Published online May 6, 2025. doi: 10.12998/wjcc.v13.i13.102457
Revised: December 5, 2024
Accepted: December 27, 2024
Published online: May 6, 2025
Processing time: 85 Days and 10.4 Hours
This case report examines the challenges associated with removing a totally implantable venous access port (TIVAP) used for long-term chemotherapy in a patient with breast cancer. Prolonged use of TIVAPs can result in complications such as catheter kinking, thrombosis, and adhesions between the catheter and surrounding tissues, potentially complicating their removal.
A breast cancer patient with bone metastasis presented with difficulty aspirating blood from a TIVAP that had been placed in the right internal jugular vein for 3 years. Initial removal attempts at the Department of Venous Access Center were unsuccessful, likely due to adhesions, necessitating a subsequent successful catheter extraction in a hybrid operating room. Imaging revealed no abnor
This case highlights the challenges of removing TIVAPs inserted via the internal jugular vein, particularly when the catheter traverses the sternocleidomastoid muscle. Repeated neck movements might lead to significant adhesions around the catheter, complicating its removal. Careful consideration should be given during catheter placement to avoid muscle-related adhesions and facilitate smoother extraction in long-term use.
Core Tip: Totally implantable venous access ports (TIVAPs) are an effective catheterization method for patients with cancer, offering safe, convenient, and cosmetically long-term vascular access. This case highlights the complications that could arise from prolonged TIVAP use. For patients with TIVAPs inserted via the internal jugular vein, careful consideration of catheter placement is essential. Avoiding passage through active muscles, such as the sternocleidomastoid, might reduce the risk of adhesions and facilitate easier catheter removal.
- Citation: Chen J, Tang M, Han QY, Tang L, Yu TH, Zhao YP, He CW. Difficulty removing a totally implantable venous access port: A case report. World J Clin Cases 2025; 13(13): 102457
- URL: https://www.wjgnet.com/2307-8960/full/v13/i13/102457.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i13.102457
Totally implantable venous access port (TIVAP) was first demonstrated to the public in 1982, when Niederhuber et al[1] at Monroe D Anderson Cancer Center in the United States, used surgical techniques to place a fully implantable venous port through the cephalic vein into the central vein. In 1992, Morris et al[2] pioneered using radiology-assisted techniques for implantable subcutaneous infusion ports. Compared to other central venous line placement methods, TIVAPs are preferred for intravenous infusion in patients undergoing chemotherapy due to their advantages, including the avoidance of repeated punctures, safe infusion, extended placement duration, and low complication rate. In addition to providing adequate vascular access, TIVAPs enhance patient care and improve quality of life[3]. For infusions exceeding 3 months, intravenous port placement is recommended.
TIVAPs are typically removed at the end of treatment or when they are no longer clinically necessary. Removal might also be required in the presence of complications, such as TIVAP infection, rejection reactions, injection port infections, catheter rupture, catheter fracture, blockage, or displacement[4]. While most TIVAPs are removed easily in procedures referred to as “simple removals”, complications could lead to “difficult removals”[5]. Challenges in difficult removals might include requiring greater traction than usual, using a guidewire to extract the port and catheter, performing a secondary neck incision, or failing to remove the despite these measures. This case involves a breast cancer patient with bone metastasis who had a venous port implanted in the right internal jugular vein (IJV) for 3 years. A specialized nurse experienced difficulty aspirating blood from the venous port, prompting a recommendation for its removal. Conventional extraction methods were ineffective in retrieving the catheter from the vascular lumen. Ultimately, with assistance from vascular surgery, the catheter was successfully removed in hybrid operating room.
A specialized nurse was unable to aspirate blood from the TIVAP of a breast cancer patient with bone metastasis.
A breast cancer patient with bone metastasis presented with difficulty during intravenous infusion preparations. A specialized nurse was unable to aspirate blood from the patient’s TIVAP.
Three years prior, the patient was diagnosed with left-sided invasive ductal carcinoma of the breast and underwent right IJV, TIVAP implantation at age of 47 years. This was followed by six cycles of paclitaxel-based chemotherapy and a modified radical mastectomy of the left breast. Postoperatively, the patient received tamoxifen endocrine therapy and attended regular follow-ups every three months. The TIVAP was maintained monthly and remained in place. In the third postoperative year, thoracic vertebral bone metastasis was detected during a follow-up examination.
The patient denied any family history of malignant tumors.
The patient’s the vital signs were as follows: Body temperature, 36.4°C; blood pressure, 125/65 mmHg; heart rate, 72 beats per minute; respiratory rate, 18 breaths per minute. Examination revealed the absence of the left breast, while the right breast appeared normal in shape, size, and skin color, with no palpable masses. No lymphadenopathy was detected in the axillary or supraclavicular regions.
