Published online May 6, 2025. doi: 10.12998/wjcc.v13.i13.102108
Revised: November 23, 2024
Accepted: December 23, 2024
Published online: May 6, 2025
Processing time: 94 Days and 12.7 Hours
Hem-o-lock clip, a versatile and reliable non-absorbable tissue clip, has gained widespread acceptance in laparoscopic surgeries for vessel ligation and tissue approximation. Its efficacy and safety have been well-documented.
This case report describes the occurrence of a bronchopleural fistula following the application of the Hem-o-lock clip for the treatment of a lobar bronchial stump after lobectomy.
This case underscores the importance of exercising caution when using the Hem-o-lock clip for the management of non-vascular tissues during thoracic surgery.
Core Tip: This case report describes the development of a bronchopleural fistula following the application of the Hem-o-lock clip to secure a lobar bronchial stump after lobectomy. The complication was managed by chest tube drainage and resolved without significant issues. This case underscores the importance of exercising caution when using the Hem-o-lock clip for non-vascular tissues in thoracic surgery.
- Citation: Li QY, Wang XL, Zhang F, Wei HT. Bronchopleural fistula following application of Hem-o-lock clip at bronchial stump after lobectomy: A case report. World J Clin Cases 2025; 13(13): 102108
- URL: https://www.wjgnet.com/2307-8960/full/v13/i13/102108.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i13.102108
Hem-o-lock clip is an non-absorbable multi-polymer clip with a locking mechanism, bow-shaped nail legs, anti-slip teeth, hinge, and boss structure, which is easy to use and reliable, while also improving the drawbacks of titanium clips such as easy cutting, easy shedding, and electrical conduction[1]. The safety and efficacy of the Hem-o-lock clip in handling vessels and tissues during laparoscopic surgeries have been confirmed[2-6]; it is also extensively used in thoracic surgery for handling pulmonary arteries and veins, bronchial arteries, and so on; it is also used to treat segmental bronchial stump and reinforce the lung tissue edge after resection. Here, we report a case in which the application of a Hem-o-lock clip to reinforce the bronchial stump during video-assisted thoracoscopic lobectomy in a lung cancer patient resulted in a bronchopleural fistula (BPF).
A 64-year-old woman presented with a chief complaint of intermittent hemoptysis for the past five months.
