Published online Jul 6, 2025. doi: 10.12998/wjcc.v13.i19.102484
Revised: February 13, 2025
Accepted: February 25, 2025
Published online: July 6, 2025
Processing time: 150 Days and 3.3 Hours
The rising prevalence of chronic multimorbidity poses substantial challenges to healthcare systems, necessitating the development of innovative management strategies to optimize patient care and system efficiency. The study by Fontalba-Navas et al investigates the implementation of a novel high complexity unit (HCU) specifically designed to improve the management of patients with chronic complex conditions. By adopting a multidisciplinary approach, the HCU aims to provide comprehensive, patient-centered care that enhances health outcomes and alleviates the strain on traditional hospital services. Utilizing a longitudinal analysis of data from the Basic Minimum Data Set, this study compares hospitalization metrics among the HCU, Internal Medicine, and other departments within a regional hospital throughout 2022. The findings reveal that the HCU's integrated care model significantly reduces readmission rates and boosts patient satisfaction compared to conventional care practices. The study highlights the HCU's poten
Core Tip: Fontalba-Navas et al's study analyzes a high complexity unit (HCU) designed to tackle chronic multimorbidity through a multidisciplinary, patient-centered approach. The HCU's integrated care model significantly improves health outcomes, reduces readmission rates, and enhances patient satisfaction, as evidenced by longitudinal data from the Basic Minimum Data Set. This innovative framework alleviates the strain on traditional healthcare services by minimizing unnecessary hospitalizations and improving care quality. The HCU serves as a replicable model for healthcare systems facing similar challenges, offering a sustainable strategy for managing the rising prevalence of chronic multimorbidities and optimizing healthcare delivery.
- Citation: Byeon H. Innovative approaches to managing chronic multimorbidity: A multidisciplinary perspective. World J Clin Cases 2025; 13(19): 102484
- URL: https://www.wjgnet.com/2307-8960/full/v13/i19/102484.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i19.102484
Chronic diseases pose a significant challenge to global healthcare systems, affecting millions and straining resources due to their persistent and often debilitating nature[1]. Recent studies have shown that chronic diseases are responsible for over 70% of all deaths worldwide, highlighting their impact on global health[2]. Conditions such as diabetes, hyper
Patients with complex chronic conditions frequently experience multiple comorbidities, which complicate their management and result in increased healthcare utilization. Comorbidity, the presence of multiple simultaneous chronic conditions, requires a comprehensive and coordinated approach to care. This complexity often leads to fragmented healthcare delivery, increased risk of medication interactions, and frequent hospital admissions. Effective management of these patients necessitates a shift towards a patient-centered model of care[5,6]. This involves engaging patients actively in their treatment plans, promoting self-care education, and ensuring cohesive communication across healthcare providers[7]. Such an approach is crucial for reducing hospital readmissions and improving overall patient outcomes.
In this context, the recent study by Fontalba-Navas et al[8] introduces the high complexity unit (HCU) as an innovative model designed to meet the intricate needs of patients with complex chronic diseases. The HCU focused on providing comprehensive, multidisciplinary care aimed at preventing unnecessary hospitalizations and mitigating the adverse effects associated with extended hospital stays[8]. By prioritizing personalized care strategies and fostering strong coordination among healthcare professionals, the HCU sought to enhance patient and caregiver experiences[8].
The HCU is distinguished by its emphasis on individualized care, low staff-to-patient ratios, and integration of multidisciplinary expertise. It prioritizes the continuity of care, particularly during the transition from hospital to home, and incorporates comprehensive evaluations to track patient progress. This model not only addresses the clinical needs of patients but also supports caregivers through targeted interventions and resource management.
Managing complex chronic patients effectively remains a daunting task for modern health systems, demanding substantial resources and meticulous coordination of care. The HCU represents a transformative approach, offering a specialized framework that prioritizes personalized treatment and seamless care transitions. This editorial explores the operational procedures within the HCU and underscores the importance of a stratified, multidisciplinary strategy in achieving optimal patient outcomes and satisfaction.
The management of chronic diseases has increasingly shifted towards a patient-centered approach[7], recognizing the importance of individualized care that respects and responds to the unique preferences, needs, and values of each patient. This paradigm is particularly crucial in the context of chronic conditions, where long-term management and patient engagement are essential for effective care.
