Published online Apr 26, 2025. doi: 10.12998/wjcc.v13.i12.100045
Revised: October 25, 2024
Accepted: December 16, 2024
Published online: April 26, 2025
Processing time: 154 Days and 5.5 Hours
Lung cancer is the most prevalent malignant tumor in human body, and is characterized by a high level of malignancy. The most common metastatic sites include the liver, bone, brain, and adrenal gland, while lung cancer resulting in gas
A 74-years-old man with lung cancer was hospitalized owing to blood in the stool, The cause was identified as metastasis to the small intestine, and the patient subsequently underwent radical resection of the small intestine tumor. Currently, the overall condition of the patient is good, and undergoing combined chemo
Early intervention in patients with metastatic tumors can significantly improve prognosis.
Core Tip: This article introduces a case of lung cancer with small bowel metastasis and gastrointestinal bleeding, which is relatively rare compared with other sites, and the patient underwent laparoscopic radical resection of small bowel cancer, and the long-term prognosis still needs to be observed and followed. We look forward to providing a helpful clinical experience based on this case, and there is an urgent need to record more cases to support more advanced research efforts aimed at improving the detection rate of these patients and ultimately improving the quality of life and survival of patients.
- Citation: Yuan TY, Chen YX, Zhao YG, Wang B, Wang SX. Gastrointestinal bleeding due to small bowel metastasis from lung adenocarcinoma: A case report. World J Clin Cases 2025; 13(12): 100045
- URL: https://www.wjgnet.com/2307-8960/full/v13/i12/100045.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i12.100045
Lung cancer is the most prevalent malignant tumor in the human body, characterized by a high degree of malignancy. The most common sites of metastasis are including the liver, bone, brain, and adrenal glands. In contrast, metastasis of lung cancer resulting in the digestive tract is relatively uncommon, and limited research is found on this topic. Therefore, this study aims to investigate a case of small bowel metastasis from lung cancer that caused gastrointestinal bleeding, offering a potential diagnostic and therapeutic approach for managing with gastrointestinal bleeding as the primary symptom.
This patient was admitted to the hospital with black stools for 5 hours.
The patient (a 74-year-old elderly man) was first visited our hospital in 2019 after a ground-glass nodule was discovered in the upper lobe of the right lung. On July 18, 2019, he underwent thoracoscopic wedge resection of the right upper and lower lung nodule under general anesthesia, following the ruling out of any contraindications to surgery. Postoperative pathology revealed invasive adenocarcinoma (nodule in the upper lobe of the right lung), with two masses that did not invade the lung membranes, and no cancerous involvement of the anastomotic margins. The (nodule in the lower lobe of the right lung) showed microinvasive adenocarcinoma without invasion of the lung membranes, and no cancer involvement at the anastomotic end margins. The patients underwent regular follow-up chest computed tomography (CT). On July 25, 2023, the patient was hospitalized with a history of “4 years after surgery for right lung cancer, and the right lung nodule was found to have increased in size over the past 3 days compared with the previous one”. Upon admission, the patient underwent a complete examination of blood, which revealed no significant abnormalities. After discussing with the family, the patient chose to undergo CT-guided percutaneous lung nodule aspiration biopsy and thermal ablation under local anesthesia on July 28, 2023 and August 8, 2023, respectively, following these procedures, the patient underwent regular follow-up chest CT scans of the upper and middle lobe lesions in the right lung, alongside thermal ablation treatment to reduce the lesions compared to those of the previous scan.
On January 9, 2024, the patient was admitted to the emergency department of our hospital 5 hours ago for acute upper gastrointestinal hemorrhage after having 3 black stools, large in total amount, without vomiting blood, accompanied by obvious panic and weakness, without fainting, and without abdominal pain and distension.
Thirty years history of hypertension, systolic blood pressure up to 200 mmHg, taking 2 tablets of compound reserpine 1 day, 1 tablet of nifedipine extended-release tablets 1 day, 2 tablets of captopril 1 day, systolic blood pressure under control at 150 mmHg. Seven years history of carotid stenosis on the left side and cerebral stenosis. Four years after surgery for right lung cancer. Right lung cancer 4 years after surgery. Five months after thermal ablation of right lung tumor. No history of coronary heart disease or diabetes mellitus; no history of hepatitis, tuberculosis or other infectious diseases or close contact with them; no history of blood transfusion; allergic to penicillin and streptomycin, no history of food or other drug allergies; history of vaccinations unknown.
No obvious abnormalities were found.
