Published online Jun 16, 2025. doi: 10.12998/wjcc.v13.i17.102207
Revised: January 13, 2025
Accepted: January 21, 2025
Published online: June 16, 2025
Processing time: 129 Days and 16.2 Hours
Pertussis is an acute respiratory infectious disease caused by Bordetella pertussis. Although the diphtheria-pertussis-tetanus vaccine is widely administered, there are still a number of patients with severe pertussis each year, which can lead to death, especially in infants and young children. Hyperleukocytosis is a factor related to the severity of pertussis and a risk factor for death. Reducing the leuko
Two children with pertussis with cough as the initial symptom, developed pneumonia during the course of the illness. White blood cell counts were significantly increased with the highest values of 87.34 × 109/L and 55.46 × 109/L. Following anti-infection, plasma exchange, and ventilator treatment, both children recovered.
Early identification of children with pertussis complicated with hyperleukocytosis and timely plasma exchange can improve the prognosis and reduce mortality.
Core Tip: Hyperleukocytosis associated with pertussis is a serious condition associated with a high mortality rate. Timely application of relevant antibiotics, ventilator therapy and plasma exchange improve outcomes and reduces mortality. Plasma exchange plays a crucial role in decreasing the white blood cell count in pediatric patients with pertussis-induced hyperleukocytosis. A thorough evaluation of the child’s white blood cell count, circulatory status, and respiratory function is essential, and the timing of plasma exchange should be meticulously assessed.
- Citation: Han HW, Wang XX, Wang Y, Zhang WH. Hyperleukocytosis associated with pertussis: Two case reports. World J Clin Cases 2025; 13(17): 102207
- URL: https://www.wjgnet.com/2307-8960/full/v13/i17/102207.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i17.102207
Pertussis is an acute respiratory infectious disease caused by Bordetella pertussis. It is characterized by a paroxysmal spasmodic cough followed by a prolonged inspiratory whooping sound, which can last for one to two months or even longer. Patients with severe pertussis may experience complications such as frequent apnea, severe pneumonia, hyperleukocytosis, pulmonary hypertension, and potentially fatal outcomes[1]. Recent surveillance data indicate that children, particularly infants under the age of 1 year, have a high incidence of pertussis. Severe cases and fatalities are predominantly observed in this age group[1,2]. Our hospital recently admitted two children with pertussis complicated by hyperleukocytosis. Despite anti-infective treatment showing limited efficacy, plasma exchange successfully normalized the white blood cell (WBC) count and significantly alleviated clinical symptoms. This case report aims to provide insights into the diagnosis and treatment of children with pertussis complicated by hyperleukocytosis as a reference for managing similar cases and improving treatment success rates.
Case 1: A 4-month-old girl was admitted to our hospital with cough persisting for fourteen days (August 6, 2023 to August 19, 2023) and worsening for two days.
Case 2: A 2-month-old girl was admitted to our hospital due to cough for ten days (August 15, 2023 to August 24, 2023) and aggravated for four days.
Case 1: Eight days ago, the child was hospitalized in our department with a positive DNA test for pertussis. The patient was diagnosed with pertussis and underwent a six-days treatment course of erythromycin.
Case 2: The patient presented with vomiting, airway obstruction, cyanosis, and facial flushing during coughing for ten days, without fever, loss of consciousness, or seizures. She had received a course of cephalosporin therapy for one week at another hospital.
Case 1: The patient was gestation 3 parity 3, delivered at term via cesarean section with a birth weight of 2800 g. Her postnatal condition was normal without any history of asphyxia or resuscitation. Breastfeeding was initiated at birth and her growth and development history were similar to normal children of the same age.
Case 2: The patient was gestation 2 parity 2, delivered by cesarean section at full term, weighing 3850 g at birth, with a normal postnatal course. She was breastfed from birth and her growth and development were similar to that of normal children of the same age.
Family history of genetic disease was negative in both cases.
Case 1: Physical examination revealed the following: Temperature: 36.4 °C; pulse rate: 152 beats/minute; respiration: 36 breaths/minute; weight: 7.5 kg. The patient exhibited clear consciousness and good mental responsiveness. The fontanelle appeared flat and soft, while the three depressions sign was negative. Coarse breath sounds were detected in both lungs along with fine moist rales audible upon auscultation. Abdominal examination yielded unremarkable findings.
