Published online Feb 16, 2024. doi: 10.12998/wjcc.v12.i5.988
Peer-review started: September 22, 2023
First decision: November 13, 2023
Revised: December 11, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 16, 2024
Processing time: 130 Days and 18 Hours
The most common causes of scrotal enlargement in patients include primary tumor of the scrotum, inflammation, hydrocele of the tunica vaginalis, and indirect inguinal hernia; scrotal enlargement caused by external tumors of the scrotum is rare. The patient had both a greater omentum tumor and an inguinal hernia, and the tumor protruded into the scrotum through the hernia sac, which is even rarer. Moreover, omental tumors are mostly metastatic, and primary omental fibroma is rare.
Here, we report a rare case of a 25-year-old young man with scrotal enlargement and pain for 3 months. Preoperative examination and multidisciplinary discu
This unusual presentation of a common inguinal hernia disease illustrates the necessity of performing detailed history taking, physical examination, and imaging before surgery.
Core Tip: Intrascrotal tumors are common male reproductive system-related tumors and are mostly primary tumors. In this case, the tumor in the scrotum of the patient was not a primary tumor of the scrotum or a metastatic lesion of other tumors. Instead, a primary lesion of the greater omentum fibroma in the abdominal cavity was completely displaced to the scrotum, which is a rare occurrence. We searched the studies included in PubMed since 2011 and found four similar reports of fibromas herniating into the scrotum, originating from the greater omentum, mesentery, and appendix. Analysis showed that the patients’ tumor activity was high, and all patients also had an inguinal hernia, which was the basis of the disease. This case reminds us that even the most common diseases may have various unexpected situations, and it is necessary to conduct detailed inquiries and physical examinations on the patient and complete relevant preoperative examinations and tests to avoid misdiagnosis. When the patient's condition is complex, multidisciplinary joint diagnosis and treatment are needed to choose the most suitable treatment method.
- Citation: Zhou P, Jin CH, Shi Y, Ma GQ, Wu WH, Wang Y, Cai K, Fan WF, Wang TB. Omental fibroma combined with right indirect inguinal hernia masquerades as a scrotal tumor: A case report. World J Clin Cases 2024; 12(5): 988-994
- URL: https://www.wjgnet.com/2307-8960/full/v12/i5/988.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i5.988
Intrascrotal tumors are common male reproductive system-related tumors and are mostly primary tumors. In this case, the tumor in the scrotum of the patient was not a primary tumor of the scrotum or a metastatic lesion of other tumors. Instead, a primary lesion of the greater omentum fibroma in the abdominal cavity was completely displaced to the scrotum, which is a rare occurrence. We searched the studies included in PubMed since 2011 and found four similar reports of fibromas herniating into the scrotum, originating from the greater omentum, mesentery, and appendix. Analysis showed that the patients’ tumor activity was high, and all patients also had an inguinal hernia, which was the basis of the disease. This case reminds us that even the most common diseases may have various unexpected situations, and it is necessary to conduct detailed inquiries and physical examinations on the patient and complete relevant preoperative examinations and tests to avoid misdiagnosis. When the patient's condition is complex, multidisciplinary joint diagnosis and treatment are needed to choose the most suitable treatment method.
A 25-year-old male patient presented to the Department of Urology, South China Hospital of Shenzhen University, because of "right testicular pain for 3 months, aggravated for 1 wk".
The patient developed right testicular pain without obvious cause 3 months prior with intermittent attacks accompanied by gradual enlargement of the scrotum and lower abdominal pain 1 wk prior.
Previously healthy and without any other illnesses.
No special.
Physical examination revealed that the patient had a mass in the right groin area varying in size with the position of the body, which could be partially returned, and there was a sense of impact in the inner ring opening when coughing. The patient had significant scrotal swelling, and approximately 5 cm of mass could be felt, accompanied by light tenderness.
Carcinoembryonic antigen (CEA) 1.49 ng/mL, alpha-fetoprotein (AFP) 2.90 ng/mL, β- human chorionic gonadotropin (HCG) 0.15 IU/L, lactate dehydrogenase (LDH) 148 u/L ↓.
B ultrasound: Right inguinal oblique hernia, hernia sac considered omentum, right scrotal solid mass.