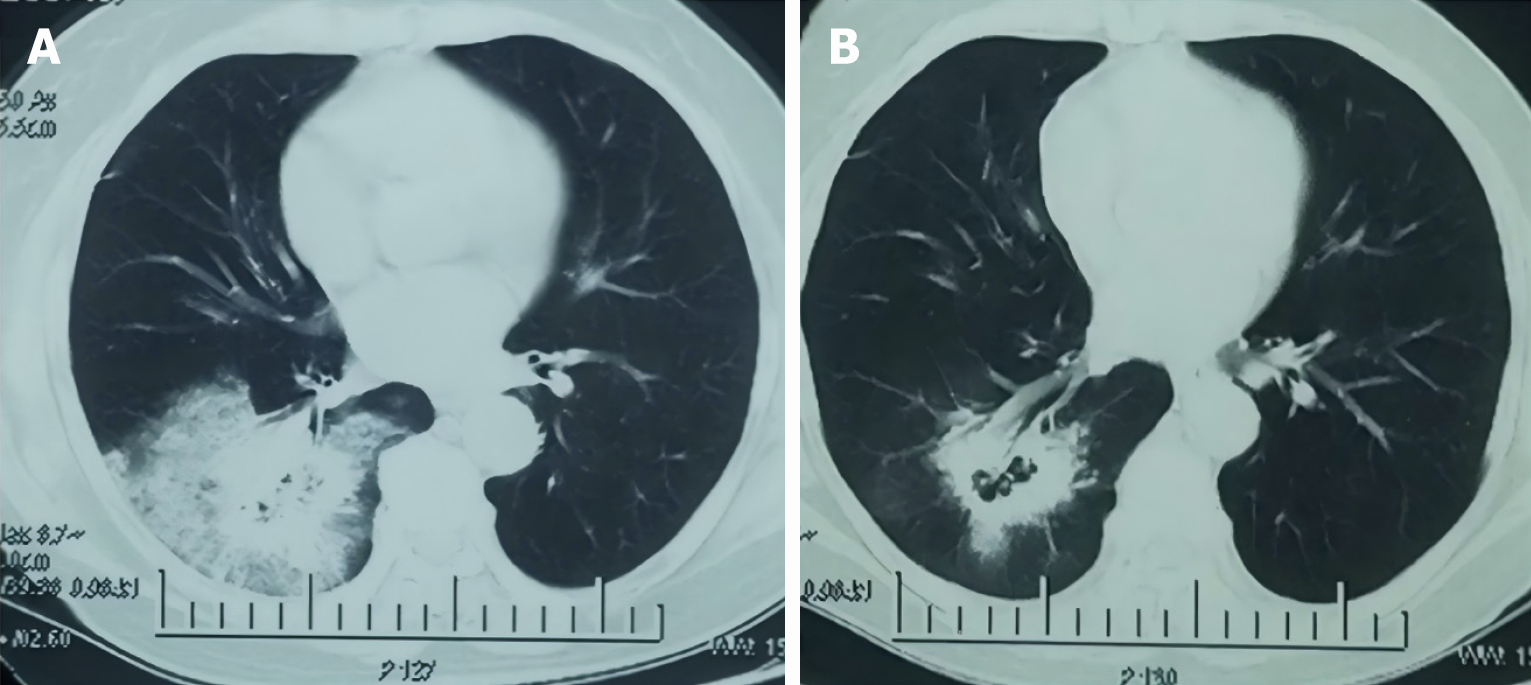
Initial symptoms included cough with bright red and blood-tinged sputum in the morning, without associated symptoms of fever, dyspnea, or chest pain. The chest computed tomography (CT) imaging revealed a mass in the lower lobe of the right lung (Figure 1). After a course of antimicrobial and hemostatic therapy with no improvement, the patient was referred to our hospital. Routine admission tests were unremarkable, with normal blood counts and procalcitonin levels, and a negative tuberculosis skin test.
The patient had a 10-year history of well-controlled diabetes mellitus. She denied any history of radiation exposure or occupational chemical exposure. There was no history of hypertension.
There were no personal or family history of the disease.
No significant abnormalities were observed upon physical examination.
Routine admission tests were unremarkable, with normal blood counts and procalcitonin levels, and a negative tuberculosis skin test.
The chest CT imaging revealed a mass in the lower lobe of the right lung (Figure 1).
The diagnosis was primarily considered a neoplasm, and bronchoscopy was unable to obtain pathological tissue. The patient refused preoperative CT-guided biopsy. After further examination, no surgical contraindications were found.
A video-assisted thoracoscopic right lower lobectomy was performed, including lymph node dissection of groups 9, 10, 11, and 12 (required intraoperatively). The intraoperative frozen pathology result revealed adenocarcinoma of the lower lobe of the right lung. Subsequent to this, the lymph node groups 2R, 4R, and 7 were dissected. Air leakage was noted at the posterior foot of the lower lobe bronchial stump, which was initially managed with a 3-0 Mersilk suture and reinforced with a Hem-o-lock clip. Two chest tubes were inserted, and the surgical incision was closed. Postoperative recovery was uneventful, and both chest tubes were removed on the third postoperative day (no air leakage, and the drainage was less than 100 mL within 24 hours).
Postoperative pathology: Invasive adenocarcinoma 0.3 cm from the bronchial margin, predominantly papillary in growth pattern, measuring 5 cm × 3 cm × 2 cm, infiltrative growth, involving the pleural membrane without penetration, and no cancer at the bronchial margin.
Lymph node status: 2R (0/8), 4R (0/2), 7 (0/1), 10 (3/7), 11 (0/1), 12 (0/1).
Pathological stage: PT2aN0M0, 8th edition.