Patient-centered care emphasizes the active involvement of patients in their own healthcare decisions, promoting shared decision-making between patients and healthcare providers[8]. This approach not only enhances patient satisfaction but also improves adherence to treatment plans, as patients are more likely to commit to therapies they have helped design and understand. Previous research[9,10] has shown that when patients are actively engaged in their care, they experience better health outcomes, reduced hospitalizations, and improved quality of life.
In the realm of chronic disease management, patient-centered care involves a comprehensive assessment of individual patient needs, including medical, psychological, and social aspects[11]. This holistic view allows healthcare providers to tailor interventions that address the entire spectrum of factors affecting a patient's health. Such strategies may include personalized medication plans, lifestyle modifications, and psychosocial support, all coordinated through a multidisciplinary team approach[12].
Furthermore, patient-centered care encourages the use of technology to enhance communication and information sharing. Tools such as electronic health records, patient portals, and telemedicine platforms facilitate continuous interaction between patients and providers, ensuring timely updates and adjustments to care plans[13]. These technologies empower patients by providing them with easy access to their health information and the ability to engage with their care teams remotely.
The implementation of patient-centered care models, like those in HCU, demonstrates the potential for transforming chronic disease management. By focusing on the unique needs of each patient and fostering a collaborative care environment, these models not only improve clinical outcomes but also enhance the overall healthcare experience for patients and their families[14]. As healthcare systems continue to evolve, the integration of patient-centered practices will be pivotal in addressing the growing burden of chronic diseases.
HCU have emerged as an innovative response to the intricate challenges posed by chronic patients with multifaceted health needs[15]. These specialized units are designed to provide comprehensive, multidisciplinary care tailored specifically to individuals with complex chronic conditions, who often require intensive, coordinated management strategies.
The primary objective of HCUs is to mitigate the burden of chronic diseases by preventing unnecessary hospitalizations, minimizing the risk of complications, and enhancing overall patient outcomes[16]. By integrating a broad spectrum of healthcare professionals, including physicians, nurses, social workers, and allied health specialists, HCUs facilitate a holistic approach to patient care. This multidisciplinary collaboration ensures that all aspects of a patient's health—medical, psychological, and social—are addressed in a cohesive manner.
Previous research[17] has demonstrated that HCUs significantly improve clinical outcomes for chronic patients. These units reduce hospital readmission rates by implementing proactive management strategies and individualized care plans that are continuously monitored and adjusted as necessary[18]. The presence of dedicated care teams within HCUs allows for rapid identification and response to changes in a patient's condition, thereby preventing the escalation of health issues that could lead to acute care interventions.
Moreover, HCUs emphasize the importance of continuity of care, particularly during transitions between hospital and home[19]. This seamless transition is facilitated through comprehensive discharge planning and follow-up care, which are integral components of the HCU model. Patients and their caregivers are educated and supported throughout the process, ensuring that they are well-prepared to manage chronic conditions independently.
The impact of HCUs extends beyond clinical outcomes, contributing to improved patient satisfaction and quality of life. By fostering a patient-centered environment that prioritizes individualized attention and respect for patient preferences, HCUs empower patients to take an active role in their healthcare journey[20]. Additionally, the supportive framework of HCUs alleviates the caregiving burden, providing families with the resources and guidance needed to navigate complex healthcare landscapes.
As healthcare systems continue to grapple with the rising prevalence of chronic diseases, the role of HCUs becomes increasingly vital. These units exemplify how strategic resource allocation and a focus on coordinated care can transform the management of chronic patients, ultimately leading to more sustainable and effective healthcare delivery models. A review of previous studies[21-31] on the effectiveness of high-complexity units for chronic patients is presented in Table 1.