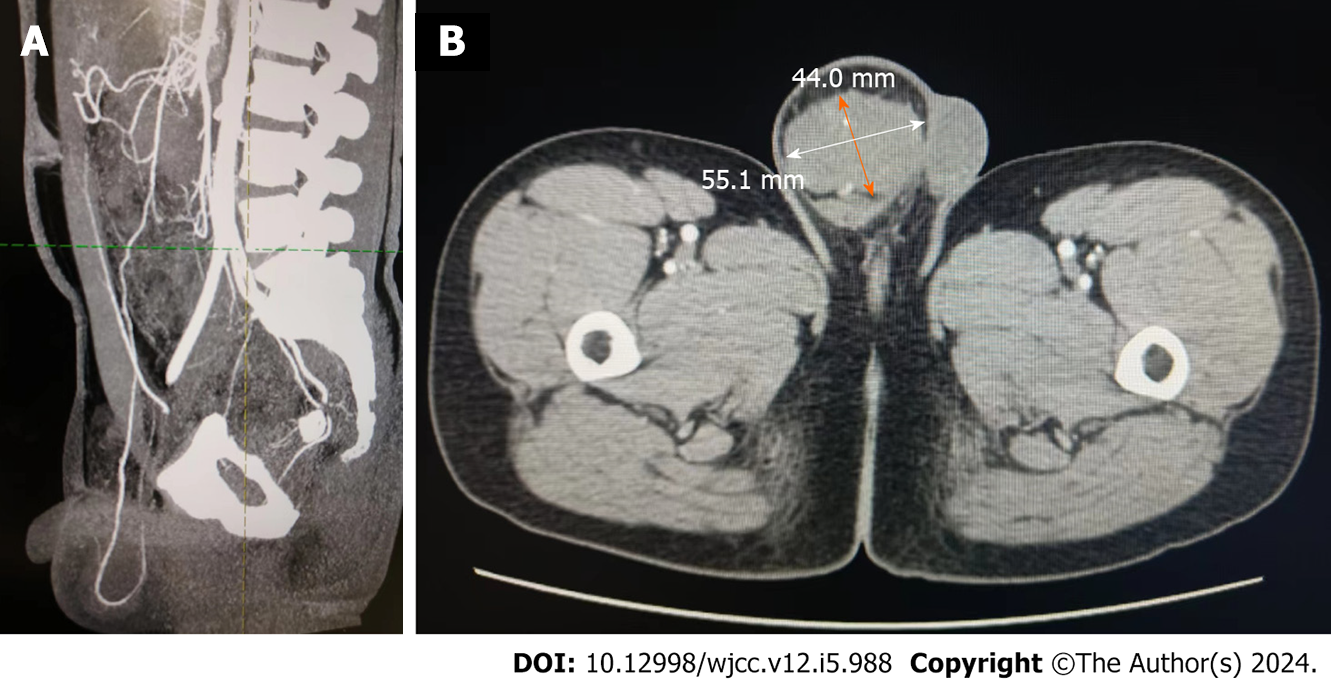
Total abdominal computed tomography (CT) enhancement: Right oblique inguinal hernia, hernia contents may be greater omentum. Right scrotal mass, no obvious enhancement, and superior mesenteric artery branch blood supply? The possibility of tumors of mesenteric origin was considered (Figure 1).
Pelvic magnetic resonance imaging (MRI) enhancement: Right scrotal mass with slightly short T1T2 signal, low signal in diffusion weighted imaging lesion, mixed apparent dispersion coefficient image with slightly low signal shadow, mild enhancement after enhancement, and clear boundary between the tumor and right testicle.
After completing the relevant examinations, after multidisciplinary discussions among doctors in urology, gastrointestinal surgery, and imaging, the patient was considered to have a right inguinal hernia and scrotal tumor before the surgery. Considering the degree of tumor activity and blood supply, the mass was most likely to be a greater omentum tumor, Mesenteric tumors and primary tumors in the scrotum are less likely. The nature of the tumor was unknown, and it was to be surgically removed directly. No preoperative puncture was performed to avoid the risk of tumor spread. We are considering adopting a surgical approach of groin exploration combined with laparoscopic exploration of the abdominal cavity for patients. After determining the source of the tumor, safely and completely remove the tumor.
If laparoscopic exploration considers metastatic cancer originating from within the abdominal cavity, further abdominal surgery may be required under laparoscopy (including resection or biopsy of intra-abdominal lesions, intestinal resection and anastomosis, combined organ resection, etc.).
Omental fibroma combined with right indirect inguinal hernia.