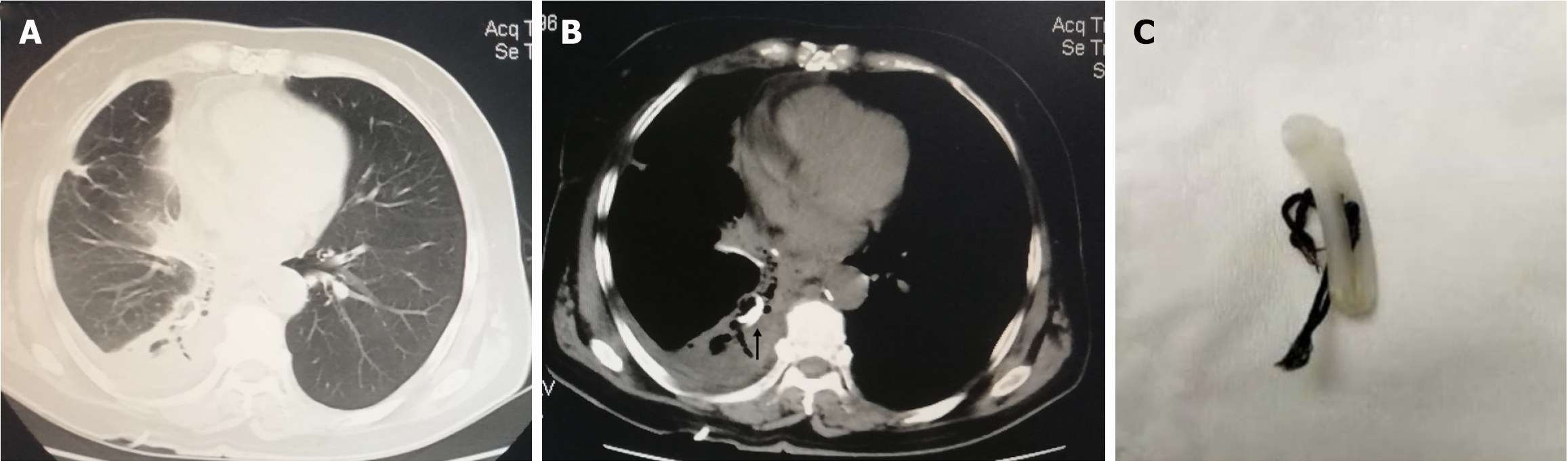
On the 6th postoperative day, the patient developed a dry cough, excluding infection, asthma, and post-nasal drip syndrome, which could be relieved with oral non-opioid cough suppressants. Thus, persistent postoperative cough was considered. The patient was discharged on the 7th postoperative day. On the 10th postoperative day, she experienced a severe cough in the morning, followed by coughing out the Hem-o-lock clip (Figure 2), prompting urgent re-admission.
Vital signs were stable, there was no subcutaneous emphysema, and chest CT showed local hydropneumothorax on the right side. Fiberoptic bronchoscopy identified a fistula orifice of approximately 3 mm. Under color Doppler ultrasound guidance, a pigtail catheter was inserted to drain a small amount of slightly turbid pleural effusion (Figure 2). No bacterial growth was detected in the culture, and pleural lavage was performed to prevent infection.
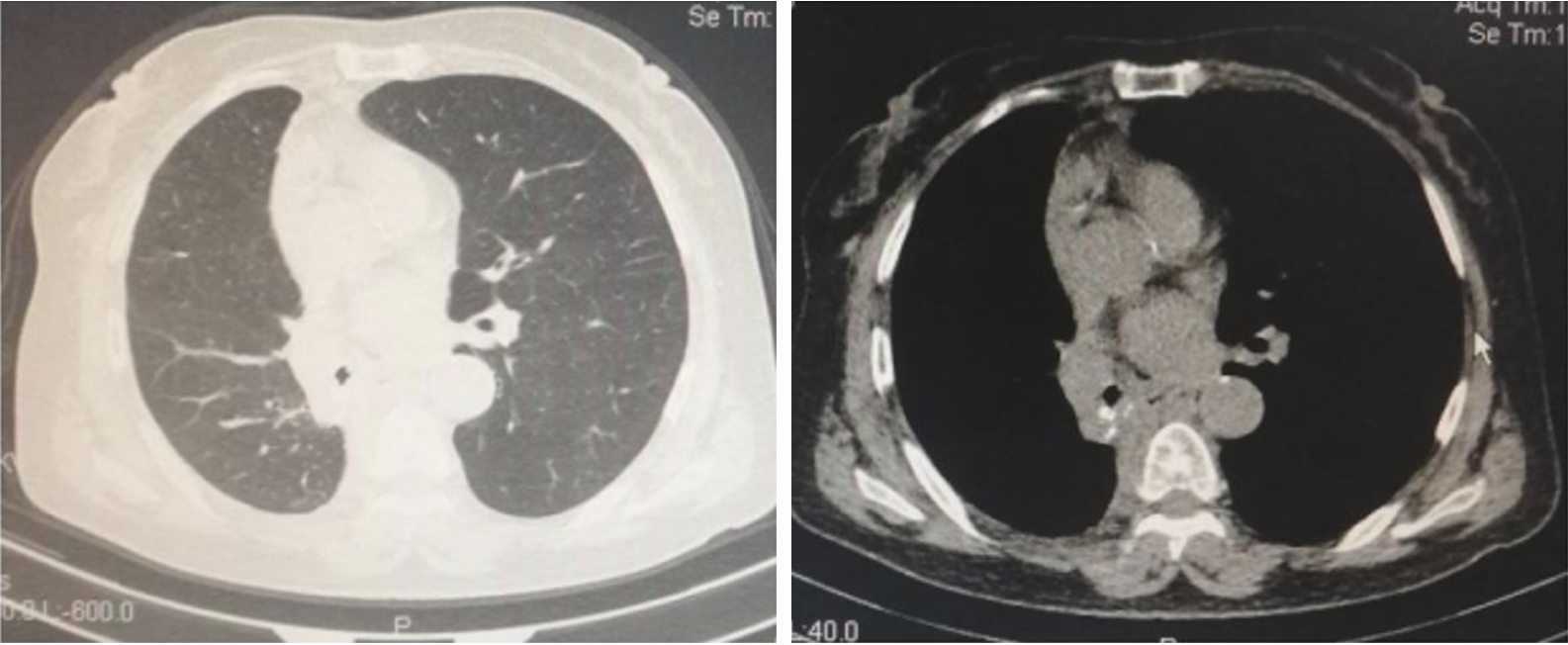
One month later, the chest CT showed good lung expansion with no cavities or effusions, suggesting that the bronchial stump surrounding area had adhered and stabilized (Figure 3), and the chest tube was removed. Subsequently, the patient underwent adjuvant therapy with epidermal growth factor receptor tyrosine kinase inhibitor treatment plus chemotherapy postoperatively. The patient’s condition has remained clinically stable; unfortunately, she was lost to follow-up in the 5th year after the operation.