| Ref. | Focus area | Key findings |
| Berkman et al[21] | Heart failure | Reduction in hospital readmissions; improved symptom management |
| Collado et al[22] | COPD | Better control of exacerbations; enhanced medication adherence |
| Evans et al[23] | Chronic kidney disease | Lower mortality rates in HCUs |
| Huth et al[24] | Diabetes | No significant difference in mortality between HCUs and standard care |
| Osunkwo et al[25] | Patient satisfaction | Higher satisfaction scores due to personalized care |
| Murphy Salem et al[26] | Mental health | Increased sense of security; improved mental health outcomes |
| Salem et al[26] | Physical health | Better outcomes due to coordinated care and monitoring |
| Osunkwo et al[25] | Mental health | Reduced anxiety and depression levels |
| Collado et al[22] | Cost implications | Higher initial costs; long-term savings through reduced readmissions |
| Berkman et al[21] | Cost-benefit analysis | HCUs are cost-effective for complex chronic patients |
| Paoloni-Giacobino et al[27] | Efficiency and workflow | Streamlined care delivery; reduced unnecessary tests and procedures |
| Thompson et al[28] | Resource allocation | Improved resource utilization; optimized healthcare delivery |
| Suárez-Avellaneda et al[29] | SLE in ICUs | Importance of evaluating disease severity for management and outcomes |
| Onofri et al[30] | Cardiogenic shock economic impact | Significant costs with a focus on critical care unit stays |
| Onofri et al[30] | Telemedicine in CMC | Effective tool for maintaining continuity of care during the pandemic |
| Leeksma et al[31] | Genomic arrays in CLL | Personalized care potential through risk stratification |
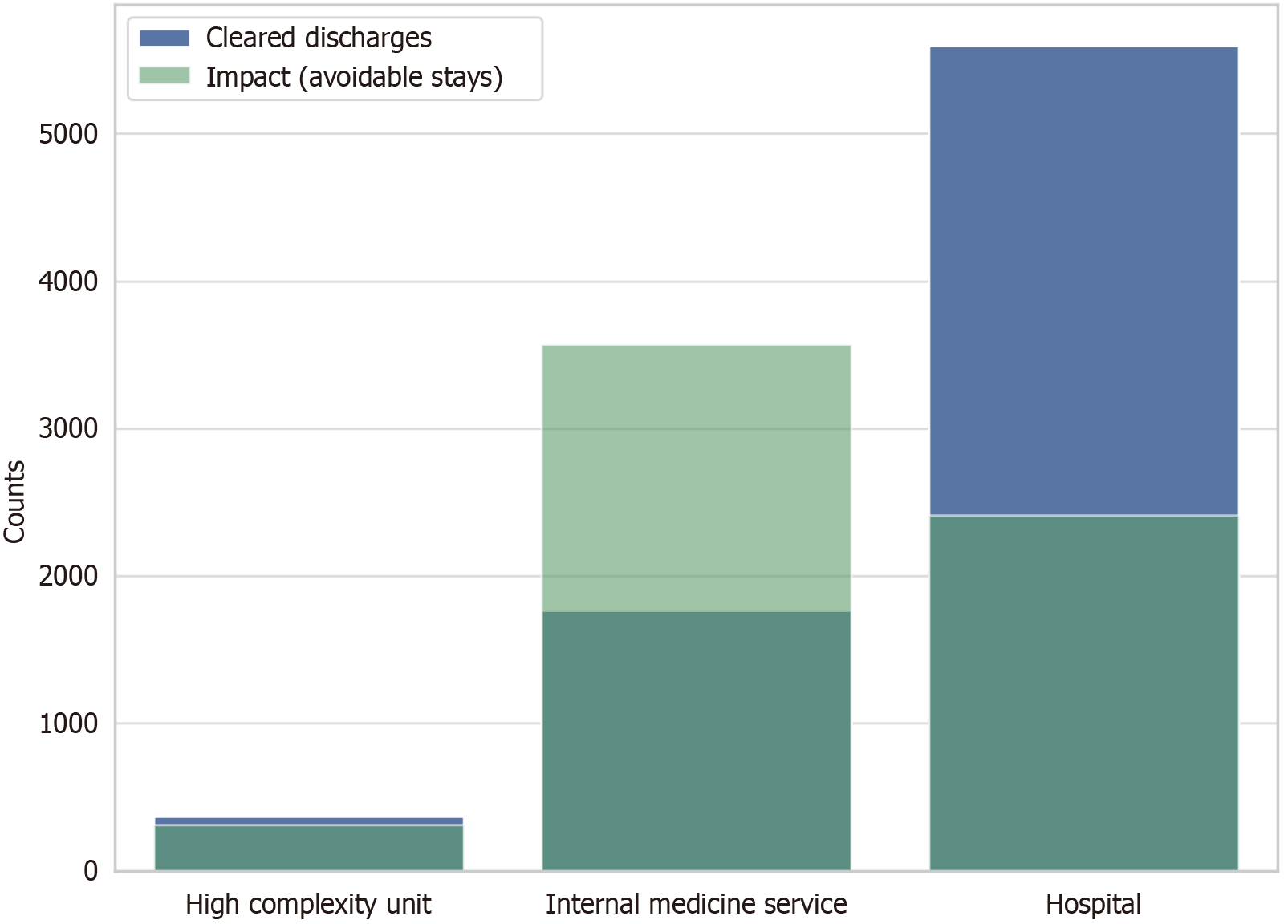
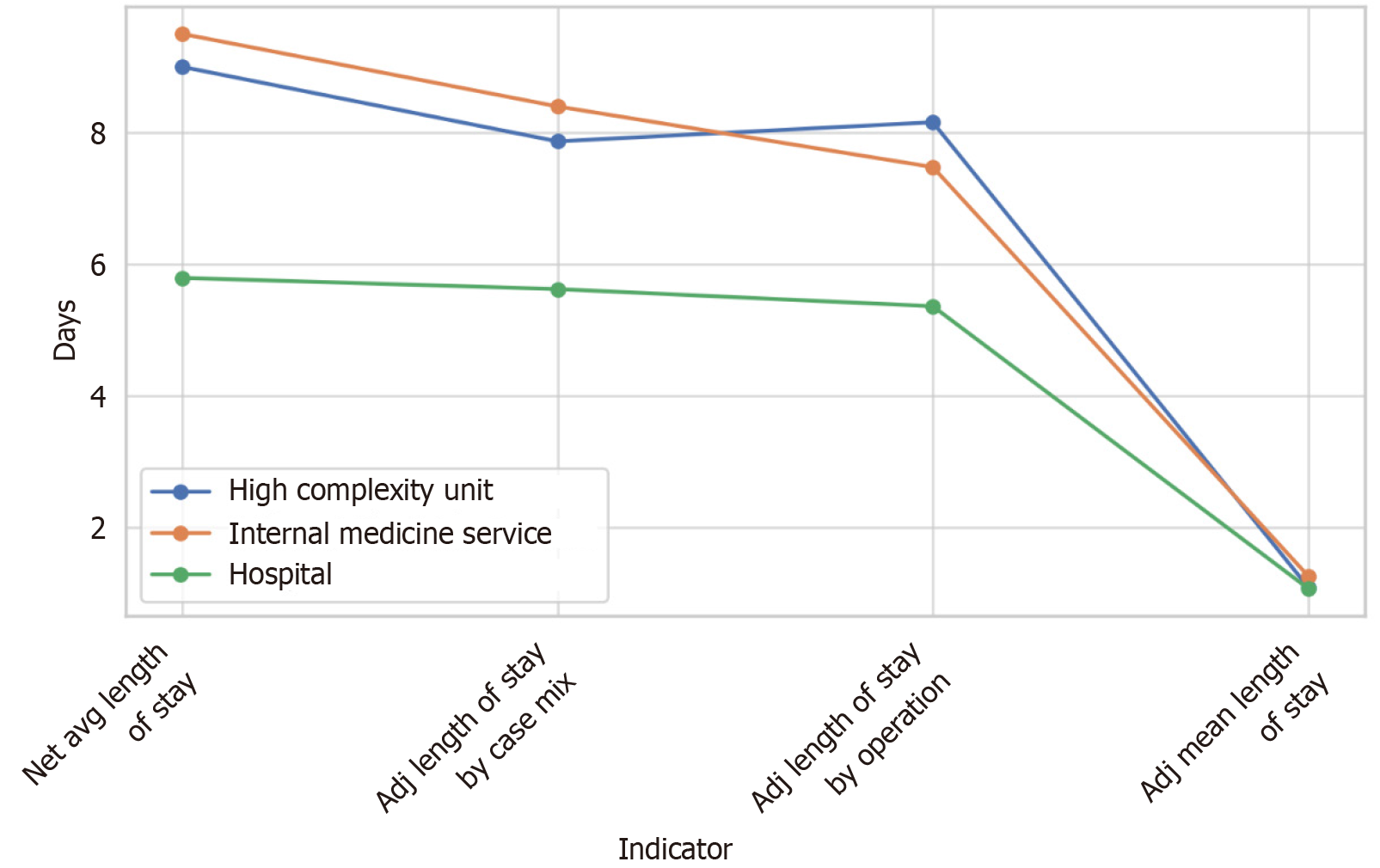
The study conducted by Fontalba-Navas et al[8] provides an in-depth analysis of the HCU and its effectiveness in managing patients with complex chronic conditions. Utilizing a descriptive longitudinal approach, the research compares hospitalization variables among the HCU, the Internal Medicine Service, and other services at Antequera Hospital. Firstly, the HCU demonstrated a substantial reduction in avoidable hospital stays, with 310.56 days recorded compared to 3568.6 days by the