Case 2: Physical examination revealed the following: Temperature: 37.1 °C; pulse rate: 150 beats/minute; respiration: 40 breaths/minute; weight: 6.2 kg. She was alert and had a fair response to stimuli. The fontanelle was flat and soft. Nasal airflow was obstructed, and there was some nasal secretion visible. There was no nasal flaring. The three depressions sign was negative. Bilateral lung breath sounds were rough, with occasional rales audible. Fine moist rales were audible. Cardiac and abdominal examinations were unremarkable.
Case 1: Upon admission, the WBC count was 31.69 × 109/L, neutrophil count was 7.54 × 109/L, lymphocyte count was 21.7 × 109/L, red blood cell count was 3.79 × 1012/L, hemoglobin level was 105 g/L, and the platelet count was 782 × 109/L. Pertussis DNA was positive, and Mycoplasma pneumoniae DNA in the lavage fluid measured 1.37 × 107 copies/mL.
Case 2: Laboratory tests showed that the WBC count was 20.15 × 109/L, neutrophil count was 4.43 × 109/L, lymphocyte count was 14.55 × 109/L, red blood cell count was 4.1 × 1012/L, hemoglobin level was 127 g/L, and platelet count was 319 × 109/L. Pertussis DNA was positive.
Case 1: Chest imaging demonstrated evident pulmonary exudation prompting electronic bronchoscopy and lavage on day 3.
Case 2: Chest imaging showed patchy shadows in both lungs and effusion in the left pleural space on day 6.
The final diagnoses were acute respiratory failure, severe pertussis pneumonia, and Mycoplasma pneumoniae pneumonia.
The final diagnoses were acute respiratory failure and severe pertussis pneumonia.
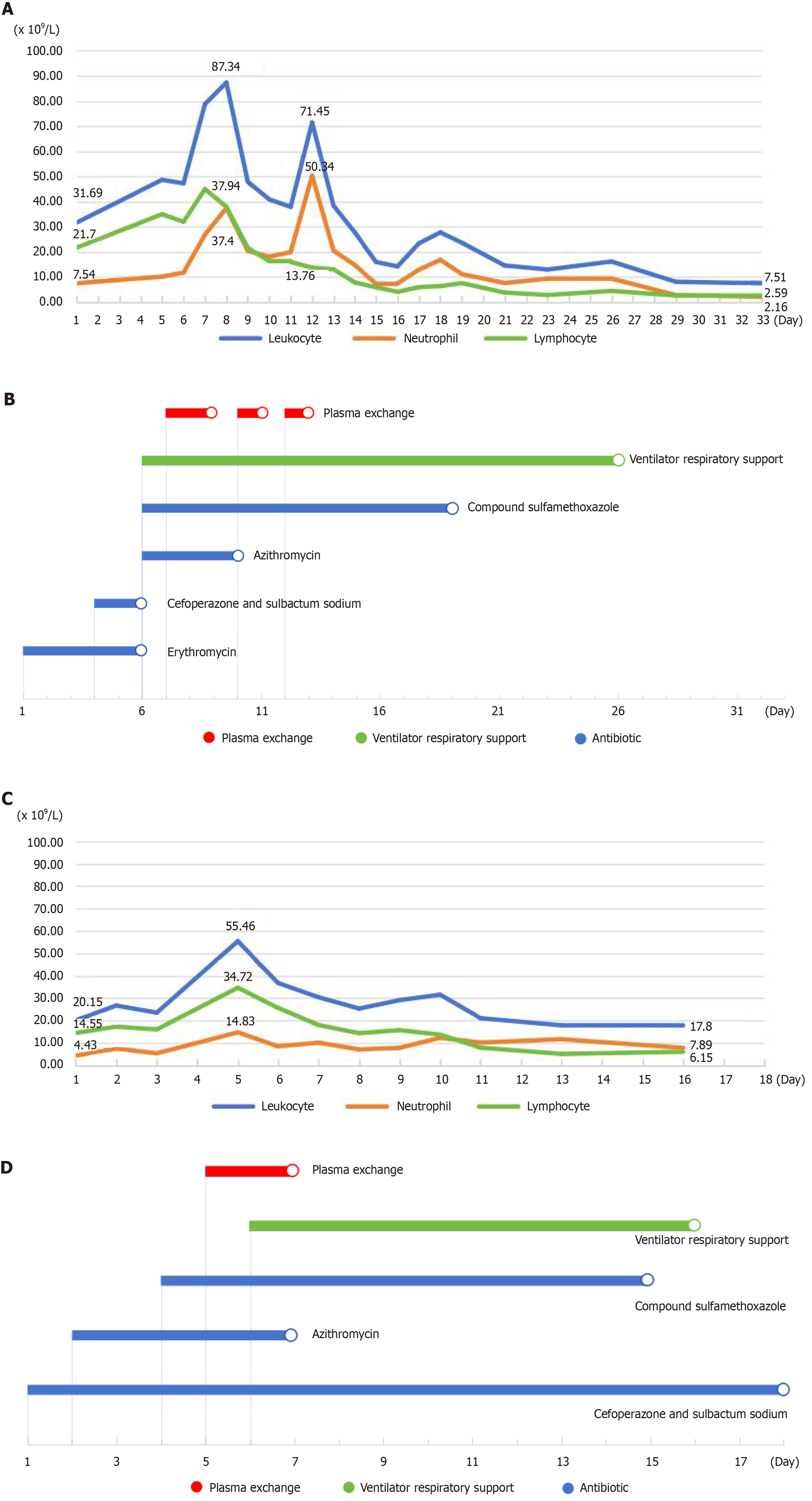
Following admission, erythromycin therapy was continued for anti-infection. On day 4 after admission, the patient’s cough was not significantly alleviated, and transient fever occurred reaching a peak temperature of 37.7 °C. To prevent infection, cefoperazone sulbactum sodium was added to the treatment regimen. Electronic bronchoscopy and lavage were performed on day 3. On day 6, she developed tachypnea (50-60 breaths/minute), the three depressions sign was positive, she had a severe cough, and a significant increase in WBC count to 47.26 × 109/L. She was transferred to the pediatric intensive care unit and received ventilator respiratory support, azithromycin, and compound sulfamethoxazole tablets for anti-infection treatment. On day 7, the first plasma exchange therapy was performed with a plasma volume of 300 mL, blood flow rate