Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.100169
Revised: September 5, 2024
Accepted: March 6, 2025
Published online: July 16, 2025
Processing time: 236 Days and 17.9 Hours
According to the GLOBCAN2022 database, pancreatic cancer has become the 6th leading cause of cancer-related death worldwide. The latest statistics suggest that the incidence of pancreatic cancer is increasing at a rate of 0.5% to 1.0% per year, and it is expected to become the 2nd leading cause of tumor-related deaths in the United States by 2030. More than 50% of pancreatic cancer patients have already developed distant metastases at the time of diagnosis, with the liver being the most common site. Patients with pancreatic cancer with liver metastasis (PCLM) have a worse prognosis than those with locally progressed pancreatic cancer, with a median survival of less than six months. Therefore, the outcome of liver metastases is often a vital determinant of the prognosis of patients with PCLM. There are few successful cases of localized treatment for PCLM patients. Our department recently performed local radiofrequency ablation (RFA) treatment for a PCLM patient through an evidence-based medicine approach, with remarkable therapeutic effects.
The patient was admitted to the hospital on May 03, 2018, 3 weeks after pancreatic cancer surgery. In October 2017, the patient presented with lower back pain. No abnormalities were detected via computed tomography (CT), colonoscopy, or gastroscopy. However, on March 18, 2018, the patient was investigated in a foreign hospital via CT, which suggested occupational lesions in the descending part of the duodenum, and magnetic resonance imaging suggested pancreatic occupancy. He was considered to be suffering from pancreatic cancer. He underwent laparoscopic-assisted pancreatic + duodenum + superior mesenteric vein partial resection and reconstruction under general anesthesia on March 26, 2018 at The Affiliated Hospital of Xuzhou Medical University. The pancreas and duodenum were partially resected. Postoperative pathology showed adenocarcinoma of the pancreas (moderately differentiated), partly mucinous carcinoma, invading the mucosal layer of the duodenum; the tumor size was 4.5 cm × 4 cm × 4 cm. There was no apparent nerve or vascular invasion. There was no cancer or involvement of the pancreas section or expected hepatic duct margins. There was no cancer involvement in the gastric and duodenal sections. There was no cancer metastasis to the peripheral lymph nodes of the pancreas (0/9). No metastasis to the gastric lesser curvature or more significant curvature lymph nodes (0/1, 0/5) was detected, and the peri-intestinal lymph nodes showed no cancer metastasis (0/4). Although the gallbladder showed signs of chronic cholecystitis, there was no cancer involvement, and the lymph nodes in Groups 12 and 13 also showed no cancer metastasis (0/6, 0/1). His postoperative recovery was acceptable. CT was performed on May 2018 at our hospital and found the following: (1) Double lung bronchial vascular bundles slightly heavier than normal; (2) Postoperative changes in the pancreas and a retention tube shadow in front of the head of the pancreas; (3) Small cysts in the right lobe of the liver; (4) Abdominopelvic effusion; and (5) Para splenic enlargement. pTNM stage: PT3N0M0. The patient was in the second stage of postoperative pancreatic cancer, with a potential risk of recurrence considering the patient's postoperative body quality deviation. The patient was unable to tolerate the standard multidrug combination and underwent six cycles of single-agent gemcitabine chemotherapy from May 10, 2018 to August 31, 2018 (the specific drug dosage was 1.4 g/d1/d8 gemcitabine injection, which was repeated every 21 days). Efficacy was determined to be stable disease after 2, 4, and 6 cycles. The side effects during treatment were tolerable.
This case suggests that RFA can serve as a viable local treatment modality for selected patients with PCLM, offering a chance for long-term survival. Such localized interventions, when carefully tailored, may complement systemic therapies in controlling metastatic pancreatic cancer.
Core Tip: Patients with pancreatic cancer liver metastases have a worse prognosis than locally advanced pancreatic cancer patients do, with a median survival of less than 6 months; however, patients are now surviving for more than 6 years after radiofrequency ablation.
