next, the timing and amount of urine leaks provide insight into bladder compliance and capacity, with early leaks suggesting reduced capacity and late leaks indicating better compliance but potentially poor control. Reflex voiding, if present, highlights detrusor reflex activity commonly seen in UMN dysfunction and may guide reflex-based management strategies.
The total bladder capacity, calculated as the sum of all leaked urine, reflex voiding, self-voided urine, and PVR, provides a comprehensive measure of bladder storage and emptying ability. Reduced capacity often points to poor bladder compliance or overactivity, while normal or high capacity with significant retention suggests underactivity or overflow issues. PVR estimation is particularly crucial for assessing voiding efficiency; high PVR volumes (> 100 mL) indicate incomplete emptying. These findings collectively help tailor interventions such as timed voiding, medications, self-clean intermittent catheterization (CIC), or surgical options, ensuring effective management and prevention of complications like infections or renal damage.
It helps in advising the self-CIC, and its timings per day. It also assists in adjustment with fluid intake to control the time and amount of leakage. Furthermore it helps in advising the bladder diary: (1) The times of micturition and voided volumes; (2) Incontinence episodes; (3) Pad usage; and (4) Other information such as fluid intake, the degree of urgency, and the degree of incontinence.
It includes (1) No cost at govt. set up; (2) Lowest cost at any set-up compared to urodynamics[3]; (3) It is good in low resource settings, developing country or in primary health care settings; (4) No risk of instrumentation and antibiotic prophylaxis as required for urodynamics; and (5) More realistic in terms of the patient’s goal (corroborate to the real-life situation) and management.
In underdeveloped areas, structured training of these methods are essential steps. But these would be easy for even general physicians and nursing personnel. Furthermore, future research is needed to validate and compare these steps with findings of urodynamics for better reliability across diverse patient populations.
There is no specific study on clinical bladder assessment. No validation study exists as well. Maximum voided volume is defined as the highest voided volume recorded from the frequency-volume chart measured continuously for 72 hours and it is the most accurate measure of bladder capacity compared with maximum cystometric capacity measured by urodynamic study (UDS)[4]. There are few situations where UDS is not found reliable[5].
Considering the context of low economic backgrounds, the need to avoid instrumentation-related side effects, and the preference for simple, non-invasive assessment methods, clinical bladder evaluation serves as an effective approach for understanding bladder function and guiding further management.
This clinical method for bladder evaluation provides a cost-effective and accessible alternative for neurogenic bladder management, particularly in underdeveloped regions or where urodynamic studies are unavailable. It offers practical steps for assessing bladder function and guiding rehabilitation strategies tailored to individual needs. Further validation through comparative studies and real-world applications is essential to establish its clinical efficacy and broader adoption.
| 1. | Weatherall M, Harwood M. The accuracy of clinical assessment of bladder volume. Arch Phys Med Rehabil. 2002;83:1300-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Asimakopoulos AD, De Nunzio C, Kocjancic E, Tubaro A, Rosier PF, Finazzi-Agrò E. Measurement of post-void residual urine. Neurourol Urodyn. 2016;35:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Lewis AL, Young GJ, Selman LE, Rice C, Clement C, Ochieng CA, Abrams P, Blair PS, Chapple C, Glazener CM, Horwood J, McGrath JS, Noble S, Taylor GT, Lane JA, Drake MJ. Urodynamics tests for the diagnosis and management of bladder outlet obstruction in men: the UPSTREAM non-inferiority RCT. Health Technol Assess. 2020;24:1-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 4. | Kim MH, Suh J, Kong HJ, Oh SJ. Maximum Voided Volume Is a Better Clinical Parameter for Bladder Capacity Than Maximum Cystometric Capacity in Patients With Lower Urinary Tract Symptoms/Benign Prostatic Hyperplasia: A Prospective Cohort Study. Int Neurourol J. 2022;26:317-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Rodrigues P, Hering F, Cielici E, D Império M. False-negative finding in urodynamic study for the chief complaint. Does it interfere with the clinical outcomes for the treatment of SUI or OAB syndromes? Int Braz J Urol. 2021;47:551-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/