INTRODUCTION
A clavicle fracture stands out as one of the most frequently occurring fractures, with an overall incidence rate of 64 cases per 100000 individuals each year[1,2]. Over time, a multitude of treatment approaches have been developed to address this issue. Extensive investigation into the therapeutic techniques for clavicle fractures has been conducted, comparing a range of treatment options from conservative to surgical management in numerous studies[3-5]. Furthermore, a mounting body of high-quality evidence from randomized controlled trials has suggested that non-surgical methods may lead to increased initial fracture displacement, higher non-union rates, and longer recovery times, fostering a growing consensus that surgical treatment may be more beneficial for individuals with clavicle fractures especially when it occurs in the lateral one-third[6-8].
Several surgical methods are available for lateral-third clavicle fracture management, with plate and screw constructs representing one of the most employed options[4]. There are a multitude of choices to fix the fracture using this construct. This editorial outlined the key plating choices employed in the management of distal third clavicle fractures and the fixation methods involved in them.
ANATOMICAL PRECONTOURED LOCKING PLATES
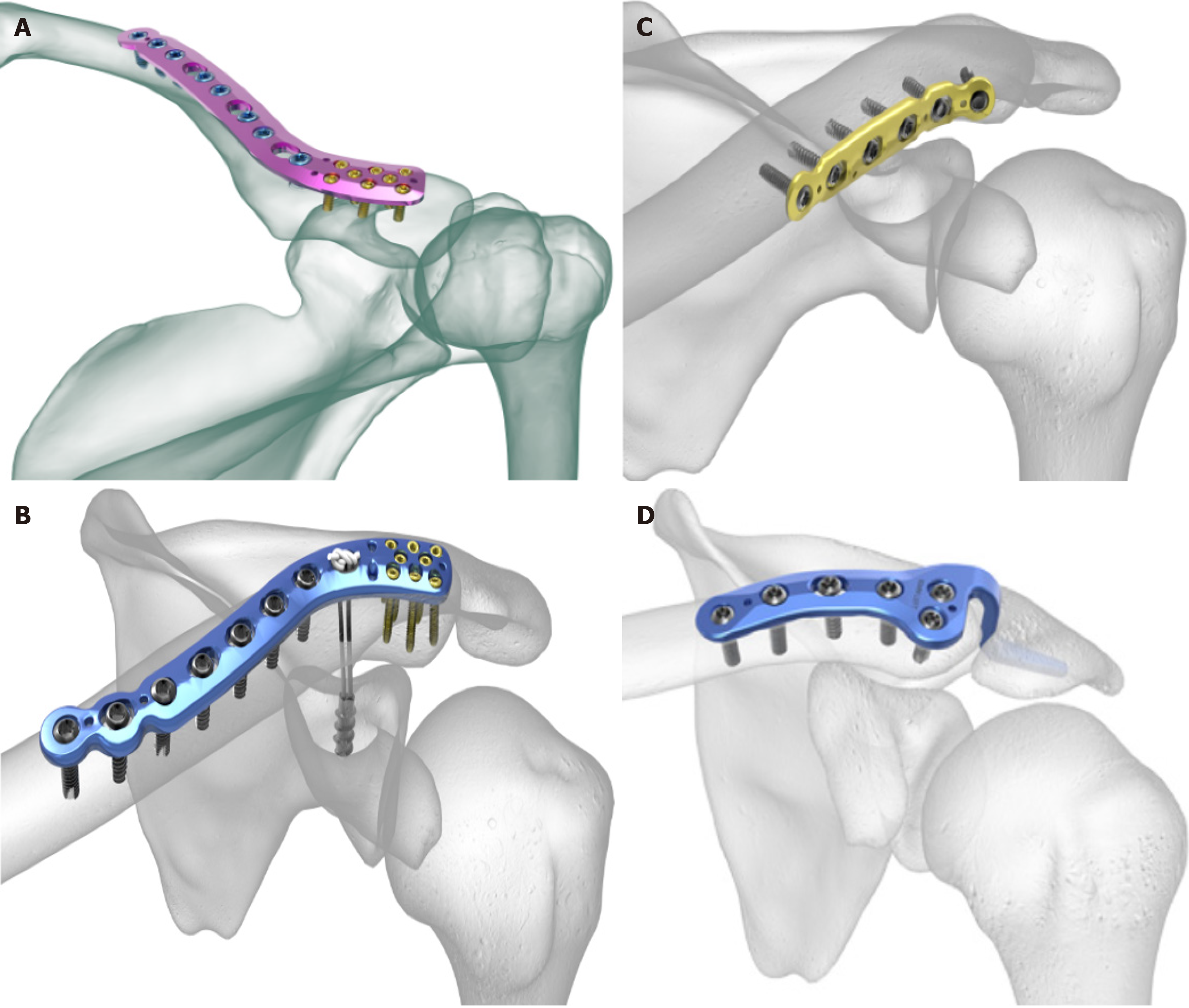
Locking plates remain one of the most utilized in the management of fractures due to their advantages, such as strong fixation resulting from the screw-plate locking mechanism and minimal contact with cortical bone, which preserves blood supply[9,10]. The current implementation of the minimally invasive technology that allows plating by percutaneous methods combined with locking plates is considered ideal for bone fixation as it minimizes periosteal stripping and promotes rapid healing[10]. The recent array of region-specific tailor-made locking plates is considered less conspicuous even after the bone union, and its implant removal rates are lower compared to the traditional plates[11]. Numerous anatomically contoured plates available in the market are equipped with lateral screw clusters, designed to secure even small lateral fragments effectively as shown in Figure 1A. In most of these cluster designs, the lateral fragment needs to be around 10 mm to 15 mm in size to accommodate three screws. Some plates come with features such as suture holes or provisions for snugly incorporating a suture button considering the additional option to add a coracoclavicular (CC) suspensory fixation as shown in Figure 1B.