ranged from 40-80 mL/minute, total exchange volume of 300 mL/hour, replacement fluid rate of 150 mL/hour, and heparin sodium infusion rate was 2 mL/hour (5 U/kg/hour). The WBC count decreased to 57.91 × 109/L. On day 8, the second plasma exchange treatment was conducted with the same parameters as before. The WBC count increased to 87.34 × 109/L. On day 9 the WBC count was 47.91 × 109/L, on day 10 the WBC count dropped to 40.89 × 109/L, on day 11 the WBC count was 37.92 × 109/L, on day 12 the WBC count increased to 71.45 × 109/L, and the fourth plasmapheresis procedure took place on day 13 after which the WBC count decreased to 38.37 × 109/L. On day 15 the WBC count reached 16.01 × 109/L. The patient’s temperature and circulation were stable, and her cough was subdued. Thus, the ventilator was removed on day 26. The full blood count (FBC) change and therapeutic process are shown in Figure 1A and B.
After admission, cefoperazone sulbactam sodium was given for anti-infection. On day 2, her cough was not relieved and azithromycin was given for anti-infection. On day 4, the cough worsened, and compound sulfamethoxazole tablets were given for anti-infective treatment. On day 5, the WBC count was 55.46 × 109/L, and plasma exchange was performed. The blood flow rate was 40-70 mL/minute, the total amount of exchange was 280 mL/hour, the replacement fluid was 140 mL/hour, and the heparin sodium infusion rate was 2 mL/hour (5 U/kg/hour). On day 6, the WBC count was 36.82 × 109/L, and chest imaging showed lesions in the upper field of the right lung, large patchy shadows in the left lung field, and left pleural effusion. Plasma exchange therapy was performed again, and the plasma volume, blood flow rate, and total amount of exchange were the same as before. The patient had dyspnea, cyanosis, the three depressions sign was positive, and decreased heart rate and peripheral capillary oxygen saturation (SpO2). The heart rate decreased to 68 beats/min and SpO2 decreased to 85%. Invasive assisted ventilation was given. The WBC count was 30.45 × 109/L on day 7. On the day 16, the WBC count was 17.80 × 109/L, lymphocyte count was 6.15 × 109/L, and neutrophil count was 7.89 × 109/L, with a significant decrease in the WBC count compared with the previous measurements. The child’s SpO2 was maintained above 96% under invasive assisted ventilation, and the ventilator was removed. The FBC change and therapeutic process are shown in Figure 1C and D.
