Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.100714
Revised: February 18, 2025
Accepted: March 20, 2025
Published online: July 16, 2025
Processing time: 225 Days and 19.7 Hours
Carriers of chromosomal balanced translocations are often physically healthy with no obvious developmental problems. However, potential chromosomal imbalance in their gametes can lead to implantation failure, miscarriage, or the birth of a child with a chromosomal abnormality.
We report six cases of chromosomal translocations involving three families, including the specific Robertson (Roche) translocation. Case 1: The karyotype of the proband was 46, XX, t(18;19)(q22;p12). Case 2: Interventional prenatal diagno
Carriers of chromosomal translocations have a high risk of adverse pregnancy outcomes, though they can still have normal offspring. This report on six cases of chromosomal translocations from three families could serve as a reference for future prenatal diagnosis of chro
Core Tip: This paper reports six cases of chromosomal translocations involving three families, including a specific Robertson (Roche) translocation. None of the probands in the three families had an obvious abnormal phenotype. However, they all had varying degrees of chromosomal translocations, including balanced translocations in families 1 and 2 and a Roche translocation in family 3. Additionally, their fetuses did not have any apparent abnormalities postnatally. This case report of six chromosomal translocations in three families will serve as a reference for future prenatal diagnosis of chromosomal translocations and decision-making on whether to continue the pregnancy.
- Citation: Kan X, Xie YX, Yao L, Wang LY, Xia YX, Sun JQ, Bian ML, Yu L, Lu YL. Prenatal diagnosis of balanced translocation from three families: Six case reports. World J Clin Cases 2025; 13(20): 100714
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/100714.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.100714
Chromosomal balanced translocations and Robertson (Roche) translocations are two common types of chromosomal structural abnormalities. They often have no phenotypic abnormality because there is usually no addition or loss of genetic material, or only loss of part of the heterochromatin. However, during the meiotic division of germ cells, unbalanced rearrangements of gametes can occur, leading to infertility, spontaneous abortion, and stillbirth[1]. Therefore, having chromosomal translocations is an important indication for prenatal diagnosis. In this study, we retrospectively analyzed six cases of chromosomal translocations across three families, discussing their prenatal diagnostic outcomes and providing references for future decisions on whether to continue pregnancies with chromosomal translocations.
Case 1: Family 1, Proband, 29 years old, female.
Case 2: Family 1, Fetus at 18 weeks of gestation.
Case 3: Family 2, Proband, 48 years old, male.
Case 4: Family 2, Fetus at 14+6 weeks of gestation.
Case 5: Family 3, Proband, 31 years old, male.
Case 6: Family 3, Fetus at 19+4 weeks of gestation.
Case 1: In family 1, the proband had a previous pregnancy but with no live birth.
Case 2: In family 1, Fetus at 18 weeks of gestation.
Case 3: In family 2, the wife of the proband had six pregnancies, zero abortions, two spontaneous abortions, one induced abortion, and two mid-term induced abortions (cause of induced labor: Unbalanced translocation of fetal chromosomes).
Case 4: In Family 2, Fetus at 14+6 weeks of gestation.
Case 5: In family 3, the wife of the proband had two pregnancies, resulting in zero births and one spontaneous abortion.
Case 6: In Family 3, Fetus at 19+4 weeks of gestation.
All three couples were well-developed and phenotypically normal, with no consanguineous marriage and no history of exposure to drugs, poisons, and radiation during pregnancy.
All three couples denied any family history of malignancy.
The physical examination of the three couples was normal.
Laboratory tests for these three couples showed no abnormalities.
Case 1: In family 1, the ultrasonography revealed appropriate fetal growth.
Case 2: In family 1, Fetus of case 1, with imaging findings identical to those of case 1.
Case 3: In family 2, the wife of the proband underwent ultrasonography at 20 weeks of gestation, which revealed an intrauterine pregnancy with a single viable fetus (ultrasound gestational age of 20 weeks and one day) and no echo in the fetal intracranial cavity (verga cavity? Arachnoid cysts to be excreted).
Case 4: In family 2, Fetus of the wife in case 3, with imaging findings identical to those of the wife in case 3.
Case 5: In family 3, the wife of the ultrasonography revealed appropriate fetal growth.
Case 6: In family 5, Fetus of the wife in case 5, with imaging findings identical to those of the wife in case 5.