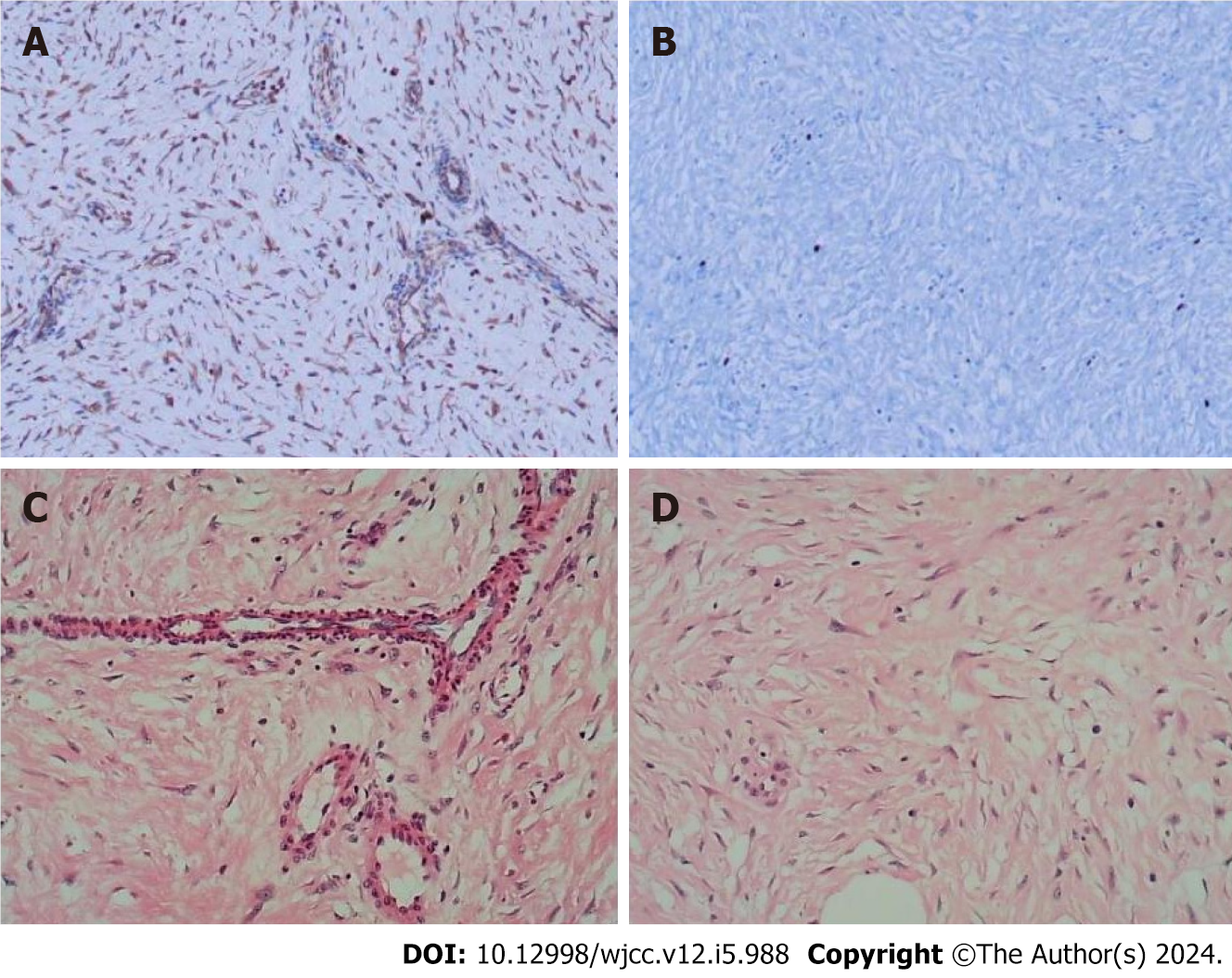
Postoperative pathological diagnosis: Right greater omentum mass, spindle cell proliferative lesion, considered benign or low-grade mesenchymal tumor, tended to be fibrous or fibroblastic in origin (Figure 2).
Immunohistochemistry: Vimentin +, Ki-67 < 1%. All others are negative: Alpha-smooth muscle actin, Desmin, CD34, s100 proteins (S100), signal transducer and activator of transcription 6, anaplastic lymphoma kinase, mucin 4, epithelial membrane antigen, CD117, discovered on GIST-1, and β-catenin (Guangzhou Kingmed Center for Clinical Laboratory).
A CTNNB1 gene mutation was detected (Ruijin Hospital, Shanghai Jiao Tong University School of Medicine).