- Citation: Yong JP, Mu XY, Zhou CF, Zhang KK, Gao JQ, Guo ZZ, Zhou SF, Ma Z. Radiofrequency ablation of liver metastases in a patient with pancreatic cancer and long-term survival: A case report. World J Clin Cases 2025; 13(20): 100169
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/100169.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.100169
According to the GLOBCAN2022 database, pancreatic cancer has become the 6th leading cause of cancer-related deaths worldwide[1]. The latest statistics suggest that the incidence of pancreatic cancer is increasing at a rate of 0.5% to 1.0% per year, and it is expected to become the 2nd leading cause of tumor-related deaths in the United States by 2030[2]. More than 50% of pancreatic cancer patients have already developed systemic distant metastases at the time of diagnosis, with the liver being the most common site of metastasis for pancreatic cancer. Patients with pancreatic cancer with liver metastasis (PCLM) have a worse prognosis than those with locally progressed pancreatic cancer, with a median survival of less than six months[3]. Therefore, the outcome of liver metastases is often a vital determinant of the prognosis of patients with PCLM. There are few successful cases of localized treatment for PCLM patients; however, our department recently performed local radiofrequency ablation (RFA) treatment for a PCLM patient through an evidence-based medicine approach, with remarkable therapeutic effects, which are reported herein.
The patient was admitted to the hospital on March 03, 2018, 3 weeks after pancreatic cancer surgery.
There was no significant past medical history. There were no chronic diseases, previous surgeries, hospitalizations, or known allergies. The patient was not on any current or past medications and had no notable significant illnesses. The patient’s family medical history was unremarkable.
In October 2017, the patient experienced lower back pain. No abnormalities were detected via computed tomography (CT), colonoscopy, or gastroscopy. On March 18, 2018, the patient was investigated in a foreign hospital via CT, which suggested occupational lesions in the descending part of the duodenum, and magnetic resonance imaging (MRI) suggested pancreatic occupancy. The patient was considered to be suffering from pancreatic cancer. He underwent laparoscopic-assisted pancreatic + duodenum + superior mesenteric vein partial resection and reconstruction under general anesthesia on March 26, 2018 at the Affiliated Hospital of Xuzhou Medical University. The