Published online Jun 26, 2025. doi: 10.12998/wjcc.v13.i18.102194
Revised: December 11, 2024
Accepted: February 18, 2025
Published online: June 26, 2025
Processing time: 138 Days and 22.6 Hours
This case highlights the importance of a multidisciplinary approach in differentiating localized infections from systemic inflammatory diseases like psoriatic arthritis. Nail psoriasis can mimic conditions like paronychia, complicating diagnosis. We wrote this report to emphasize the need for clinical vigilance when interpreting imaging findings, especially in patients with a family history of psoriasis. Misdiagnosis can lead to unnecessary systemic treatments, undersco
A 56-year-old woman presented with redness and swelling of multiple fingertips. Her family history of psoriasis raised suspicion of psoriatic arthritis. Two rheumatologists diagnosed psoriatic arthritis based on ultrasound findings of enthesitis with a positive Doppler signal and recommended methotrexate. However, she was reluctant to initiate therapy due to potential side effects. At our Rheumatology Center, paronychia was suspected, and laboratory tests excluded systemic inflammatory arthritis. Dermatological examination confirmed paro
This case underscores the need for thorough clinical evaluation and caution in interpreting nonspecific imaging findings, especially in patients with a family history of psoriasis. While familial predisposition may raise suspicion for psoriatic arthritis, it is essential to integrate laboratory data, imaging studies, and clinical presentation, including response to targeted antimicrobial therapy. A multidisciplinary approach, involving both rheumatologists and dermatologists, is crucial to preventing misdiagnosis, ensuring appropriate treatment, and avoiding the potential harms of unwarranted therapies.
Core Tip: This case report emphasizes the importance of a multidisciplinary approach in distinguishing localized conditions, such as paronychia, from systemic inflammatory diseases like psoriatic arthritis. Misdiagnosis based on imaging findings, such as enthesitis with positive Doppler signal, can lead to unnecessary systemic treatments with potential adverse effects. A comprehensive clinical evaluation, including dermatological expertise, revealed paronychia as the underlying condition in a patient initially misdiagnosed with psoriatic arthritis. Timely antimicrobial therapy resolved the symptoms, highlighting the critical role of integrating clinical, imaging, and laboratory findings to avoid diagnostic errors and optimize patient outcomes.
- Citation: Nigro A. Misdiagnosis of psoriatic arthritis in a patient with paronychia confirmed by dermatological examination: A case report. World J Clin Cases 2025; 13(18): 102194
- URL: https://www.wjgnet.com/2307-8960/full/v13/i18/102194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i18.102194
Accurate diagnosis is essential for appropriate treatment, especially when systemic diseases like psoriatic arthritis are suspected[1]. Psoriasis can involve the nails and, in some cases, present features that resemble paronychia. Recent literature suggests that nail psoriasis may mimic inflammatory conditions of the nail bed[2]. Moreover, paronychia can occur as an isolated condition or as a manifestation of underlying systemic diseases, adverse drug reactions, or chemical irritation[3]. We present the case of a 56-year-old woman with a family history of psoriasis, who was initially misdiagnosed with psoriatic arthritis. This case emphasizes the complexity of the differential diagnosis when familial predisposition to psoriasis is present.
The patient, a 56-year-old woman, presented with redness and swelling of multiple fingertips involving several digits (Figure 1).
The symptoms had been present for weeks, prompting consultations with two rheumatologists. Based on her family history of psoriasis and ultrasound findings suggestive of enthesitis with positive Doppler signals, she was diagnosed with psoriatic arthritis and prescribed methotrexate, which she declined due to concerns about side effects.
Her medical history was unremarkable, with no prior systemic inflammatory diseases, significant infections, or chronic illnesses.
Her father had a history of psoriasis, raising suspicion for psoriatic arthritis.
Examination revealed erythema and swelling localized to the fingertips, with no other psoriatic skin lesions or arthritic signs beyond the digital involvement.
Blood tests, including inflammatory markers, were normal, excluding systemic inflammatory arthritis. HLA-B27 testing was not performed.