Figure 1 Common plating options in the management of distal end of clavicle fracture.
A: Anatomical precontoured locking plate in superior positioning; B: Anatomical precontoured locking plate with coracoclavicular suture construct; C: Anteroinferior positioning of dynamic compression plates; D: Hook plate.
The consideration to incorporate CC fixation along with the plated constructs is decided based on their efficacy demonstrated in various studies. For instance, in a study conducted by Furuhata et al[12], it was observed that using a locking plate as the sole treatment for injuries involving ligamentous injury demonstrated an increase in the CC distance, while those without the CC ligament injury did not show this pattern. This finding implied that locking plates on their own may not provide adequate vertical stability when CC ligaments are compromised. From this finding, one might conclude that CC fixation could be bundled with the traditional locking plates in cases with CC ligament injury. However, it is worth noting that no disparities in function scores, union rates, or complications were noted between the two groups. We also have studies reporting comparable results using either of the techniques for injuries with CC ligament injury[13]. In summary, we understand that incorporation of the CC fixation augments the biomechanics of the repair construct in distal clavicular fractures. It is indicated in cases with partial or complete CC ligament injury (Neer 2B and 5), whereas it might not be indicated in cases with intact ligaments (Neer 2A).
Celestre et al[14] conducted a study to understand the effect of localization of the plate in the management of midshaft clavicular fractures. They compared anterior vs superior locking plates and standard vs locking plates. Their findings indicated that resistance to failure due to bending along with axial compression/torsion stiffness was found at its best in the superior location of the locking plate. Hence, a similar positioning and plating option is commonly used for lateral end clavicle fractures. Locked plating has certain limitations, including the potential challenge of achieving sufficient grip when there is lateral comminution and the possibility of implant prominence. In a retrospective analysis encompassing 16 cases of distal clavicle fractures treated with plates and screws, 50% of cases required hardware removal[15]. However, there are also other studies with lower hardware removal rates[16-18]. Hence, caution should be exercised in the selection of these high-profile plates that might necessitate future surgery for implant removal.
NON-LOCKING PLATES
Apart from the precontoured anatomical locking plates for lateral end clavicle fractures, several other plate types used in surgical management include reconstruction plates, limited-contact dynamic compression plates, and T-plates with comparable clinical results[19-21]. However, clinical results comparing them with the locking plates in the fixation of the lateral end of the clavicle are limited. To enhance the rate and quality of bone union, several factors need to be considered when selecting an implant, including the location of the fracture, level of comminution, quality of the bone, demand, and compliance of the patient. Clavicle bridging plating in osteoporotic bone, while achieving stable fixation, may not provide the same level of rigidity. It is noted that in elderly patients more complications are noted in plated constructs compared to intramedullary pin fixation (Knowles pinning)[22]. Plate loosening is the drawback of dynamic compression plate fixation, especially in patients with poor bone quality. The locking plate technology mitigates this complication of the plate and screws loosening with a robust fixation construct even in osteopenic bone[22].
HOOK PLATES
Hook plates are a construct with a hook placed in the lateral aspect beneath the acromion process anchored to the medial clavicle fragment with cortical screws as shown in Figure 1C. This approach offers a means of stabilizing fracture of the distal end of the clavicle with small lateral fragments which is not sufficient for locking compression plates to act upon. In addition to the horizontal stability, the hook plates ensure vertical stability so that they can be used in fractures with CC ligament injury with coracoid fractures where CC fixation is impractical. Another additional advantage is noted in cases of sustaining type 2B fractures where there is no need for extensive dissection around the trapezoid ligament. A 98% fusion rate and comparable functional outcomes were noted in patients using hook plates and other fixation methods based on a recent meta-analysis[23].