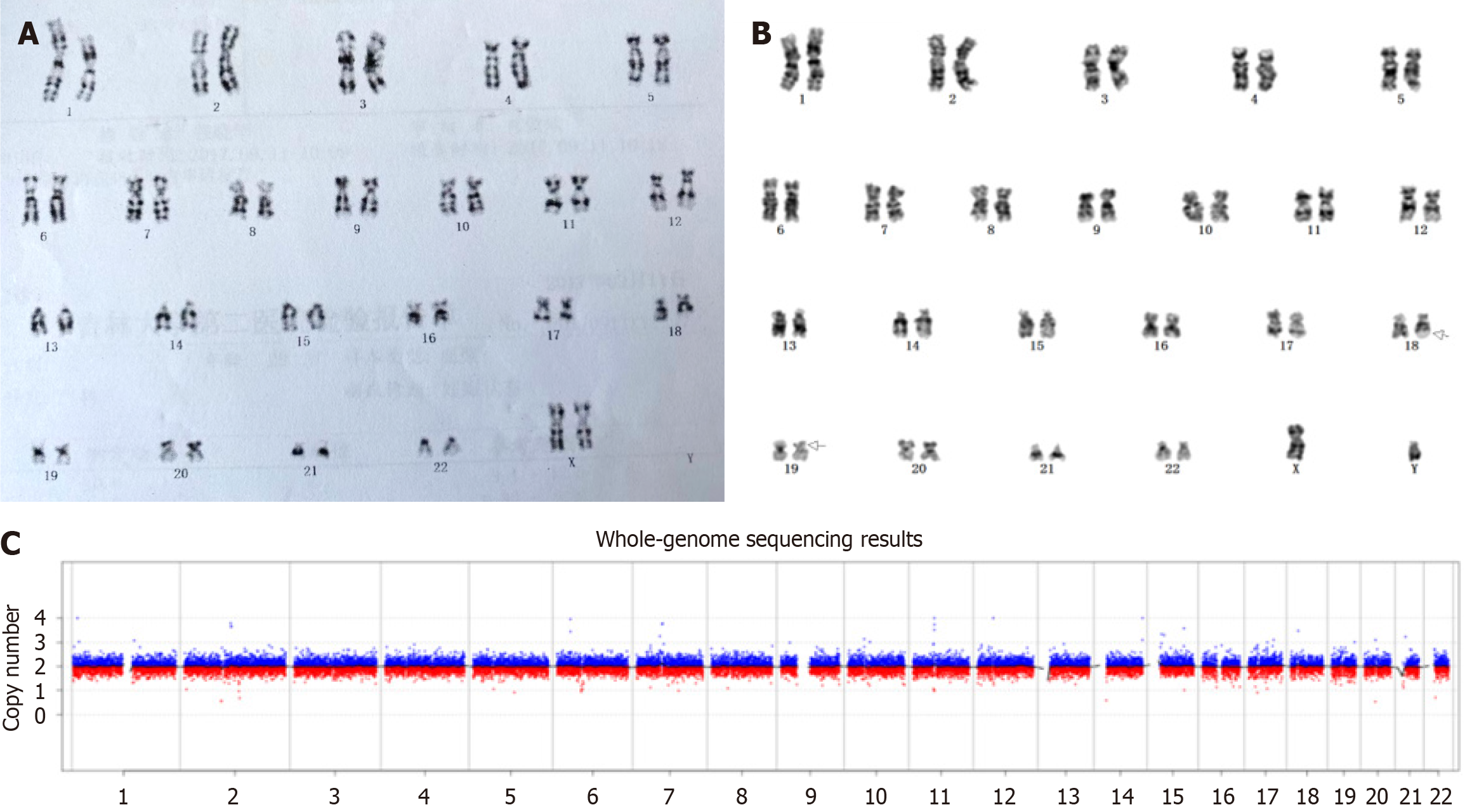
In family 1, the chromosome karyotype of the proband was 46, XX, t(18;19)(q22;p12) (Figure 1A), and that of the husband was normal. At 18 weeks of gestation, the proband underwent interventional prenatal diagnosis at our hospital. Amniotic fluid (30 mL) was collected, of which 20 mL was used for routine cell culture, slide preparation, and chromosome G-banding karyotype analysis, as described in the ISCN 2016 guidelines. The fetal karyotype was 46, XY, t(18;19)(q22;p12) (Figure 1B), identical to that of the proband. The remaining 10 mL of amniotic fluid was used for copy number variation (CNV) analysis, and no abnormalities were detected (Figure 1C).