pancreas and duodenum were partially resected. Postoperative pathology revealed adenocarcinoma of the pancreas (moderately differentiated), partly mucinous carcinoma, invading the mucosal layer of the duodenum.
The individual has a healthy lifestyle with no significant occupational or social issues and no relevant travel history or hobbies that could have impacted his health. No significant genetic disorders or chronic illnesses were reported in the family.
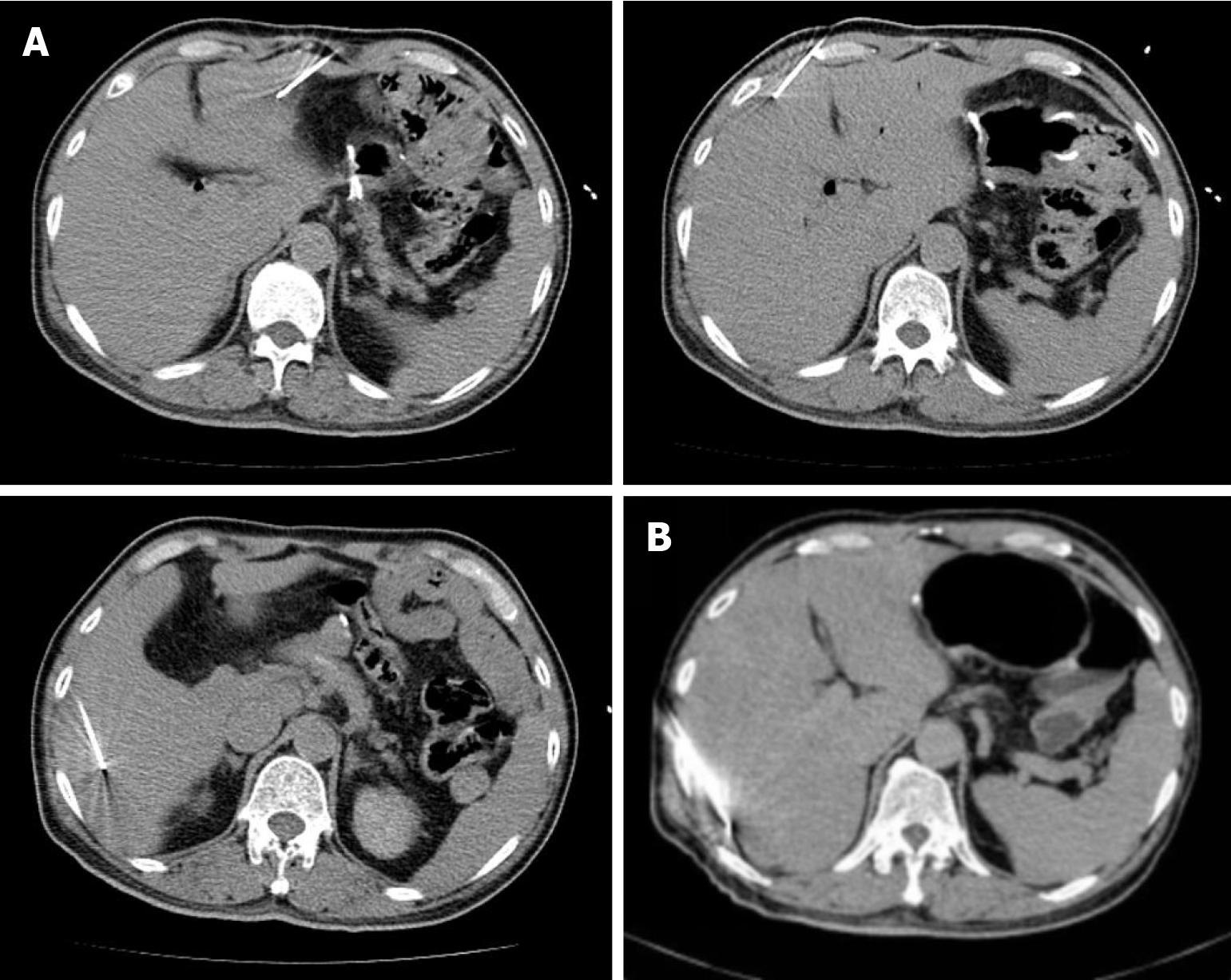
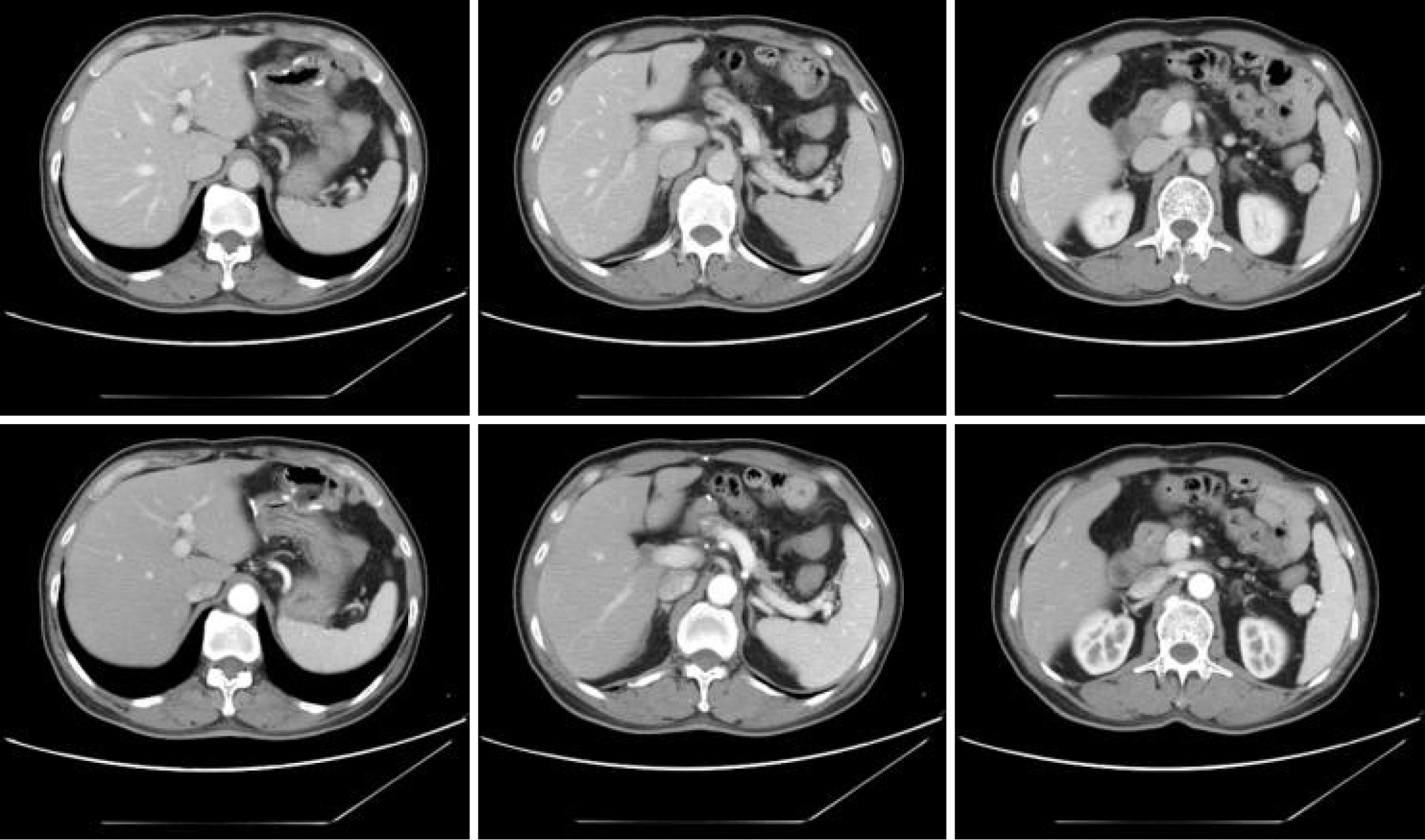
RFA of liver metastases was performed on the patient (Figure 1).
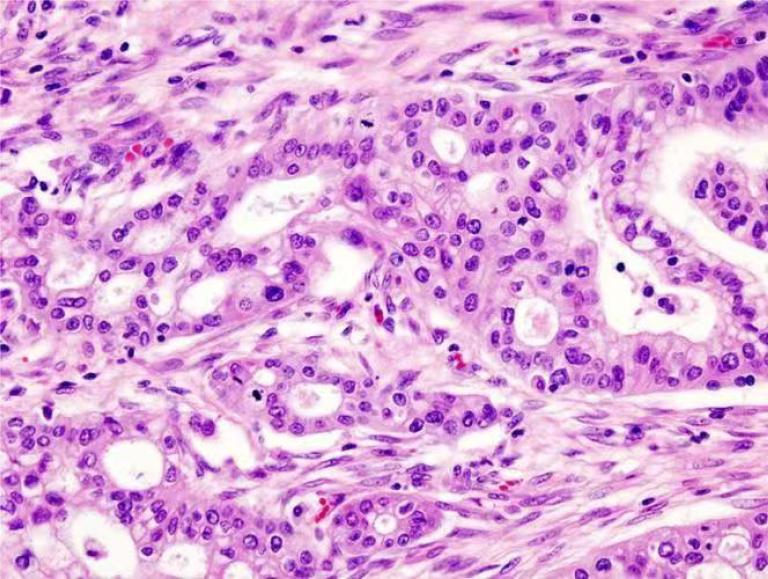
Resected tumor, 4.5 cm × 4 cm × 4 cm; no apparent nerve or vascular invasion, no cancer or involvement of the pancreas section and expected hepatic duct margins, no cancer involvement in the gastric or duodenal sections, no cancer metastasis to the peripheral lymph nodes of the pancreas (0/9), and no metastasis to the gastric lesser curvature or more significant curvature lymph nodes (0/1, 0/5), and the peri-intestinal lymph nodes show no cancer metastasis (0/4); the gallbladder shows chronic cholecystitis but no cancer involvement, and the lymph nodes in Groups 12 and 13 have no cancer metastasis (0/6, 0/1; Figure 2).