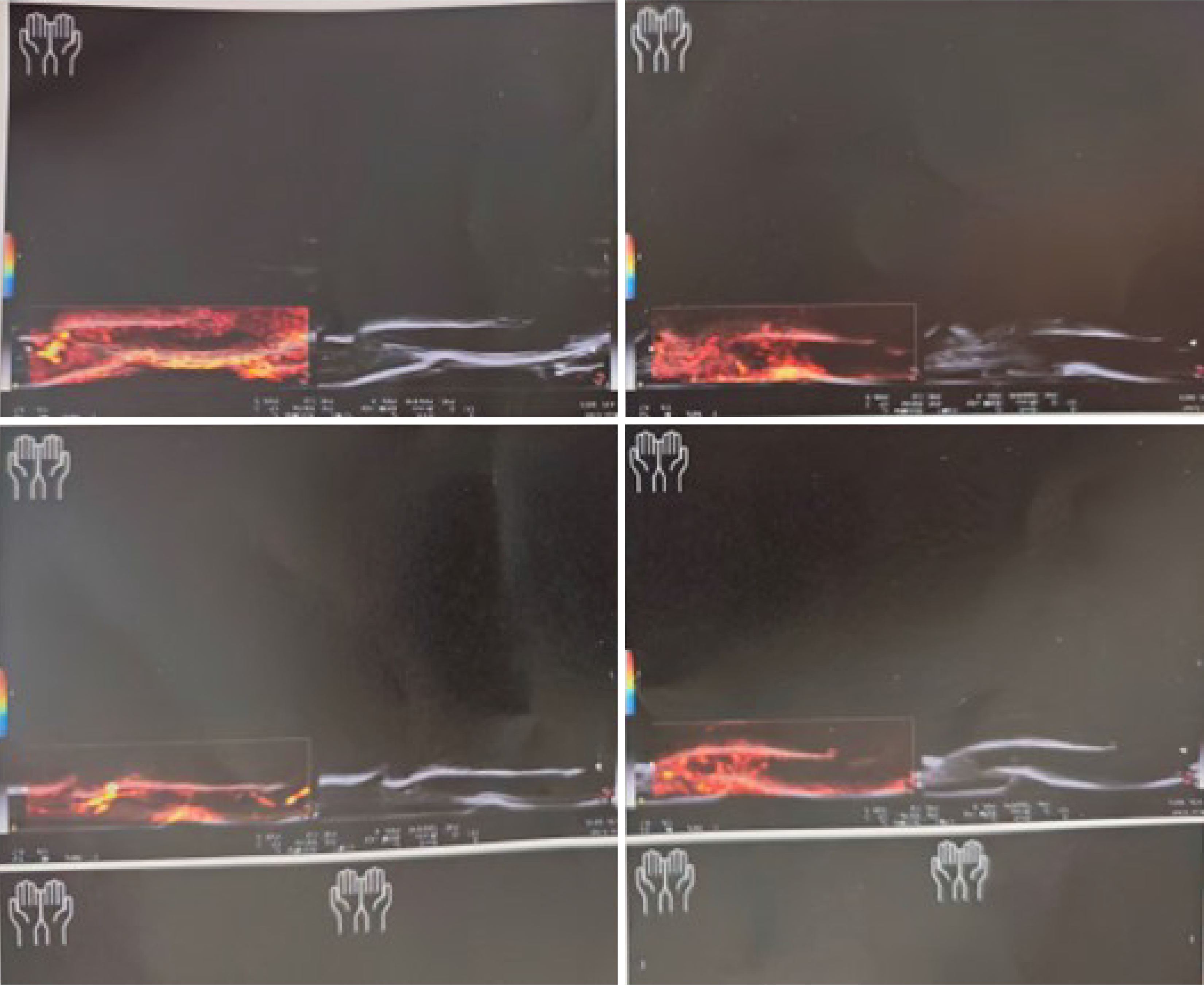
Hand and wrist X-rays showed no erosions or features typical of psoriatic arthritis. However, an ultrasound examination reported enthesitis with positive Doppler signals (Figure 2), a finding commonly associated with psoriatic arthritis but also seen in other conditions[3,4].
The final diagnosis is paronychia, confirmed by dermatological examination.
The patient was treated with fluconazole and ceftriaxone to address suspected bacterial and fungal pathogens.
The patient showed significant improvement, with resolution of symptoms after antimicrobial therapy.
This case highlights the importance of a cautious and comprehensive diagnostic approach. While a family history of psoriasis increases the index of suspicion for psoriatic arthritis, it is crucial to consider other diagnostic elements such as the CASPAR criteria for psoriatic arthritis, laboratory findings, and the presence or absence of characteristic skin or nail psoriatic lesions. The absence of radiographic changes, systemic inflammatory markers, and progression of joint involvement helped rule out psoriatic arthritis.
Paronychia can be due to bacterial, fungal, or mixed infections and may also result from underlying conditions such as diabetes, adverse drug reactions, or psoriasis. In cases of multifinger involvement, as seen here, one should carefully consider systemic factors. Despite the family history of psoriasis, our patient’s presentation and laboratory findings did not support psoriatic arthritis. Instead, the clinical and therapeutic response strongly pointed towards an infectious etiology.
The empirical use of fluconazole alongside ceftriaxone was guided by dermatological consultation. Some cases of persistent paronychia may involve fungal colonization, especially when multiple digits are affected and the response to standard antibacterial treatment is uncertain. While fluconazole is typically reserved for confirmed fungal infections, it was chosen here to address the possibility of a fungal component. This approach led to rapid improvement, reinforcing the diagnosis of an infectious rather than inflammatory arthritic process.
Ultimately, a multidisciplinary approach involving rheumatologists and dermatologists is key to distinguishing between psoriatic arthritis and mimickers like paronychia[5] By carefully evaluating clinical, laboratory, and imaging findings, and considering underlying conditions that could lead to multifocal paronychia, clinicians can avoid misdiagnosis and unnecessary exposure to immunosuppressive therapy.
This case underscores the need for thorough clinical evaluation and caution in interpreting nonspecific imaging findings, especially in patients with a family history of psoriasis. While familial predisposition may raise suspicion for psoriatic arthritis, it is essential to integrate laboratory data, imaging studies, and clinical presentation, including response to targeted antimicrobial therapy. A multidisciplinary approach, involving both rheumatologists and dermatologists, is crucial to preventing misdiagnosis, ensuring appropriate treatment, and avoiding the potential harms of unwarranted therapies.
| 1. | van de Kerkhof PC. From Empirical to Pathogenesis-Based Treatments for Psoriasis. J Invest Dermatol. 2022;142:1778-1785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 2. | Lee DK, Lipner SR. Optimal diagnosis and management of common nail disorders. Ann Med. 2022;54:694-712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 56] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 3. | Kehl AS, Corr M, Weisman MH. Review: Enthesitis: New Insights Into Pathogenesis, Diagnostic Modalities, and Treatment. Arthritis Rheumatol. 2016;68:312-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 119] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 4. | Visalli E, Crispino N, Foti R. Multidisciplinary Management of Psoriatic Arthritis: The Benefits of a Comprehensive Approach. Adv Ther. 2019;36:806-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Zhou C, Yu G, Wang Q, Yang Z, Wang H, Zhao Y. Global trends and hotspots in research of paronychia: A bibliometric analysis. Medicine (Baltimore). 2024;103:e39838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/