On January 9, 2024, the patient presented with black stool and was urgently tested, revealing a hemoglobin level of 58
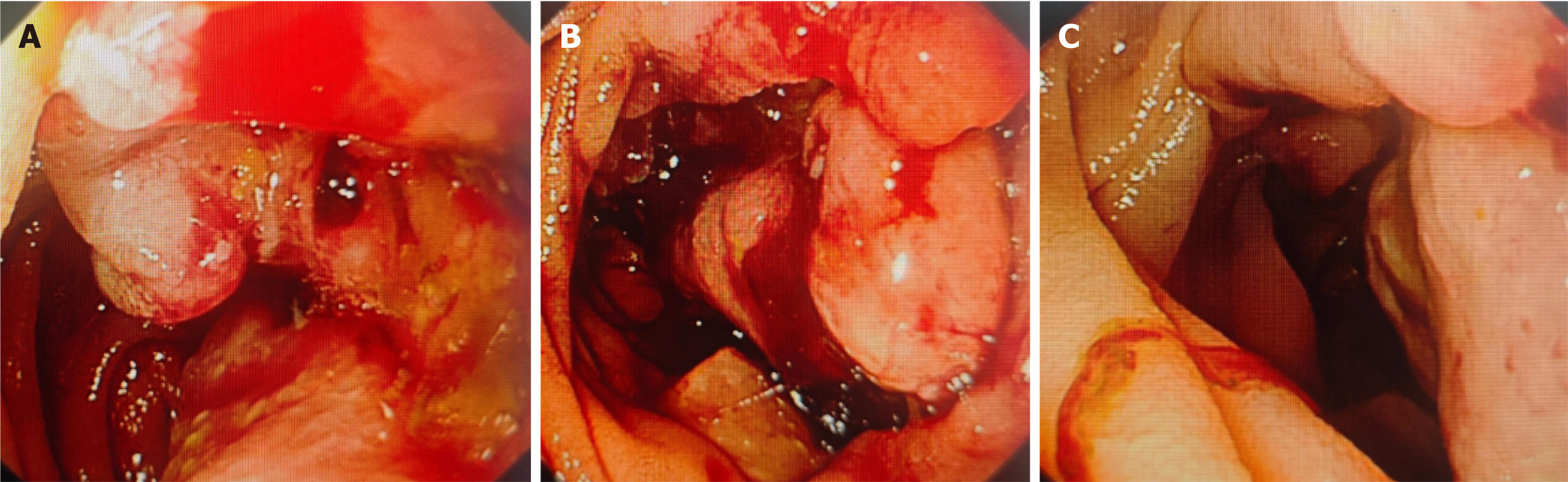
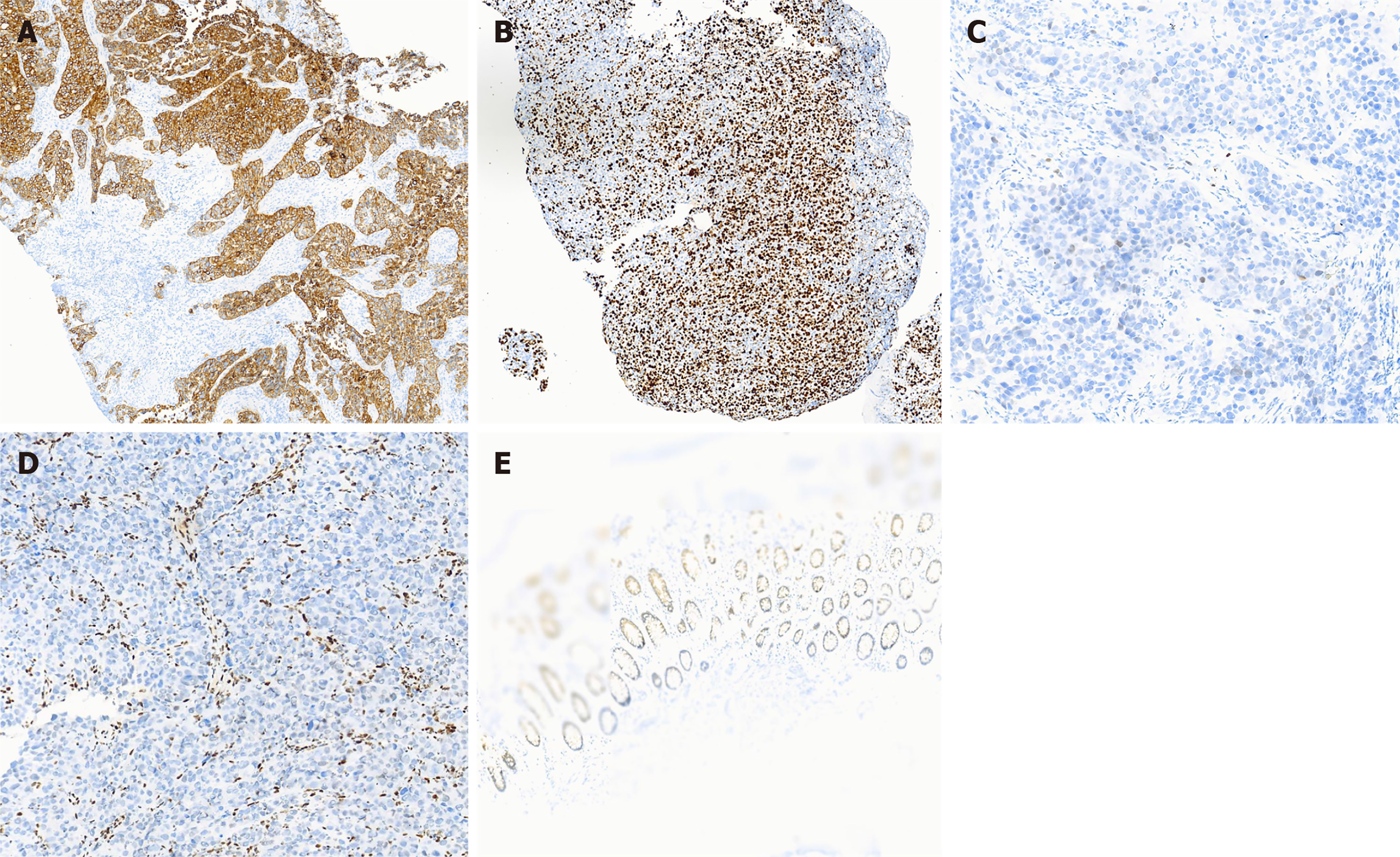
The patient underwent a CT examination of the chest and abdomen, which revealed localized thickening of the small bowel wall in the left lower abdomen with multiple surrounding lymph nodes, suggesting small bowel occupancy with peripheral lymph node metastasis. Oral small bowel imaging showed gastritis, while no significant abnormalities were found in the jejunum ileum and ileocecum region. Additionally, double-balloon enteroscopy revealed small bowel occupation and bleeding; along with submucosal elevation, that may represent lipoma. The nature of esophageal lesions; non-atrophic gastritis (Figure 1). Immunohistochemistry results showed the following: P53 (wild type expression), Ki67 (basal high expression), and jejunum checked for carcinoma, the findings included: SMARCA4 (deletion), CK7 (+), TTF-1 (-), Napsin A (-), SPA (-), SP-B (-), CK20 (-), Villin (focal +), CDX-2 (-), SATB2 (individually weakly plus), CK5/6 (-), P40
Following the surgical intervention, the patient no longer experienced black stool, and the postoperative diagnosis included: (1) Postoperative lung cancer with small intestinal tumor metastasis; (2) Acute upper gastrointestinal hemorrhage; (3) Postoperative right lung cancer; and (4) Post thermal ablation of the right lung tumor.
The patient underwent laparoscopic radical resection for small bowel cancer on January 20, 2024.
A literature review revealed that > 50% of patients with small intestinal metastases from lung cancer died within 3 months, while < 10% survived beyond 1 year[1]. Tracking and follow-up revealed that the patient discontinued docetaxel/carboplatin and tirilizumab combination chemotherapy after surgery, during which no adverse reactions, such as small intestinal hemorrhage, perforation, or obstruction, were observed. As a non-traditional PD-1 inhibitor, tirilizumab avoids T-cell reduction while maintaining anti-tumor efficacy. The current general condition of the patient is good, further demonstrating that early detection and therapeutic intervention can improve the survival rate of such cases.
(1) Digestive tract metastasis caused by lung cancer is primarily categorized into symptomatic and asymptomatic digestive tract metastasis. Symptomatic digestive tract metastasis can be detected clinically. In contrast, asymptomatic digestive tract metastasis, is usually identified more frequently during autopsy than that observed in the clinically, making it challenging to detect and diagnose; (2) Since