Internal Medicine Service, underscoring the unit's efficiency in preventing unnecessary admissions. Secondly, patients in the HCU had an average of 13.72 diagnoses each, exceeding the 10.47 in Internal Medicine and 7.51 in the general hospital, highlighting the unit's capacity to handle more complex and multipathological cases. Thirdly, the HCU averaged 1.89 procedures per patient, a strategic reduction compared to 2.78 in Internal Medicine and 2.39 in the hospital overall, reflecting a more focused and patient-centered selection of interventions. This approach contributes to more efficient resource utilization. Additionally, the HCU's efficiency is further illustrated by its average length of stay adjusted for case mix (7.86 days) and operation (8.15 days), indicating an optimized management adapted to patient complexity. The adjusted mean length of stay was 1.10, demonstrating efficiency despite higher patient complexity. Furthermore, through a comprehensive evaluation involving 170 semi-structured interviews, the study found high levels of patient satisfaction with the care provided by the HCU. The uniform positive feedback across various demographics highlights the effectiveness of the HCU's patient-centered care model. Lastly, the comparison of management indicators, as detailed in Figure 1 and Figure 2, illustrates the HCU's superior performance in several key areas, confirming its effectiveness in managing complex chronic patients through a multidisciplinary approach (Figures 1 and 2).
The study's findings highlight the transformative potential of implementing a comprehensive, patient-centered care framework within HCU, particularly for the management of patients with chronic, multimorbid conditions. This model of care, which actively involves patients in the decision-making process and emphasizes self-care education, is crucial in addressing the challenges posed by an aging population and the increasing prevalence of lifestyle-related health issues.
Firstly, the HCU model demonstrates its effectiveness in reducing the risks associated with polypharmacy and adverse drug interactions. By ensuring coordinated and integrated care across various specialties, HCUs mitigate the complexities of managing multiple medications, which is a common issue among patients with chronic conditions. This integrated approach not only enhances medication safety but also optimizes therapeutic outcomes by tailoring treatment plans to meet individual patient needs[11-13].