Serum tumor marker levels were normal. Routine blood and urine analyses revealed no abnormalities.
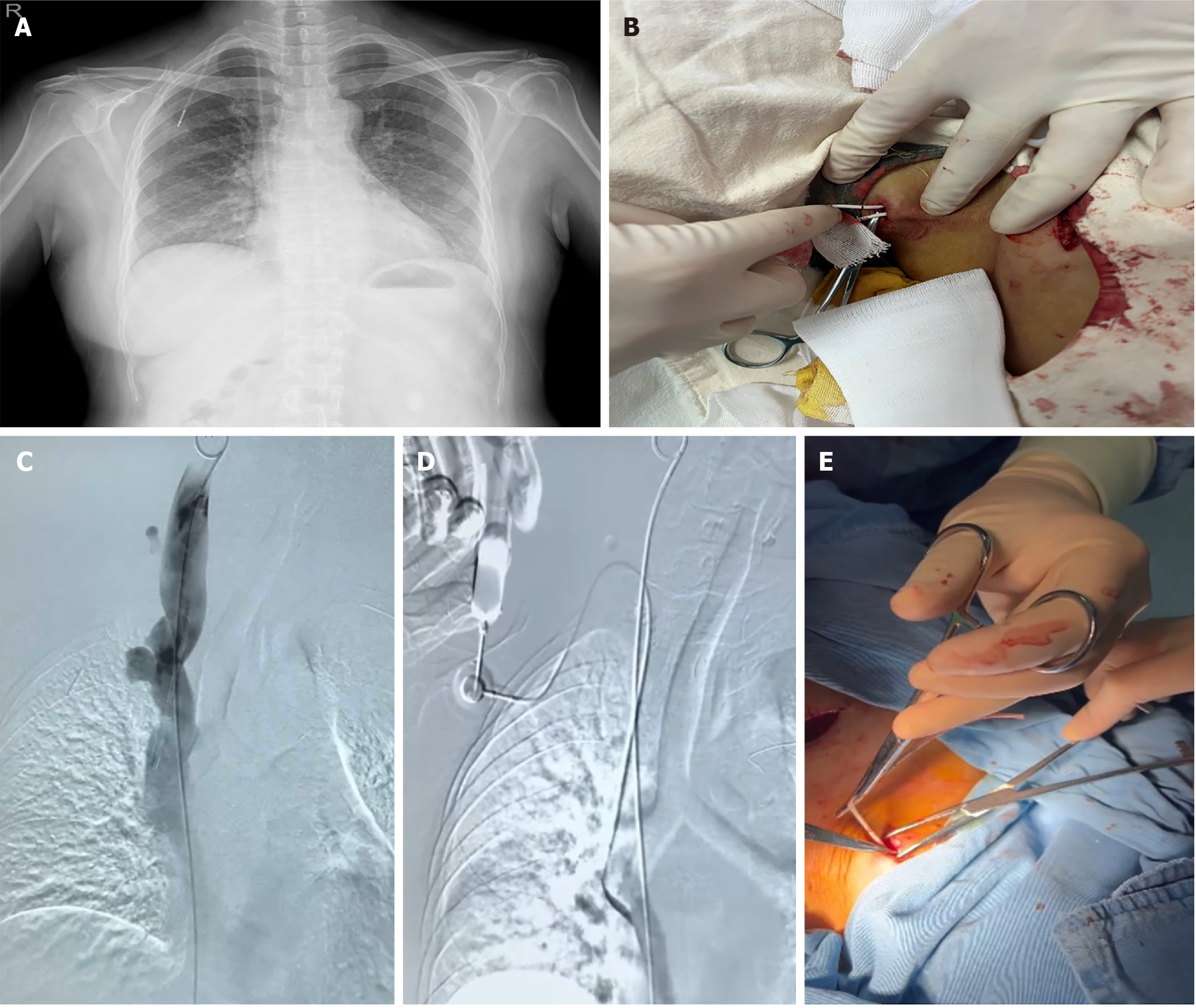
The chest computed tomography scans indicated multiple thoracic vertebral bone metastases. A preoperative chest radiograph showed no abnormalities (Figure 1A).
The patient, undergoing treatment for breast cancer bone metastasis, experienced difficulties during intravenous preparation. After connecting the Huber needle, a clinical nurse specialist was unable to aspirate blood. To address this issue, 100000 units of dissolved urokinase were injected into the catheter for thrombolysis. The nurse then repositioned the patient’s neck to relax the sternocleidomastoid muscle and assess for catheter recanalization. Based on these findings and the patient’s medical history, the final diagnosis was functional complications of the venous catheter and left breast cancer with sternal bone metastasis.