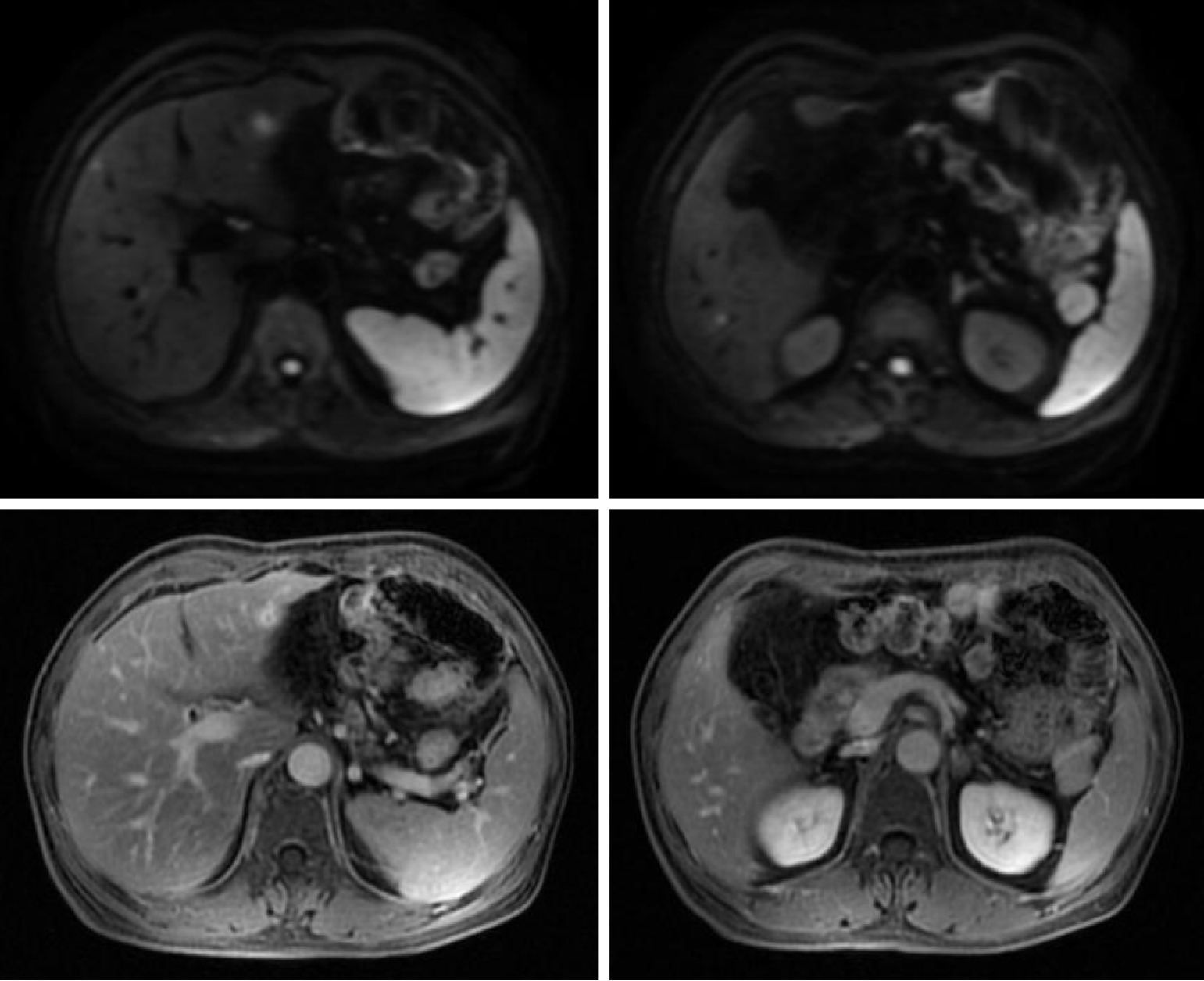
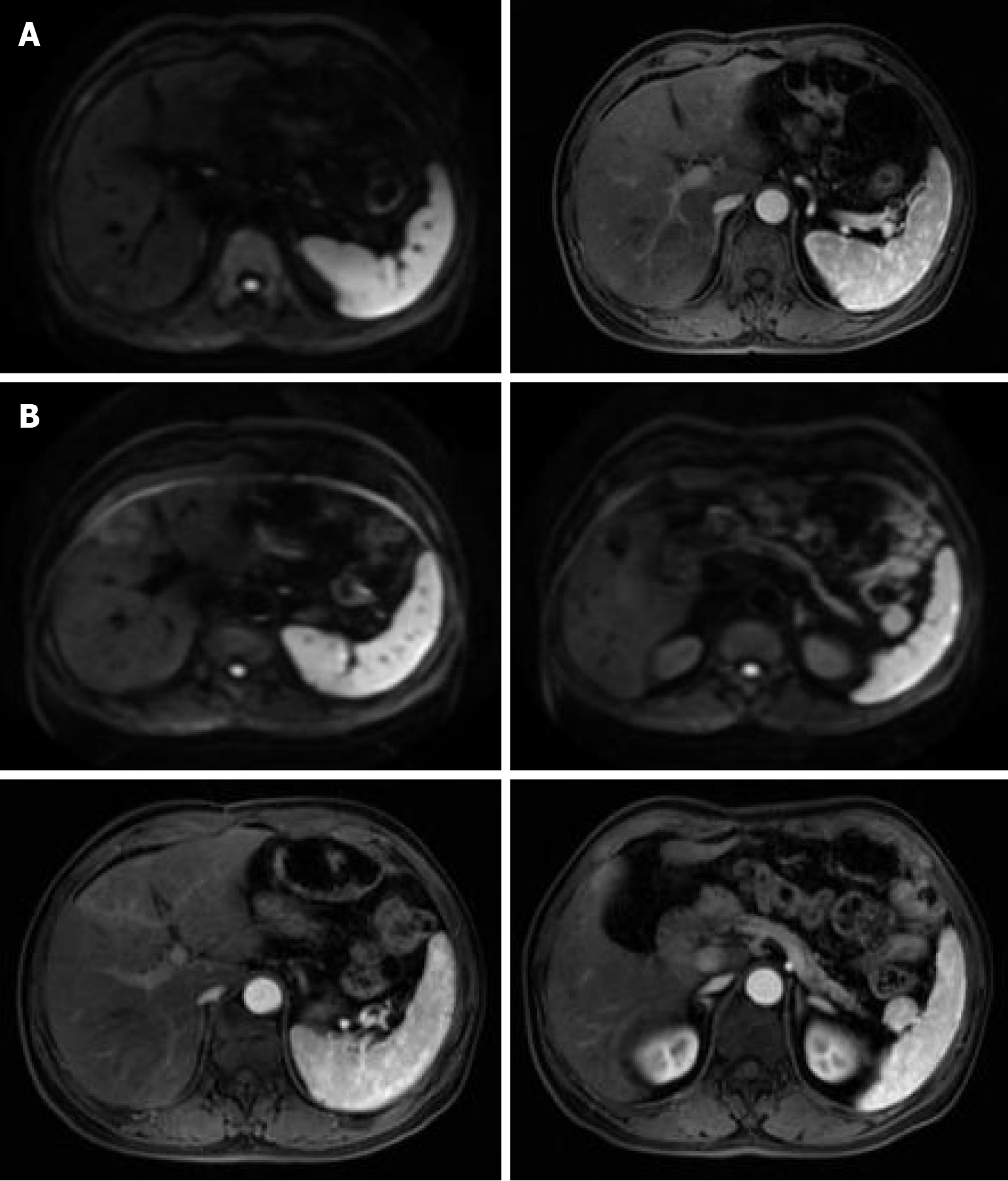
MRI testing was conducted on the patient (Figures 3 and 4).