Secondly, the patient-centered approach of the HCU fosters improved clinical outcomes by actively engaging patients in their care. This engagement promotes adherence to treatment regimens and encourages patients to take an active role in managing their health, leading to better health behaviors and outcomes. Moreover, the emphasis on patient education empowers individuals to make informed decisions about their care, thereby enhancing their autonomy and satisfaction with the healthcare process[14,15].
Furthermore, HCUs provide a structured environment that supports the seamless integration of multidisciplinary care teams. This collaboration is essential in addressing the multifaceted needs of chronic patients, who often require input from various healthcare professionals. By fostering communication and coordination among these teams, HCUs ensure that care delivery is both comprehensive and cohesive, reducing the likelihood of fragmented care and improving overall patient experiences.
Additionally, the strategic focus on continuity of care within HCUs addresses the critical transition from hospital to home, a vulnerable period for many chronic patients. By implementing detailed discharge planning and follow-up care, HCUs minimize the risk of hospital readmissions and ensure that patients continue to receive the necessary support and resources post-discharge. This continuity is vital in maintaining the progress achieved during hospitalization and in preventing the exacerbation of chronic conditions[16].
Lastly, the HCU model serves as an exemplary framework for healthcare systems aiming to enhance the management of chronic diseases. Its success in improving patient outcomes and reducing healthcare burdens underscores the importance of adopting similar patient-centered, integrated care models across diverse healthcare settings. By doing so, healthcare providers can better meet the growing demands of chronic disease management, ultimately improving the quality of care for patients with complex health needs[17].