The initial plan was to retrieve the port body and catheter by making an incision along the original site at the chest wall in the Department of Vascular Access Center of Jiangxi Cancer Hospital, China. However, the catheter could not be extracted during the procedure. Considering that some hospitals secure the catheter with sutures at the neck during implantation via the IJV, a 1.5 cm neck incision was made to locate such sutures, but none were identified. The attempt to retrieve the catheter from the neck incision was unsuccessful (Figure 1B and Supplementary Video 1). Due to the absence of digital subtraction angiography at the center, which limited insight into the condition of the catheter, forcibly removing it posed risks such as IJV tearing or catheter fracture. After consulting with the patient, it was recommended that they seek treatment at the Department of Vascular Surgery the First Affiliated Hospital of Nanchang University, China. On 26 January 2024, the patient underwent venous port removal in hybrid operating room. A 5-Fr catheter sheath was inserted via the femoral vein, and a pigtail catheter was advanced with its tip positioned in the IJV. Angiography revealed no fibrin sheath, thrombus, or catheter kinking (Figure 1C and Supplementary Video 2). Contrast injection through the TIVAP also showed no abnormalities (Figure 1D and Supplementary Video 3). With no anomalies detected around the catheter, another attempt was made to extract it through the neck incision, but it remained immobile (Supplementary Video 4). Finally, using mosquito clamp, the catheter was carefully separated from the surrounding sternocleidomastoid muscle and IJV. A slight pull successfully removed the catheter (Figure 1E and Supplementary Video 4).
Two weeks post-procedure, the surgical incisions on the patient’s right neck and chest had fully healed, and neck mobility was restored to normal.
TIVAPs provide safe, convenient, cosmetic, and long-term vascular access for patients with requiring multiple infusions of highly concentrated chemotherapy drugs and chronic gastrointestinal nutrition and chronic diseases[2]. In the Department of Vascular Access Center of Jiangxi Cancer Hospital, the right IJV is the preferred site for infusion port placement due to anatomical advantages. Regardless of whether the right or left IJV is selected, patients might experience discomfort because of the proximity between the catheter and the neck muscles. However, studies indicate that the IJV approach for TIVAP implantation offers the highest success rate with the fewest intraoperative and postoperative complications[6,7].
Based on its numerous advantages, the patient in this case also opted for chemotherapy with TIVAP implantation via the right IJV approach. However, after 3 years of use, functional complications arose, characterized by the inability to aspirate blood while maintaining easy injection access- a condition affecting more than 25% of the patients[8]. When TIVAP removal became necessary, challenges in the catheter extraction were encountered. A literature review identified several potential factors contributing to the challenges associated with catheter removal: (1) Thrombus formation[9]: Thrombi might form around or at the catheter tip due to factors such as reduced venous blood flow or a hypercoagulable state. This could lead to adhesion between the catheter and the vessel, increasing resistance during removal; (2) Catheter obstruction[10]: Blockage of the catheter lumen by clots, drug deposits, or precipitated substances might result in adhesion to the vessel wall, complicating removal and impeding blood flow; (3) Infection or inflammation[11,12]: Infections or inflammation around the catheter may stimulate tissue proliferation and adhesion, making removal more difficult. Resolving the infection or inflammation is often necessary before attempting removal; (4) Catheter kinking or fracture[13,14]: Catheters might bend or fracture during the indwelling period, potentially due to catheter material, design, or patient activity. Such issues increase the difficulty of removal and might necessitate specialized tools or imaging guidance; and (5) Fibrous tissue ingrowth[15,16]: Long-term indwelling catheters can promote fibrous tissue proliferation, leading to adhesion between the catheter and adjacent tissues. The material and surface properties of the catheter influence the extent of this tissue response. In this case, the central venous catheter had been placed via a midline puncture of the IJV, with the catheter passing through the sternocleidomastoid muscle. This muscle is critical for neck movement and is highly active; repeated movements likely contributed to significant adhesions between the catheter and surrounding muscle and peripheral tissues. These adhesions complicated the catheter removal process. To minimize the risk of such complications, it is recommended to use the medial approach when puncturing the IJV for catheter placement. Specifically, the puncture should be as close as possible to the medial border of the sternocleidomastoid muscle, at the apex of the triangle formed by the clavicular head, sternal head of the sternocleidomastoid muscle, and the clavicle. This approach reduces friction between the catheter and the sternocleidomastoid muscle. In this case, using a mosquito clamp to separate the catheter from surrounding tissues facilitated smooth removal. The procedure was performed under interventional conditions with repeated confirmations to ensure the absence of thrombosis, adhesions, or other complications around the catheter.