A diagnosis of PCLM was made.
Metastatic pancreatic cancer has historically been considered a disease with an inferior prognosis, with a survival of less than one year, even with the most effective combination chemotherapy. This patient has experienced prolonged survival of 6 years postoperatively to date, thanks to RFA treatment applied as soon as the liver metastasis was detected (Figure 5).
After completing two rounds of RFA, the patient achieved scomplete remission of the liver metastasis. Remarkably, no recurrence of the metastatic liver tumor was observed over a six-year follow-up period since the initial treatment, indicating a favorable long-term outcome.
Pancreatic cancer is a common malignant tumor of the digestive tract, which has the highest morbidity and mortality rate and the lowest survival rate among all digestive tract tumors, and the 5-year survival rate of patients is only 7%-9%. Due to its deep location and lack of early diagnostic methods, 70%-80% of pancreatic cancer patients are diagnosed with locally advanced or distant metastases, and only 10% of patients are suitable for surgical resection[4]. Among operable patients, surgical resection is still the most effective treatment for pancreatic cancer. Still, postoperative distant metastasis and local recurrence are common, and the median survival of patients with postoperative combined adjuvant therapy is primarily located in 24-28 months[5,6]. The conventional treatment process for resectable pancreatic cancer is radical (R0) resection followed by postoperative adjuvant chemotherapy, and the recommended regimen is combination chemotherapy based on gemcitabine or fluorouracil analogs[7]. The patient was found in time, with no organ metastasis before surgery, and no invasion of lymph nodes, vasculature, nerves, or surrounding organs and tissues was seen in the pathology sent for examination after surgical resection. To reduce the risk of recurrence and metastasis in the postope
This case suggests that RFA can serve as a viable local treatment modality for select patients with PCLM, offering a chance for long-term survival. Such localized interventions, when carefully tailored, may complement systemic therapies in controlling metastatic pancreatic cancer.
| 1. | Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74:229-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5690] [Cited by in RCA: 12727] [Article Influence: 6363.5] [Reference Citation Analysis (8)] |
| 2. | Park W, Chawla A, O'Reilly EM. Pancreatic Cancer: A Review. JAMA. 2021;326:851-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 798] [Cited by in RCA: 1307] [Article Influence: 261.4] [Reference Citation Analysis (0)] |
| 3. | Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet. 2020;395:2008-2020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 869] [Cited by in RCA: 1847] [Article Influence: 307.8] [Reference Citation Analysis (1)] |
| 4. | Adamska A, Domenichini A, Falasca M. Pancreatic Ductal Adenocarcinoma: Current and Evolving Therapies. Int J Mol Sci. 2017;18:1338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 382] [Cited by in RCA: 454] [Article Influence: 50.4] [Reference Citation Analysis (1)] |
| 5. | Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, Schramm H, Fahlke J, Zuelke C, Burkart C, Gutberlet K, Kettner E, Schmalenberg H, Weigang-Koehler K, Bechstein WO, Niedergethmann M, Schmidt-Wolf I, Roll L, Doerken B, Riess H. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1779] [Cited by in RCA: 1791] [Article Influence: 94.3] [Reference Citation Analysis (0)] |