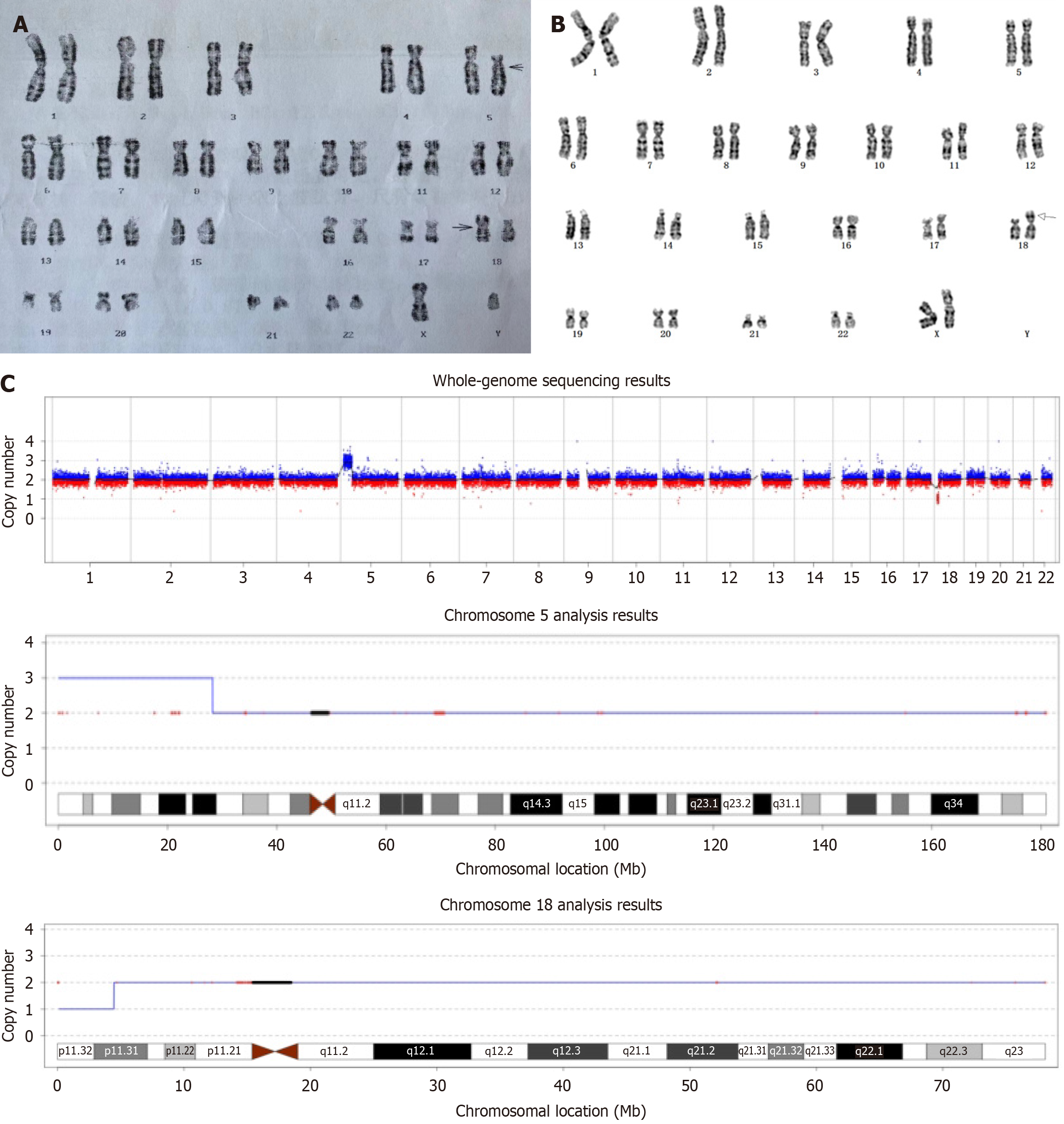
In family 2, the proband’s routine semen examination was normal. The chromosomal
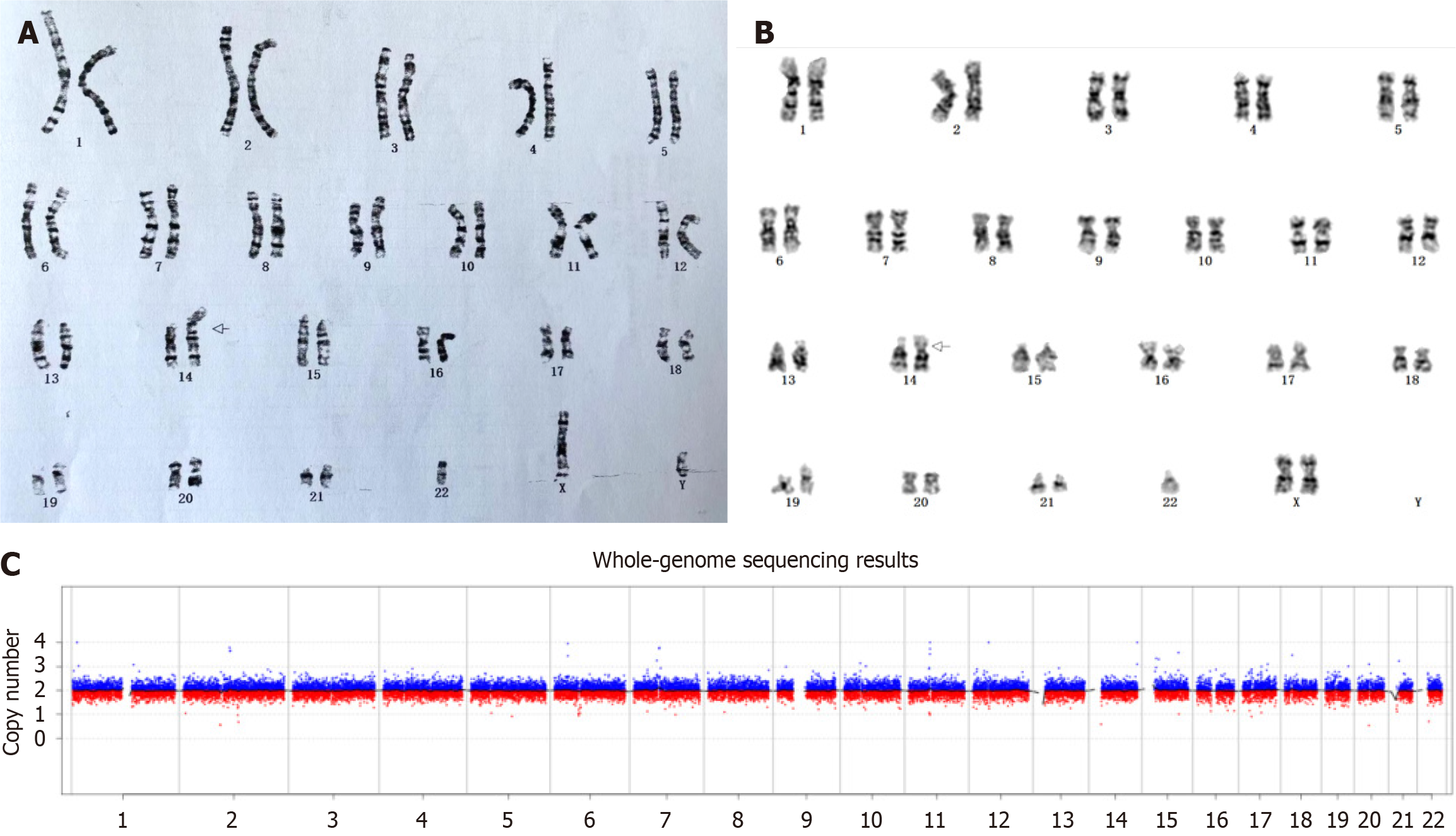
In family 3, the proband’s routine semen examination was normal. The chromosomal karyotype of the proband was 45, XY, der(14;22)(q10;q10) (Figure 3A), while the chromosome karyotype of his wife was normal. At 19+4 weeks of gestation, the proband’s wife underwent interventional prenatal diagnosis at our hospital. Routine amniotic fluid cell culture and G-banding karyotype analysis were performed. The fetal karyotype was 45, XX, rob(14;22)(q10;q10) (Figure 3B). The CNVs test results suggested no significant abnormalities (Figure 3C).