Despite providing valuable insights into the management of complex chronic conditions through HCU, this study is subject to several limitations that should be acknowledged to contextualize its findings accurately. Firstly, the study's descriptive longitudinal design inherently limits the ability to establish causal relationships between the interventions implemented by the HCU and the observed outcomes. While the study effectively illustrates associations and trends, the lack of a control group or randomization means that definitive conclusions about causality cannot be drawn. Future research employing experimental designs, such as randomized controlled trials, would be beneficial in confirming these causal links.
Secondly, the study's focus on a specific population within a single healthcare setting poses challenges to the generalizability of its findings. The demographic and clinical characteristics of the patient population at Antequera Hospital may not reflect those of other regions or healthcare systems, particularly where healthcare infrastructures and patient demographics differ significantly. As such, the applicability of the results to broader, more diverse populations may be limited.
Thirdly, the study did not account for certain confounding variables that could influence the outcomes. Factors such as socioeconomic status, lifestyle habits, and genetic predispositions were not controlled for, which may have affected the results. Including these variables in future analyses could enhance the robustness of the findings and provide a more comprehensive understanding of the factors influencing patient outcomes in HCUs.
Fourthly, while the study highlights the effectiveness of the HCU model in reducing hospital stays and improving patient satisfaction, it relies heavily on subjective measures of patient satisfaction obtained through semi-structured interviews. Although valuable, these subjective assessments may be subject to bias, such as recall or social desirability bias. Incorporating objective measures of patient outcomes, such as clinical biomarkers or health-related quality of life indices, would provide a more balanced evaluation of the HCU's impact.
Lastly, the study's reliance on retrospective data collection may have introduced inaccuracies or omissions in the data recorded, potentially affecting the study's conclusions. Prospective data collection methods, which allow for real-time data capture and monitoring, could improve data accuracy and reliability in future research efforts. Addressing these limitations in subsequent studies would help validate the current findings and expand our understanding of how HCUs can be optimized to enhance chronic disease management across various healthcare settings.
The exploration of HCU in managing chronic multimorbid patients presents a promising frontier for future research. To further elucidate their potential, several research directions should be pursued. Expanding the demographic scope of future studies is essential to enhance the applicability and generalizability of the HCU model. By including diverse populations across various geographic, socioeconomic, and cultural backgrounds, researchers can identify how different demographic factors influence the effectiveness of HCUs. This expansion will help tailor the HCU model to meet the unique needs of disparate patient populations, ensuring its adaptability and efficacy in varied healthcare settings.
Incorporating longitudinal study designs to explore the causal pathways and long-term impacts of HCU interventions will provide valuable insights into the progression of chronic diseases and the sustained effects of interventions over time. Such an approach would enable researchers to assess not only immediate outcomes but also the durability of benefits conferred by the HCU model, thereby offering a more comprehensive evaluation of its effectiveness in chronic disease management.
Integrating advanced data analytics and machine learning techniques[32] could significantly enhance the predictive capabilities of HCUs. By analyzing large datasets, researchers can identify patterns and predictors of patient outcomes, enabling more personalized and proactive care strategies[33]. These technological advancements could facilitate the development of decision-support tools that aid healthcare providers in optimizing treatment plans for individual patients based on their unique clinical profiles.
Additionally, exploring the integration of digital health technologies within HCUs is crucial. The use of telemedicine, remote monitoring, and mobile health applications can extend the reach of HCUs beyond the hospital setting, providing continuous support and management for chronic patients in their homes. Research into the effectiveness and feasibility of these technologies in enhancing patient engagement and adherence to care plans would be invaluable in shaping the future landscape of HCU-based care.
Finally, evaluating the cost-effectiveness of the HCU model is crucial in demonstrating its value to healthcare policymakers and stakeholders. By conducting economic analyses that compare the costs and benefits of HCU interventions with traditional care models, researchers can provide evidence of the financial sustainability of HCUs. This information is vital for securing funding and support for the widespread implementation of HCUs within healthcare systems. By pursuing these research directions, the healthcare community can advance its understanding of HCUs, refine their implementation, and ultimately improve the quality of care for patients with complex chronic conditions across the globe.