The patient was discharged on September 20, 2023 following an improvement in her condition. The duration of hospitalization was thirty-three days. At the time of discharge, she presented with occasional coughing episodes that were alleviated after 2-3 coughs. One-week post-discharge, the child continued to experience intermittent coughing but had significant improvement compared to that at the time of discharge. Routine blood analysis revealed normal WBC, neutrophil and lymphocyte counts.
The patient was hospitalized for a total of eighteen days. At the time of discharge, the patient’s SpO2 was maintained above 96%, and her cough was significantly relieved with 2-3 coughs each time. One week after discharge, the child had occasional cough, which was significantly relieved compared with that at discharge. The WBC, neutrophil and lymphocyte counts in the FBC were all normal.
Case 1 and case 2 were followed up for three months and six months after discharge, respectively. Routine blood counts were normal, with no cough or expectoration, and both growth and development were normal.
Typical pertussis is characterized by a paroxysmal spastic cough, cough ending in a whistle-like inspiratory roar, and peripheral lymphocytosis. It is divided into three stages, the catarrhal stage is characterized by symptoms of upper respiratory tract infection such as rhinorrhea, sneezing, tears, sore throat, and paroxysmal cough. The spasmotic cough stage is characterized by a paroxysmal spastic cough with inspiratory roar at the end of a cough, which is repeated many times, and the spastic cough is more prominent during sleep. During the recovery period, spasticity is gradually relieved, cough intensity is weakened, the number of attacks is reduced, and the whooping sound gradually disappears. Since the 1980s, “pertussis resurgences” (epidemics and local outbreaks of pertussis) have gradually occurred in some countries with high pertussis vaccination rates. This condition is more common in children under one year of age, especially in infants under six months of age, which poses great harm to children and may even be life-threatening. In recent years, the pertussis epidemic has also rebounded sharply in some provinces in China. From 2018 to 2022, the incidence of pertussis in China was 0.32-2.71/100000, with 52.40% of infants under one year old, 13.01% of children aged five-nine years, and 2.49% of children and adults aged ≥ ten years[3]. Macrolide antibiotics are often used for mild pertussis. Given the high resistance rate of Bordetella pertussis to macrolides in China, children and adults older than two months can be given trimethoprim sulfamethoxazole if they have contraindications to macrolides, cannot tolerate macrolides or are infected with macrolide-resistant strains. For infants under two months of age, cefoperazone sulbactam sodium and piperacillin tazobactam can be used for treatment[4].
Most children with severe pertussis have pertussis pneumonia, which may also be complicated by atelectasis, pneumothorax, mediastinal emphysema, subcutaneous emphysema, pulmonary hypertension, asphyxia and encephalopathy[5]. Hyperleukocytosis is an independent risk factor for severe pertussis and death[6,7]. The levels of WBCs and lymphocytes in children with severe pertussis are significantly higher than those in children without pertussis, which can reflect the severity of the disease to a certain extent and can indicate the severity of pertussis. At present, the mechanism of hyper
The abnormal increase in WBCs in children with pertussis and their accumulation in the lungs can lead to local microcirculation obstruction in the lungs, which can cause pulmonary hypertension, and this may lead to respiratory failure and heart failure. It has been reported that pathological examination of lung tissue from infants who died of pertussis showed that a large number of immature WBCs accumulated in small arteries, veins and lymphatic vessels of the lungs[9]. Therefore, it is necessary to ensure that cardiac ultrasound examination is routine for pertussis complicated with hyperleukocytosis, in order to be alert to the occurrence of pulmonary hypertension.