Combined with the results of the original unit's immunohistochemistry and our unit's genetic test, it was judged to be consistent with fibromatosis (Ruijin Hospital, Shanghai Jiao Tong University School of Medicine).
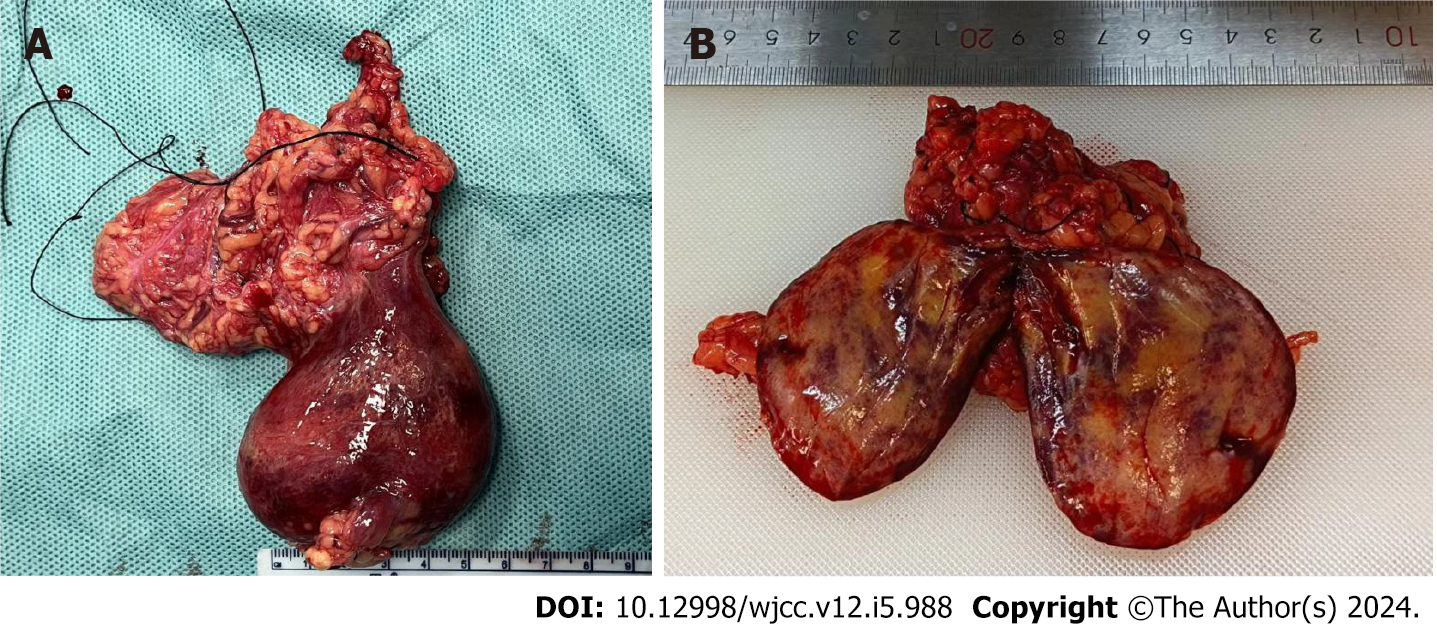
Intraoperative exploration: Through the right groin incision exploration, the tumor was confirmed to be of greater omentum origin, hard, completely enveloped, and approximately 6 cm × 5 cm in size. In addition, several nodules the size of rice grains were observed in the protruding omentum, and no abnormalities were observed in the right spermatic cord or testicular exploration. No obvious abnormality was found in any organ of the abdominal cavity by laparoscopy combined with exploration.
The greater omentum mass and part of the omentum nodule were resected and sent for rapid frozen section examination (Figure 3).
Intraoperative rapid frozen section examination revealed that the greater omentum mass was a benign spindle cell tumor, and the omentum nodule was considered a benign lesion.
Then, right inguinal oblique hernia tension-free repair was performed, and the operation was complete.
The patient was discharged the following afternoon.
The patient recovered well after the operation, and the stitches were removed in the outpatient department after discharge.
B ultrasound was reviewed 4 months after surgery, and total abdominal CT was reviewed 7 months after surgery. There was no recurrence of inguinal hernia, no recurrence of tumor, and no bad performance was found in the abdominal cavity, inguinal region or scrotum.