There have been reports of Hem-o-lock clip displacement to the biliary, urinary, and intestinal tracts after laparoscopic surgery, although the incidence is relatively low[7-11]. In the application of thoracic surgery, there has been a report of a tracheoesophageal fistula occurring 12 days after using the Hem-o-lock clip to handle the azygos vein in esophageal cancer surgery[12]. There is also a report of a Hem-o-lok clip displacement to the bronchus 7 years after a thoracoscopic right lower lobectomy, but the specific site of use was not detailed; the considered mechanisms are: (1) Respiratory cycle movement and friction with adjacent anatomical locations cause gradual erosion and penetration of the bronchial wall into the bronchial cavity; (2) Postoperative rejection response; and (3) Rough surgical manipulation leads to bronchial wall compression, corrosion, and necrosis[13].
BPF refers to the communication fistula between bronchi or alveoli and the pleural cavity, one of the serious complications after lung resection. In recent years, with the development of surgical techniques, improvement of surgical instruments, and deepening of understanding of the perioperative pathophysiological process of the disease, its incidence has decreased significantly. The incidence rate is 1.5% to 4.5% after pneumonectomy, and 0.5% to 1% after lobectomy and sublobar resection[14], but the mortality rate is as high as 40%[15]. It has been reported that BPF usually occurs between 7 days and 10 days postoperatively, and there are also a few late BPFs occurring more than 1 month postoperatively. Most surgeons believe that the main risk factors for BPF are chemotherapy and radiotherapy, tumor residue, chronic obstructive pulmonary disease, diabetes, and malnutrition[16-20]. The clinical manifestations can be sudden dyspnea, chest pain, hemodynamic instability, and tension pneumothorax after lung resection, or symptoms such as fever, malaise, and sputum expectoration due to empyema. Regarding the treatment of BPF, the efficacy of early chest closed drainage is universally recognized; it is currently widely believed that BPF usually does not close spontaneously and almost always requires bronchoscopy (occlusion, sclerotherapy, etc.) or surgical treatment; however, there is still controversy regarding the timing of reoperation.
In this patient, the bronchial stump corner had poor staple effect, and a Hem-o-lock clip was applied after a 3-0 Mersilk suture and water testing without leakage. The patient coughed out the complete Hem-o-lock clip and knot. Considering that the local tissue of the bronchial stump at the clip closure was ischemic, and due to coughing movements, it eventually fell off; since the pleural cavity was in a postoperative changed state and had adhered, there was no severe pneumothorax, the local space was small, and the visit was timely, the drainage tube was unobstructed, so no special treatment was performed for the bronchial fistula. One month later, the chest CT imaging revealed good lung expansion without evidence of cavity or effusion, suggesting stabilization of the bronchial stump.