For children with pertussis complicated with hyperleukocytosis, WBCs should be reduced as soon as possible, which will avoid or reduce pulmonary hypertension, help improve hypoxemia, and slow or prevent the disease from pro
In recent years, the importance of plasma exchange in the treatment of pertussis complicated with hyperleukocytosis has been increasingly recognized. Plasma exchange can remove the aggregated WBCs in blood vessels, reduce blood viscosity, reduce the obstruction of small pulmonary vessels caused by WBCs, and greatly reduce the level of pertussis toxin in circulation, thereby preventing the occurrence or progression of pulmonary hypertension. It is helpful to maintain hemodynamic stability[13]. At present, there is no unified standard for the indication of plasma exchange for severe pertussis, which is generally based on the level of WBCs, the rate of disease progression, and organ function[14]. Rowlands et al[10] in 2010 believed that WBCs > 100 × 109/L, or WBCs > 70 × 109/L, accompanied by pulmonary hypertension and cardiopulmonary failure, were the indications for emergency plasma exchange in children with pertussis within three months of age without extracorporeal membrane oxygenation treatment indications. Plasma exchange should be considered when WBCs were > 50 × 109/L. Nieves et al[15] suggested that plasma exchange therapy should be initiated in children with pertussis within four months of age, when WBCs increased rapidly to 30 × 109/L, accompanied by pulmonary hypertension, early onset pneumonia, pulse rate ≥ 170 beats/min and respiratory rate ≥ 70 beats/minute. According to the Chinese Guidelines for the diagnosis, treatment and prevention of pertussis (2024 edition), plasma exchange is not recommended for children with severe pertussis and hyperleukocytosis. However, for infants with severe pertussis, if the peripheral WBC count is ≥ 50 × 109/L, or ≥ 30 × 109/L and progressively increased with aggravation of the disease, pulmonary hypertension or heart and lung dysfunction occur, plasma exchange may be necessary according to the specific conditions of the child and the judgment of the physician, On the basis of shared decision-making between doctors and patients, plasma exchange therapy can be considered in the early stage of pulmonary hypertension or heart or lung failure[3].
In case 1 described in this report, the patient had a long course of disease with an obvious spastic cough phase, which was consistent with the clinical characteristics of infantile pertussis. On admission, the child’s WBC count was 31.69 × 109/L, which met the diagnostic criteria for hyperleukocytosis. On day 8, the WBC count reached the highest level of 87.34 × 109/L. Plasma exchange was performed timely and repeatedly, and the WBC count gradually decreased after the fourth plasma exchange. It is worth noting that the WBCs increased sharply and the ratio of neutrophils to lymphocytes reversed from 0.34 to 3.65, and the patient’s condition was significantly aggravated. This is consistent with the current research report that the inversion of the ratio of granulocytes to lymphocytes in children with severe pertussis and hyperleukocytosis indicates that the condition is critical[16]. According to a literature analysis, the reason for this may be that pertussis is secondary to other bacterial infections, such as bacterial pneumonia, or hospital-related nosocomial infection in the intensive care unit[17]. In this case, blood culture suggested Staphylococcus haemolyticus infection, and co-infection was considered. At this time, the compound sulfamethoxazole used in the treatment of pertussis also had a good antibacterial effect on this bacterium. Following active treatment, the patient’s condition improved and she finally recovered. Case 2 had a WBC count of 36.82 × 109/L, and on day 6 chest imaging showed patchy shadows in both lungs and effusion in the left pleural space. These also met the conditions for plasma exchange therapy mentioned above; therefore, timely plasma exchange therapy was carried out. After active symptomatic treatment, the child recovered well, and was cured at follow-up. The successful treatment of these two children was based on the application and adjustment of relevant antibiotics, and assisted ventilation and plasma exchange to stabilize the pulmonary circulation. Using the above treatment methods, cough symptoms in these children were relieved, the WBC count was reduced, and time was gained for the treatment of other complications.