Treatment is as follows: (1) Case 1 and case 2: Continuation of pregnancy; (2) Case 3 and case 4: Termination of preg
In family 1, the proband gave birth to a male infant weighing 3350 g and measuring 50 cm in length. The 1-minute Apgar score was 10, and no apparent physical abnormalities were observed.
In family 2, the couple decided to terminate the pregnancy and delivered a baby girl weighing 900 g with no apparent abnormalities.
In family 3, the proband’s wife gave birth to a baby girl weighing 3230 g and measuring 50 cm in length. The 1-minute Apgar score was 10, and no apparent physical anomalies were observed.
Chromosomal balanced translocation refers to the exchange of two chromosomes after a break in the chromosome. It involves only a change in position but not an increase or decrease in chromosome segments. This indicates that genetic material is not duplicated or lost, and carriers usually do not exhibit any abnormal clinical phenotypes[2]. The proband of family 1 was a pregnant woman who carried a balanced translocation involving chromosomes 18 and 19. The proband of family 2 was the husband of a pregnant woman who had a balanced translocation involving chromosomes 5 and 18. According to Mendel’s laws of inheritance, when germ cells of balanced translocation carriers undergo meiosis, only one normal type of gamete can be formed, and the rest are partially trisomic or partially monosomic. The fetus of family 1 was formed by combining 1/18 of the equilibrium-translocated gametes with normal gametes. They exhibited normal appearance, intelligence, and development after birth but faced reproductive challenges in adulthood, increasing the risk of miscarriage and stillbirth in their spouses[3]. The fetus of family 2 was formed by combining gametes with unbalanced translocations of the remaining 16/18 with normal gametes, resulting in an unequal total amount of genetic material, a partial trisomy of chromosome 5, and a partial monosomy of chromosome 18, with the most common being fetal malfor
On the other hand, Roche translocation is a specific type of translocation arising from the fusion of the long arms of chromosomes 13-15 and 21-22 using mitotic fusion. This translocation often leads to the loss of the short arm of the chromosome with virtually no essential genes. Therefore, carriers generally have a normal phenotype[6]. Roche translocation can produce 1/6 normal and 1/6 translocation-type gametes, and the rest are monomorphic or trisomic when forming gametes. The fetus of family 3 was formed by 1/6 translocation gametes, but CNVs did not detect any abnor
In conclusion, carriers of chromosomal translocations have a high risk of adverse pregnancy outcomes. However, they could still have normal offspring. Carriers of balanced chromosomal translocations should undergo timely prenatal diagnosis during pregnancy or consider assisted reproductive technologies to reduce the reproductive risks associated with carrying such translocations. However, evaluating the risk to the fetus after birth and determining whether to recommend pregnancy termination is a challenge in prenatal genetic counseling. The combined use of chromosomal karyotype analysis and molecular genetic testing can enhance the accuracy of prenatal diagnoses. This approach provides prospective parents with clear genetic information about the fetus, helping them make informed decisions regarding the continuation or termination of the pregnancy, or preparation for postnatal treatment of the newborn.
| 1. | Ozawa N, Maruyama T, Nagashima T, Ono M, Arase T, Ishimoto H, Yoshimura Y. Pregnancy outcomes of reciprocal translocation carriers who have a history of repeated pregnancy loss. Fertil Steril. 2008;90:1301-1304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Poornima S, Daram S, Krishna R, Hasan Q. Robertsonian and Balanced Reciprocal Translocation in Both Child and Mother with a History of Recurrent Abortions. J Reprod Infertil. 2020;21:65-67. [PubMed] |
| 3. | Wilch ES, Morton CC. Historical and Clinical Perspectives on Chromosomal Translocations. Adv Exp Med Biol. 2018;1044:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 4. | Zhang HG, Wang RX, Pan Y, Zhang H, Li LL, Zhu HB, Liu RZ. A report of nine cases and review of the literature of infertile men carrying balanced translocations involving chromosome 5. Mol Cytogenet. 2018;11:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yakut S, Çetin Z, Şİmşek M, Mendilcioğlu II, Toru HS, Berker Karaüzüm S, Lüleci G. Rare structural chromosomal abnormalities in prenatal diagnosis; clinical and cytogenetic findings on 10125 prenatal cases. Turk Patoloji Derg. 2015;31:36-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Alfarawati S, Fragouli E, Colls P, Wells D. Embryos of robertsonian translocation carriers exhibit a mitotic interchromosomal effect that enhances genetic instability during early development. PLoS Genet. 2012;8:e1003025. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/