At a follow-up visit 7 months after the surgery, the patient felt fine, with no protrusion of the right inguinal hernia, no swelling of the scrotum, and no pain or discomfort.
We conducted a systematic search of the PubMed database with the following key words: Inguinal hernia, scrotum, and fibroma. A total of 4 cases of intraabdominal fibroma protruding into the scrotum, with inguinal hernia as the manifestation, have been reported since 2011 (Table 1).
| Ref. | Article | Left/right | Patient age (yr) | Diameter of tumor | Medical history | Tumor location |
| Alsaif[6], 2011 | Mesenteric fibromatosis presenting as an irreducible inguinal hernia | Left | 18 | 19 cm × 9 cm × 7 cm | 3 months | Omental fibroma |
| Khoo and Jacob[9], 2017 | An omental fibroma resembling a testicular tumour but presented as an irreducible inguinal hernia | Right | 51 | 7.0 cm × 6.2 cm | 4 months | Omental fibroma |
| Oyelowo et al[8], 2020 | Appendiceal fibroma in an Amyand's hernia mimicking a supernumerary testis: A case report | Right | 28 | 3 cm × 3 cm × 2 cm | Not reported | Appendiceal fibroma |
| Liu et al[7], 2021 | Omental mass combined with indirect inguinal hernia leads to a scrotal mass: A case report | Left | 30 | 2.5 cm | 1 month | Omental angiofibroma |
The age of the patients ranged from 18 to 51 years. The medical history ranged from 1 to 4 months, and the tumor diameter ranged from 2.5 to 19 cm. Tumor sources included the greater omentum, mesentery, and appendix, all of which are considered benign lesions.
Of all omental tumors, metastatic malignant tumors are the most common, and they mainly occur in the stomach, colon, pancreas, and ovary[1]. Primary peritoneal tumors are rare and can be benign or malignant, accounting for approximately 50% each[2]. Malignant tumors commonly include leiomyosarcoma and hemangiopericytoma. Benign tumors commonly include lipomas, leiomyomas, fibromas, and neurofibromas, with omental fibromas accounting for approximately 2%[3-5]. Cases where tumors fall into the scrotum and manifest as inguinal hernias are even rarer[6-9].
Surgical resection is the main treatment method, in which local resection of benign omental tumors is effective and rarely relapses. Tumor markers, B-ultrasound, and CT examination are helpful for preoperative diagnosis and localization.
Scrotal tumors include primary tumors of the scrotum, metastatic tumors, and tumors that herniate into the abdominal cavity[10]. Primary tumors of the scrotum mainly include testicular tumors and testicular adnexal tumors[11].
The incidence rate of testicular tumors is approximately 1/100000, accounting for 1%-2% of male tumors. More than 90% of testicular tumors are malignant tumors, including germ cell tumors, sex cord/stromal tumors, and secondary tumors, among which germ cell tumors account for more than 90%. Testicular adnexal tumors refer to tumors originating from the epididymis, spermatic cord, white membrane, seminal vesicle, and supporting tissues, which are rarely seen clinically[12,13].
Before surgery, B-ultrasound, CT, MRI, and other examinations are recommended[14,15]. Additionally, complete laboratory tests, such as those for HCG, CEA, AFP, and LDH, are recommended.
The common locations of a hernia sac are the omentum and small intestine, while others include the cecum, appendix, sigmoid colon, bladder, uterine appendages, abdominal tumors, and so on[16]. If the hernia content cannot be returned to the abdominal cavity, the possibility of incarceration, adhesion, and tumor invasion should be considered[17]. However, it should be noted that the appendix, fecal mass, incarceration, edematous intestinal canal, and even extraperitoneal fat are easily misdiagnosed as tumors[18].
Surgeons need to be aware that scrotal masses caused by inguinal hernia can be associated with tumors. In this case report, a patient with a greater omentum tumor complicated with indirect inguinal hernia had a clinical manifestation of a scrotal mass.
The purpose of the surgery was to remove the tumor while repairing the inguinal hernia. During the operation, the hernia sac and its contents were carefully explored, and the tumor was removed. It was then sent for rapid frozen section examination to determine whether the surgical resection scope needed to be expanded and whether a patch should be placed during the operation[19,20]. The type of pathology after surgery determines whether the patient needs further treatment after surgery. Finally, the follow-up work of surgical patients after discharge is also a factor that cannot be ignored.