However, there are concerns related to the use of hook plates. The hook can potentially cause erosion in the inferior aspect of the acromion, which was noted in 27% of cases[23]. There are some reported cases of acromial fractures[24,25]. As a result, it is generally recommended to remove the implant after the fracture has fully healed, adding to the overall treatment burden. Factors that increase the risk of acromion osteolysis include the placement of the hook in a position that points anteriorly by remaining posterior to the acromioclavicular joint[26], hook misalignment where it does not match with the slope of the acromion that results in point loading instead of even distribution of the load across the entire hook[27], and allowing shoulder abduction and flexion of more than 90 degrees before plate removal. Further, delayed removal of the implant after the fracture has fully healed (e.g., due to noncompliance or loss to follow-up) is a consideration with hook plates. Furthermore, it is advisable to exercise caution when contemplating the use of hook plates in cases where preexisting acromial erosion is noted as seen in cuff tear arthropathy, weak bone due to osteoporosis, or the presence of an os acromiale[28].
The mismatch noted between the hook and the acromion slope can be mitigated by pliable plates that could be manually contoured or the utilization of recent plates with a 15-degree inferior angulation[29]. The posterior aspect of the acromioclavicular joint capsule can be used as a reference point during the surgical procedure to make sure that the hook is placed in the ideal anterior position. Other noted complications with this device include arthrosis of the acromioclavicular joint (22%), fractures of the clavicle just medial to the plate (22%), and shoulder stiffness or subacromial impingement (47%)[23]. We also noted reports of tears in the rotator cuff muscles in a magnetic resonance imaging study. However, they did not find any complete tears among the 39 cases investigated[30]. Finally, another study noted that 66% of demanding athletes did not return to sports with the utilization of the hook plates[31]. Although this inference is from a single study, one could reserve the utilization of the hook plates in select cases of elite athletes rather than for everyone.
PLATE POSITIONING
One key component in the utilization of the plating for the lateral end of the clavicle is the choice of plate position. The two commonly involved plate positioning methods include anterior inferior plating and superior plating as shown in Figure 1A and D, respectively. Multiple studies have sought to compare the merits of these two approaches for clavicle fractures. However, the optimal positioning of the plate and choice of the plate type remains a subject of debate. Zlowodzki et al[3] reported an association between superior plating and increased postoperative symptoms. In contrast, Robertson et al[8] argued in favor of superior plating over anterior inferior plating, citing advantages in fracture fixation for routine activities[32]. Furthermore, previous research has highlighted the superior biomechanical stability of superior plating[14]. Conversely, evidence has suggested a reduced risk of implant prominence and injury to the neurovascular bundle with anterior inferior plating[33-35].
COMPARATIVE STUDIES
In general, comparable results were noted in studies comparing the locked plating or CC fixation or hook plates in the management of lateral clavicular fractures with respect to the bone union and final functional outcomes. Despite removing the events of hardware removal, hook plates did not perform well in early functional outcomes and complications compared to the other two[23]. When coming to the locking plates with and without the addition of the CC constructs, either comparable results or results favoring additional CC fixation were noted[16,36].
Upon analyzing 59 studies with 2284 patients in a meta-analysis comparing different distal clavicle fixation techniques, hook plates did not perform well in Constant scores compared to CC fixation. However, in comparison to locking plates and K-wire constructs no difference was noted. All the included constructs gave comparable union rates[13]. Maximum complications including hardware failure, infection, and wound complications were noted in the K-wire constructs in the form of tension banding followed by hook plates with the second-highest rate of complications. Similar results were noted in another systematic review comparing the complications with hook plates compared to locked plating and CC fixation[23]. Their recommendation was to make a surgical fixation using CC fixation alone, followed closely by a locking plate with CC fixation.
Recent case reports on using reconstruction plates in the anteroinferior position for lateral end clavicle fracture without comminution with a single screw in the lateral fragment added to the interest[37]. Recently published biomechanical studies showcased the superiority of lateral locking plates with orthogonal anteroposterior locking screw placement in the lateral fragment to negate the need for CC stabilization[38]. Further, clinical trial results demonstrated comparable clinical outcomes at 1 year in hook plate and locking plate constructs[17]. However, quicker recovery was noted in the locking plate fixation[39]. Similar results were noted between the locking and non-locking plate constructs[40].
CONCLUSION
This literature review provided recommendations on implant selection in the management of lateral end clavicle fractures. Wherever possible, utilization of fixation techniques such as CC fixation and trans-osseous suturing should be instigated to avoid complications due to hardware prominence since similar union rates were recorded compared to other plating techniques. We did not note sufficient evidence to recommend arthroscopic-assisted CC fixation or adding CC fixation to the traditional locking plates over the commonly performed open fixation techniques. However, considering the evidence from the biomechanical studies, addition of CC fixation could be considered in high-demand athletes. On the other hand, one should not consider K-wires and tension bands as their first choice due to the inferior results compared to other techniques. In fracture patterns with small lateral fragments that could not be stabilized by other means, hook plates remain an ideal candidate. However, due to the higher complication rate compared to other techniques hook plates are less suitable for routine use. Hence, the selection of the ideal fixation construct is determined by the size of the lateral fragment and the status of CC ligaments.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jiang N, China S-Editor: Chen YL L-Editor: Filipodia P-Editor: Xu ZH