Although the patient’s postoperative recovery was largely successful with effective management of the complication, this case underscores the importance of careful consideration when using the Hem-o-lock clip for non-vascular tissues in thoracic surgery.
| 1. | Ying RC, Jin HC, Zhang J, Zhang XP, Feng GH. [Laparoscopic cholecystectomy using the Hem-o-Lok clip]. Zhongguo Weichuang Waike Zazhi. 2005;5:284-285. [DOI] [Full Text] |
| 2. | Al-Temimi MH, Berglin MA, Kim EG, Tessier DJ, Johna SD. Endostapler versus Hem-O-Lok clip to secure the appendiceal stump and mesoappendix during laparoscopic appendectomy. Am J Surg. 2017;214:1143-1148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Delibegović S, Mehmedovic Z. The influence of the different forms of appendix base closure on patient outcome in laparoscopic appendectomy: a randomized trial. Surg Endosc. 2018;32:2295-2299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Delibegović S. The use of a single Hem-o-lok clip in securing the base of the appendix during laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2012;22:85-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Porpiglia F, Renard J, Billia M, Cossu M, Morra I, Terrone C, Scarpa RM. Fast and safe closing of urethra during laparoscopic radical cystectomy. J Endourol. 2006;20:651-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Izaki H, Fukumori T, Takahashi M, Nakatsuji H, Oka N, Taue R, Nishitani MA, Kanayama HO. Clinical research of renal vein control using Hem-o-lok clips in laparoscopic nephrectomy. Int J Urol. 2006;13:1147-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Ji B, Wang GY, Liu YH, Liu K, Lü GY, Zhang W. [Report of 6 cases of Hem-o-lok clips migrating into the biliary tract after laparoscopic cholecystectomy]. Fuqiangjing Waike Zazhi. 2011;16:46, 52. [DOI] [Full Text] |
| 8. | Tang XD, Liu SH, Chen S. [Two cases of Hem-o-lok clips wandering in the common bile duct after laparoscopic cholecystectomy and biliary exploration for stone removal]. Zhonghua Xiaohua Neijing Zazhi. 2015;32:565-566. [DOI] [Full Text] |
| 9. | Gonzalgo ML, Pavlovich CP, Trock BJ, Link RE, Sullivan W, Su LM. Classification and trends of perioperative morbidities following laparoscopic radical prostatectomy. J Urol. 2005;174:135-139; discussion 139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Li LJ, Song W, Wang MW, Zhao Y. [A Case Report of Complication Occurring with Hem-O-Lok Clips in Urinary Conduit After Radical Prostatectomy and Review of the Literature]. Miniao Kaike Zazhi. 2014;45, 46, 51. [DOI] [Full Text] |
| 11. | Hao XW, Li P, Zhang ST, Ji M. A Case of Hem-o-lok Ligation Clip Detachment into the Duodenum after Laparoscopic Cholecystectomy. Zhonghua Xiaohua Neijing Zazhi. 2011;28:592-593. [DOI] [Full Text] |
| 12. | Han Y, Yang S, Huang W, Wang Z, Li H. A Hem-o-Lok-Induced Tracheoesophageal Fistula Cured by Temporary Airway Stenting Modified With Three-Dimensional Printing. Ann Thorac Surg. 2018;106:e219-e221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Shi YX, Wang C. [A rare case report of Hem-o-lok clip displacement into the bronchus]. Linchuang Feike Zazhi. 2018;23:1162-1163. [DOI] [Full Text] |
| 14. | Alpert JB, Godoy MC, Degroot PM, Truong MT, Ko JP. Imaging the post-thoracotomy patient: anatomic changes and postoperative complications. Radiol Clin North Am. 2014;52:85-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Asamura H, Naruke T, Tsuchiya R, Goya T, Kondo H, Suemasu K. Bronchopleural fistulas associated with lung cancer operations. Univariate and multivariate analysis of risk factors, management, and outcome. J Thorac Cardiovasc Surg. 1992;104:1456-1464. [PubMed] |
| 16. | Wright CD, Wain JC, Mathisen DJ, Grillo HC. Postpneumonectomy bronchopleural fistula after sutured bronchial closure: incidence, risk factors, and management. J Thorac Cardiovasc Surg. 1996;112:1367-1371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 124] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Farkas EA, Detterbeck FC. Airway complications after pulmonary resection. Thorac Surg Clin. 2006;16:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Li SJ, Zhou XD, Huang J, Liu J, Tian L, Che GW. A systematic review and meta-analysis-does chronic obstructive pulmonary disease predispose to bronchopleural fistula formation in patients undergoing lung cancer surgery? J Thorac Dis. 2016;8:1625-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Okuda M, Go T, Yokomise H. Risk factor of bronchopleural fistula after general thoracic surgery: review article. Gen Thorac Cardiovasc Surg. 2017;65:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 20. | Toufektzian L, Patris V, Sepsas E, Konstantinou M. Does postoperative mechanical ventilation predispose to bronchopleural fistula formation in patients undergoing pneumonectomy? Interact Cardiovasc Thorac Surg. 2015;21:379-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/