many gastrointestinal symptoms in patients, such as nausea, vomiting, and abdominal distension, are non-specific and may be mistaken for normal gastrointestinal reactions during lung cancer treatment, this makes diagnosis challenging owing to the atypical symptoms; and (3) Owing to the lack of specific tests for digestive tract metastasis caused by lung cancer, it can be more difficult to detect small bowel tumors using standard abdominal CT scans. Some studies have revealed that new technologies, such as positron emission tomography-CT, capsule endoscopy, and double-balloon enteroscopy, show good prospects for detecting small bowel lesions. However, it remains challenging to diagnose without specificity in ancillary tests.
The patient initially underwent abdominal CT scanning, which revealed localized thickening of the small intestine wall. While these findings could be considered as a placeholder, they did not clarify the nature of the lesion of the patient. Additionally, the small bowel imaging method provides limited results and fails to identify the cause of the gas
Studies have shown that patients with gastrointestinal metastases usually indicate advanced stages of the tumor. Surgical intervention is typically required for complications such as gastrointestinal perforation and gastrointestinal hemorrhage. However, early detection of gastrointestinal metastases in patients with lung cancer, along with timely surgery, can help alleviate the life-threatening symptoms and improve long-term survival in patients with only isolated gastrointestinal metastases. This patient has undergone radical resection of small bowel cancer and currently exhibits no further black stools. However, the long-term prognosis requires continued observation and follow-up. Additionally, the optimal timing and treatment strategies for surgical treatment of lung cancer metastases in the small bowel require further clinical research.
This case provides several insights: (1) For patients with lung cancer, small intestinal metastasis is rare; however, with advancements in diagnostic and treatment technologies, reports of such cases are gradually increasing. When gas
| 1. | Liu T, Geng Y, Wang Z, Peng X, Liu J, Huang Y. Lung carcinoma with small intestinal metastases and gastrointestinal bleeding: A rare case report. Oncol Lett. 2023;25:241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Lee PC, Lo C, Lin MT, Liang JT, Lin BR. Role of surgical intervention in managing gastrointestinal metastases from lung cancer. World J Gastroenterol. 2011;17:4314-4320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 52] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/