The study advances our understanding of managing chronic multimorbid patients by demonstrating the efficacy of a multidisciplinary approach in the HCU. This model not only improves clinical outcomes but also optimizes resource utilization, providing a viable solution to the challenges posed by complex chronic conditions. Future studies should continue to refine this model to ensure its adaptability and effectiveness in diverse healthcare contexts.
| 1. | Hajat C, Kishore SP. The case for a global focus on multiple chronic conditions. BMJ Glob Health. 2018;3:e000874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Bloom DE, Chen S, Kuhn M, Mcgovern ME, Oxley L, Prettner K. The economic burden of chronic diseases: Estimates and projections for China, Japan, and South Korea. J Econ of Ageing. 2020;17:100163. [DOI] [Full Text] |
| 3. | Chen TT, Su WC, Liu MI. Patient-centered care in diabetes care-concepts, relationships and practice. World J Diabetes. 2024;15:1417-1429. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (2)] |
| 4. | Hassan EM, Jama AB, Sharaf A, Shaikh A, El Labban M, Surani S, Khan SA. Discharging patients home from the intensive care unit: A new trend. World J Clin Cases. 2024;12:5313-5319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 5. | Świątoniowska-Lonc N, Polański J, Tański W, Jankowska-Polańska B. Impact of satisfaction with physician-patient communication on self-care and adherence in patients with hypertension: cross-sectional study. BMC Health Serv Res. 2020;20:1046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 78] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | Cabrera-león A, Jadad AR, Nuño-solinís R, Bernabéu-wittel M, Morales-asencio JM, Valdivieso-martínez B, Fernández-miera MF, Sampedro-garcía I, March-cerdá JC, Gosálvez-prados D, Espín J. Improving care for people living with chronic diseases: Innovative examples from Spain. Int J Healthc Manage. 2012;5:208-215. [RCA] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Hudon C, Fortin M, Haggerty J, Loignon C, Lambert M, Poitras ME. Patient-centered care in chronic disease management: a thematic analysis of the literature in family medicine. Patient Educ Couns. 2012;88:170-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 8. | Fontalba-Navas A, Pozo Muñoz F, Garcia Cisneros R, Garcia Larrosa MJ, Callejon Gil MDM, Garcia Delgado I, Jimenez Martinez MB. Challenges and improvement strategies in the hospitalization of chronic multimorbid patients. World J Clin Cases. 2025;13:98284. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (5)] |
| 9. | Laurance J, Henderson S, Howitt PJ, Matar M, Al Kuwari H, Edgman-Levitan S, Darzi A. Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Aff (Millwood). 2014;33:1627-1634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 87] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 10. | Vahdat S, Hamzehgardeshi L, Hessam S, Hamzehgardeshi Z. Patient involvement in health care decision making: a review. Iran Red Crescent Med J. 2014;16:e12454. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 363] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 11. | Mirza F, Norris T, Stockdale R. Mobile technologies and the holistic management of chronic diseases. Health Informatics J. 2008;14:309-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Gu YH, Wang X, Sun SS. Benefits of multidisciplinary collaborative care team-based nursing services in treating pressure injury wounds in cerebral infarction patients. World J Clin Cases. 2022;10:43-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Padte S, Samala Venkata V, Mehta P, Tawfeeq S, Kashyap R, Surani S. 21st century critical care medicine: An overview. World J Crit Care Med. 2024;13:90176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (2)] |
| 14. | Flagg AJ. The role of patient-centered care in nursing. Nurs Clin North Am. 2015;50:75-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Tonelli M, Wiebe N, Manns BJ, Klarenbach SW, James MT, Ravani P, Pannu N, Himmelfarb J, Hemmelgarn BR. Comparison of the Complexity of Patients Seen by Different Medical Subspecialists in a Universal Health Care System. JAMA Netw Open. 2018;1:e184852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 16. | Marshall JC, Bosco L, Adhikari NK, Connolly B, Diaz JV, Dorman T, Fowler RA, Meyfroidt G, Nakagawa S, Pelosi P, Vincent JL, Vollman K, Zimmerman J. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 373] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 17. | Lee JY, Muratov S, Tarride JE, Holbrook AM. Managing High-Cost Healthcare Users: The International Search for Effective Evidence-Supported Strategies. J Am Geriatr Soc. 2018;66:1002-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Muratov S, Lee J, Holbrook A, Paterson JM, Guertin JR, Mbuagbaw L, Gomes T, Khuu W, Pequeno P, Costa AP, Tarride JE. Senior high-cost healthcare users' resource utilization and outcomes: a protocol of a retrospective matched cohort study in Canada. BMJ Open. 2017;7:e018488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Pérez-Ardanaz B, Gutiérrez-Rodríguez L, Gómez-González AJ, Morales-Asencio JM, Montero-García A, León-Campos Á. Predictive model for the risk of paediatric intensive care utilization in children with medical complexity: A longitudinal retrospective cohort study. Nurs Crit Care. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Hambly N, Goodwin S, Aziz-Ur-Rehman A, Makhdami N, Ainslie-Garcia M, Grima D, Cox G, Kolb M, Fung D, Cabalteja C, DeMarco P, Moldaver D. A cross-sectional evaluation of the idiopathic pulmonary fibrosis patient satisfaction and quality of life with a care coordinator. J Thorac Dis. 2019;11:5547-5556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Berkman ND, Chang E, Seibert J, Ali R. Characteristics of High-Need, High-Cost Patients : A "Best-Fit" Framework Synthesis. Ann Intern Med. 2022;175:1728-1741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 22. | Collado E, Luiso D, Ariza-Solé A, Lorente V, Sánchez-Salado JC, Moreno R, Alsina M, Tapia J, González-Costello J, Comin-Colet J. Hospitalization-related economic impact of patients with cardiogenic shock in a high-complexity reference centre. Eur Heart J Acute Cardiovasc Care. 2021;10:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Evans M, Lopau K. The transition clinic in chronic kidney disease care. Nephrol Dial Transplant. 2020;35:ii4-ii10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 24. | Huth K, Vandecruys P, Orkin J, Patel H. Medication safety for children with medical complexity. Paediatr Child Health. 2020;25:473-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Osunkwo I, O'Connor HF, Saah E. Optimizing the management of chronic pain in sickle cell disease. Hematology Am Soc Hematol Educ Program. 2020;2020:562-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Murphy Salem S, Graham RJ. Chronic Illness in Pediatric Critical Care. Front Pediatr. 2021;9:686206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 27. | Paoloni-Giacobino A, Luthi F, Stenz L, Le Carré J, Vuistiner P, Léger B. Altered BDNF Methylation in Patients with Chronic Musculoskeletal Pain and High Biopsychosocial Complexity. J Pain Res. 2020;13:1289-1296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 28. | Thompson ER, Nguyen T, Kankanige Y, Anderson MA, Handunnetti SM, Thijssen R, Yeh PS, Tam CS, Seymour JF, Roberts AW, Westerman DA, Blombery P. High Clonal Complexity of Resistance Mechanisms Occurring at Progression after Single-Agent Targeted Therapy Strategies in Chronic Lymphocytic Leukemia. Blood. 2020;136:15-16. [RCA] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 29. | Suárez-Avellaneda A, Quintana JH, Aragón CC, Gallego LM, Gallego CN, Bolaños JD, A Guerra M, Ochoa ME, Granados M, Ruiz-Ordoñez I, Tobón GJ. Systemic lupus erythematosus in the intensive care unit: a systematic review. Lupus. 2020;29:1364-1376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 30. | Onofri A, Pavone M, De Santis S, Verrillo E, Caggiano S, Ullmann N, Cutrera R. Telemedicine in children with medical complexity on home ventilation during the COVID-19 pandemic. Pediatr Pulmonol. 2021;56:1395-1400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 31. | Leeksma AC, Baliakas P, Moysiadis T, Puiggros A, Plevova K, Van der Kevie-Kersemaekers AM, Posthuma H, Rodriguez-Vicente AE, Tran AN, Barbany G, Mansouri L, Gunnarsson R, Parker H, Van den Berg E, Bellido M, Davis Z, Wall M, Scarpelli I, Österborg A, Hansson L, Jarosova M, Ghia P, Poddighe P, Espinet B, Pospisilova S, Tam C, Ysebaert L, Nguyen-Khac F, Oscier D, Haferlach C, Schoumans J, Stevens-Kroef M, Eldering E, Stamatopoulos K, Rosenquist R, Strefford JC, Mellink C, Kater AP. Genomic arrays identify high-risk chronic lymphocytic leukemia with genomic complexity: a multi-center study. Haematologica. 2021;106:87-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 32. | Byeon H. Screening dementia and predicting high dementia risk groups using machine learning. World J Psychiatry. 2022;12:204-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Okpete UE, Byeon H. Challenges and prospects in bridging precision medicine and artificial intelligence in genomic psychiatric treatment. World J Psychiatry. 2024;14:1148-1164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/