This case report provides information to help doctors choose an optimal treatment plan, reducing medical risks and ultimately benefiting patients. These are issues that doctors need to consider.
| 1. | Guo YC, Yao LY, Tian ZS, Shi B, Liu Y, Wang YY. Malignant solitary fibrous tumor of the greater omentum: A case report and review of literature. World J Clin Cases. 2021;9:445-456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Zong L, Chen P, Wang GY, Zhu QS. Giant solitary fibrous tumor arising from greater omentum. World J Gastroenterol. 2012;18:6515-6520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Ingle A, Reddy S, Reddy VK. Omental Solitary Fibrous Tumor: A Rare Tumor at Rare Site. J Lab Physicians. 2021;13:283-285. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Garbin O, Hummel M, Diana M, Wattiez A. Solitary fibrous tumor of the great omentum. J Minim Invasive Gynecol. 2011;18:694-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Rodriguez Tarrega E, Hidalgo Mora JJ, Paya Amate V, Vega Oomen O. Solitary fibrous tumor of the greater omentum mimicking an ovarian tumor in a young woman. Gynecol Oncol Rep. 2016;17:16-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Alsaif FA. Mesenteric fibromatosis presenting as an irreducible inguinal hernia. Saudi J Gastroenterol. 2011;17:357-359. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Liu JY, Li SQ, Yao SJ, Liu Q. Omental mass combined with indirect inguinal hernia leads to a scrotal mass: A case report. World J Clin Cases. 2021;9:7850-7856. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Oyelowo N, Halima AO, Muhammed D, Ibrahim AA, Peter O, Muhammed A. Appendiceal fibroma in an Amyand's hernia mimicking a supernumerary testis: a case report. Trop Doct. 2020;50:380-383. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Khoo PJ, Jacob S. An omental fibroma resembling a testicular tumour but presented as an irreducible inguinal hernia. J Surg Case Rep. 2017;2017:rjx161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Swofford BP, Dragovich T. Sigmoid Adenocarcinoma with Regional Scrotal Metastasis. Case Rep Oncol. 2017;10:416-419. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Ghoreifi A, Djaladat H. Management of Primary Testicular Tumor. Urol Clin North Am. 2019;46:333-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Gigantino V, La Mantia E, Franco R, Cecere S, Rossetti S, Di Napoli M, Pisano C, Berretta M, Galzerano A, Botti G, Pignata S, Facchini G. Testicular and testicular adnexa tumors in the elderly. Anticancer Drugs. 2013;24:228-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Philips S, Nagar A, Dighe M, Vikram R, Sunnapwar A, Prasad S. Benign non-cystic scrotal tumors and pseudotumors. Acta Radiol. 2012;53:102-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Tallen G, Hernáiz Driever P, Degenhardt P, Henze G, Riebel T. High reliability of scrotal ultrasonography in the management of childhood primary testicular neoplasms. Klin Padiatr. 2011;223:131-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Lee S, Oh YT, Jung DC. [Imaging of Scrotal Tumors]. Taehan Yongsang Uihakhoe Chi. 2021;82:1053-1065. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 16. | HerniaSurge Group. International guidelines for groin hernia management. Hernia. 2018;22:1-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1355] [Cited by in RCA: 1391] [Article Influence: 173.9] [Reference Citation Analysis (1)] |
| 17. | Gnaś J, Bulsa M, Czaja-Bulsa G. An irreducible left scrotal hernia containing a sigmoid colon tumor (adenocarcinoma) - Case report. Int J Surg Case Rep. 2014;5:491-493. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Sezgin C, Duzgun F, Mutevelizade G, Gumuser G, Sayit E. Inguinoscrotal Bladder Hernia Mimicking Testicle Tumor. Clin Med Insights Case Rep. 2023;16:11795476231151329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 19. | Pahwa HS, Kumar A, Agarwal P, Agarwal AA. Current trends in laparoscopic groin hernia repair: A review. World J Clin Cases. 2015;3:789-792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Liang MK, Holihan JL, Itani K, Alawadi ZM, Gonzalez JR, Askenasy EP, Ballecer C, Chong HS, Goldblatt MI, Greenberg JA, Harvin JA, Keith JN, Martindale RG, Orenstein S, Richmond B, Roth JS, Szotek P, Towfigh S, Tsuda S, Vaziri K, Berger DH. Ventral Hernia Management: Expert Consensus Guided by Systematic Review. Ann Surg. 2017;265:80-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 283] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Hunasanahalli Giriyappa V, India; Richardson WS, United States S-Editor: Li L L-Editor: A P-Editor: Li L