| 6. | Neoptolemos JP, Palmer DH, Ghaneh P, Psarelli EE, Valle JW, Halloran CM, Faluyi O, O'Reilly DA, Cunningham D, Wadsley J, Darby S, Meyer T, Gillmore R, Anthoney A, Lind P, Glimelius B, Falk S, Izbicki JR, Middleton GW, Cummins S, Ross PJ, Wasan H, McDonald A, Crosby T, Ma YT, Patel K, Sherriff D, Soomal R, Borg D, Sothi S, Hammel P, Hackert T, Jackson R, Büchler MW; European Study Group for Pancreatic Cancer. Comparison of adjuvant gemcitabine and capecitabine with gemcitabine monotherapy in patients with resected pancreatic cancer (ESPAC-4): a multicentre, open-label, randomised, phase 3 trial. Lancet. 2017;389:1011-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1327] [Cited by in RCA: 1464] [Article Influence: 162.7] [Reference Citation Analysis (0)] |
| 7. | Oettle H, Neuhaus P, Hochhaus A, Hartmann JT, Gellert K, Ridwelski K, Niedergethmann M, Zülke C, Fahlke J, Arning MB, Sinn M, Hinke A, Riess H. Adjuvant chemotherapy with gemcitabine and long-term outcomes among patients with resected pancreatic cancer: the CONKO-001 randomized trial. JAMA. 2013;310:1473-1481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1180] [Cited by in RCA: 1423] [Article Influence: 109.5] [Reference Citation Analysis (0)] |
| 8. | Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, Adenis A, Raoul JL, Gourgou-Bourgade S, de la Fouchardière C, Bennouna J, Bachet JB, Khemissa-Akouz F, Péré-Vergé D, Delbaldo C, Assenat E, Chauffert B, Michel P, Montoto-Grillot C, Ducreux M; Groupe Tumeurs Digestives of Unicancer; PRODIGE Intergroup. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364:1817-1825. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4838] [Cited by in RCA: 5907] [Article Influence: 393.8] [Reference Citation Analysis (24)] |
| 9. | Von Hoff DD, Ervin T, Arena FP, Chiorean EG, Infante J, Moore M, Seay T, Tjulandin SA, Ma WW, Saleh MN, Harris M, Reni M, Dowden S, Laheru D, Bahary N, Ramanathan RK, Tabernero J, Hidalgo M, Goldstein D, Van Cutsem E, Wei X, Iglesias J, Renschler MF. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med. 2013;369:1691-1703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4035] [Cited by in RCA: 5147] [Article Influence: 395.9] [Reference Citation Analysis (12)] |
| 10. | Konstantinidis IT, Warshaw AL, Allen JN, Blaszkowsky LS, Castillo CF, Deshpande V, Hong TS, Kwak EL, Lauwers GY, Ryan DP, Wargo JA, Lillemoe KD, Ferrone CR. Pancreatic ductal adenocarcinoma: is there a survival difference for R1 resections versus locally advanced unresectable tumors? Ann Surg. 2013;257:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 318] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 11. | Tachezy M, Gebauer F, Janot M, Uhl W, Zerbi A, Montorsi M, Perinel J, Adham M, Dervenis C, Agalianos C, Malleo G, Maggino L, Stein A, Izbicki JR, Bockhorn M. Synchronous resections of hepatic oligometastatic pancreatic cancer: Disputing a principle in a time of safe pancreatic operations in a retrospective multicenter analysis. Surgery. 2016;160:136-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 121] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 12. | Hua YQ, Wang P, Zhu XY, Shen YH, Wang K, Shi WD, Lin JH, Meng ZQ, Chen Z, Chen H. Radiofrequency ablation for hepatic oligometastatic pancreatic cancer: An analysis of safety and efficacy. Pancreatology. 2017;17:967-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Yan X, Ning ZY, Wang P, Zhuang LP, Xu LT, Zhu ZF, Sheng J, Shen YH, Hua YQ, Meng ZQ. Combined ablation-chemotherapy versus chemotherapy alone for pancreatic cancer with liver metastasis: a propensity score matching study. Expert Rev Gastroenterol Hepatol. 2021;15:1047-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 14. | Faraoni EY, O'Brien BJ, Strickland LN, Osborn BK, Mota V, Chaney J, Atkins CL, Cen P, Rowe J, Cardenas J, Poulsen KL, Wray CJ, Thosani NC, Bailey-Lundberg JM. Radiofrequency Ablation Remodels the Tumor Microenvironment and Promotes Neutrophil-Mediated Abscopal Immunomodulation in Pancreatic Cancer. Cancer Immunol Res. 2023;11:4-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 44] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/