Hyperleukocytosis is an important complication of severe pertussis and a risk factor for poor prognosis. It is safe and effective to use plasma exchange to reduce WBC s and improve the survival rate of critically ill children. As pediatricians have a deeper understanding of plasma exchange in the treatment of severe pertussis, there will be more relevant reports, which will also help to improve the treatment and prognosis of children with severe pertussis.
| 1. | Skoff TH, Hadler S, Hariri S. The Epidemiology of Nationally Reported Pertussis in the United States, 2000-2016. Clin Infect Dis. 2019;68:1634-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Gil-Prieto R, Walter S, San-Román-Montero J, Marín-García P, González-Escalada A, Gil-de-Miguel A. Paediatric hospitalizations due to whooping cough in Spain (1997-2017). Vaccine. 2019;37:6342-6347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Pediatric Infection Group, Chinese Society of Infectious Diseases; Chinese Medical Association; Infection Group, Pediatric Expert Committee of National Health Commission Capacity Building and Continuing Education; China Clinical Practice Guidelines Alliance Methodology Committee; National Children′s Medical Center (Shanghai); National Medical Center for Infectious Diseases. [Guidelines for diagnosis and management and prevention of pertussis of China (2024 edition)]. Zhonghua Yi Xue Za Zhi. 2024;104:1258-1279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 4. | Shi W, Meng Q, Hu Y, Yao K. Modifying antibiotic treatment strategies in the face of pertussis surge associated to erythromycin resistance in China. J Infect. 2024;88:106174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Jia J, Yuan L, Gao W, Yao KH. [Complications of pertussis]. Zhongguo Dang Dai Er Ke Za Zhi. 2019;21:713-717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 6. | Winter K, Zipprich J, Harriman K, Murray EL, Gornbein J, Hammer SJ, Yeganeh N, Adachi K, Cherry JD. Risk Factors Associated With Infant Deaths From Pertussis: A Case-Control Study. Clin Infect Dis. 2015;61:1099-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 97] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 7. | Palvo F, Fabro AT, Cervi MC, Aragon DC, Ramalho FS, Carlotti APCP. Severe pertussis infection: A clinicopathological study. Medicine (Baltimore). 2017;96:e8823. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Scanlon K, Skerry C, Carbonetti N. Association of Pertussis Toxin with Severe Pertussis Disease. Toxins (Basel). 2019;11:373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 58] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Paddock CD, Sanden GN, Cherry JD, Gal AA, Langston C, Tatti KM, Wu KH, Goldsmith CS, Greer PW, Montague JL, Eliason MT, Holman RC, Guarner J, Shieh WJ, Zaki SR. Pathology and pathogenesis of fatal Bordetella pertussis infection in infants. Clin Infect Dis. 2008;47:328-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 251] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 10. | Rowlands HE, Goldman AP, Harrington K, Karimova A, Brierley J, Cross N, Skellett S, Peters MJ. Impact of rapid leukodepletion on the outcome of severe clinical pertussis in young infants. Pediatrics. 2010;126:e816-e827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Kuperman A, Hoffmann Y, Glikman D, Dabbah H, Zonis Z. Severe pertussis and hyperleukocytosis: is it time to change for exchange? Transfusion. 2014;54:1630-1633. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Oñoro G, Salido AG, Martínez IM, Cabeza B, Gillén M, de Azagra AM. Leukoreduction in patients with severe pertussis with hyperleukocytosis. Pediatr Infect Dis J. 2012;31:873-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Al Hanshi S, Al Ghafri M, Al Ismaili S. Severe Pertussis Pneumonia managed with Exchange Transfusion. Oman Med J. 2014;29:e074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Shi T, Du S, Fan H, Yu M, Jiang W, Zhang D, Ding T, Lu G, Huang L. Risk Factors of Exchange Blood Transfusion in Infants With Severe Pertussis. Clin Pediatr (Phila). 2023;62:1245-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Nieves D, Bradley JS, Gargas J, Mason WH, Lehman D, Lehman SM, Murray EL, Harriman K, Cherry JD. Exchange blood transfusion in the management of severe pertussis in young infants. Pediatr Infect Dis J. 2013;32:698-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Ganeshalingham A, McSharry B, Anderson B, Grant C, Beca J. Identifying Children at Risk of Malignant Bordetella pertussis Infection. Pediatr Crit Care Med. 2017;18:e42-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Kazantzi MS, Prezerakou A, Kalamitsou SN, Ilia S, Kalabalikis PK, Papadatos J, Sdougka MM, Briassoulis G, Tsolia MN. Characteristics of Bordetella pertussis infection among infantsand children admitted to paediatric intensive care units in Greece: A multicentre, 11-year study. J Paediatr Child Health. 2017;53:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/