To address these situations, healthcare professionals typically perform a comprehensive assessment, which might include ultrasound, radiographs, or other imaging techniques, accurately evaluate location and condition of the catheter within the vessel. Specialized tools, such as catheter scissors or custom catheter pullers, might be used to overcome resistance during removal. It is crucial to note that managing these challenges requires specialized medical expertise and should be carried out by experienced healthcare professionals. Furthermore, treatment approaches might vary depending on individual patient circumstances, underscoring the need for personalized management plans.
This case highlights the potential challenges associated with removing TIVAPs implanted via the IJV, particularly when the catheter passes through the sternocleidomastoid muscle. Repeated neck movements could lead to significant adhesions around the catheter, complicating its removal. It is essential to carefully consider catheter placement techniques to minimize muscle-related adhesions, thereby facilitating smoother extraction during long-term use.
| 1. | Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, Cozzi E. Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery. 1982;92:706-712. [PubMed] |
| 2. | Morris SL, Jaques PF, Mauro MA. Radiology-assisted placement of implantable subcutaneous infusion ports for long-term venous access. Radiology. 1992;184:149-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 83] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Piran S, Ngo V, McDiarmid S, Le Gal G, Petrcich W, Carrier M. Incidence and risk factors of symptomatic venous thromboembolism related to implanted ports in cancer patients. Thromb Res. 2014;133:30-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Su J, Liu L, Xie Y, Wang J. Complications associated with the removal of totally implantable venous access devices (TIVADs): a retrospective analysis of 4,954 breast cancer patients in a single institution. BMC Surg. 2024;24:324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Patel PA, Parra DA, Bath R, Amaral JG, Temple MJ, John PR, Connolly BL. IR Approaches to Difficult Removals of Totally Implanted Venous Access Port Catheters in Children: A Single-Center Experience. J Vasc Interv Radiol. 2016;27:876-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Sun Y, Zhou T, Li Y, Wang J, Jiao J, Wang H, Geng C. [Clinical application of totally implantable central venous port]. Zhonghua Wai Ke Za Zhi. 2014;52:608-611. [PubMed] |
| 7. | Wang M, Tang L, Xu R, Qin S, Zhang S. Clinical application of ultrasound-guided totally implantable venous access ports implantation via the posterior approach of the internal jugular vein. J Chin Med Assoc. 2024;87:126-130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Paleczny J, Banyś-Jafernik B, Gazurek K, Kierpieć K, Szczerba H, Zipser P. Long-term totally implantable venous access port systems--one center experience. Anaesthesiol Intensive Ther. 2013;45:215-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Zhang X, Geng C. Unsuccessful removal of a totally implantable venous access port caused by thrombosis in the left brachiocephalic vein: A case report. Medicine (Baltimore). 2019;98:e14985. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Baskin JL, Pui CH, Reiss U, Wilimas JA, Metzger ML, Ribeiro RC, Howard SC. Management of occlusion and thrombosis associated with long-term indwelling central venous catheters. Lancet. 2009;374:159-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 340] [Cited by in RCA: 303] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 11. | Lafuente Cabrero E, Terradas Robledo R, Civit Cuñado A, García Sardelli D, Hidalgo López C, Giro Formatger D, Lacueva Perez L, Esquinas López C, Tortosa Moreno A. Risk factors of catheter- associated bloodstream infection: Systematic review and meta-analysis. PLoS One. 2023;18:e0282290. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 64] [Reference Citation Analysis (0)] |
| 12. | O'Grady NP. Prevention of Central Line-Associated Bloodstream Infections. N Engl J Med. 2023;389:1121-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 53] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 13. | Erkılıç E, Aksoy M, Gümüş T, Sarı S, Kesimci E. Jugular Venous Catheterization: A Case of Knotting. Case Rep Med. 2015;2015:810346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 14. | Ko SY, Park SC, Hwang JK, Kim SD. Spontaneous fracture and migration of catheter of a totally implantable venous access port via internal jugular vein--a case report. J Cardiothorac Surg. 2016;11:50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Florescu MC, Runge J, Flora M, Nio G, Lof J, Stolze E, Fry G, Radio SJ, Foster KW. Location and structure of fibrous sheath formed after placing a tunneled hemodialysis catheter in a large pig model. J Vasc Access. 2018;19:484-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Zeiler M, Lenci FF, Agostinelli RM, Monteburini T, Marinelli R, Boccoli G, Dellabella S, Ceraudo E, Santarelli S. Malfunction of Peritoneal Catheters by Proliferation of Vascularized Fibrous Tissue. Perit Dial Int. 2015;35:490-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/