Published online Dec 6, 2024. doi: 10.12998/wjcc.v12.i34.6687
Revised: September 13, 2024
Accepted: September 25, 2024
Published online: December 6, 2024
Processing time: 248 Days and 13.5 Hours
Determination of platybasia and basilar kyphosis are significant parts of routine cranial magnetic resonance (MR) interpretations. These situations may explain a patient’s symptoms or may be associated with other anomalies.
To indicate the interobserver and intraobserver reliability of the skull base angles (SBA) (Koenigsberg standard) and modified SBA (mSBA) measurement techni
In total, 391 patients who had undergone cranial MR imaging were re-assessed regarding the SBA measurements. The SBA and mSBA techniques were used on MR images. Two reviewers independently measured the same angles twice within a 15-day interval, using different monitors. Intraclass correlation coefficient (ICC) was calculated to reveal the intraobserver and interobserver agreements.
There was an excellent agreement between reviewers regarding both angle measurements (ICC was 0.998 for SBA and mSBA). Excellent agreement levels were also observed for intraobserver measurements. ICC was 0.998 for SBA and 0.999 for mSBA for reviewer 1. ICC was 0.997 for SBA and 0.999 for mSBA according to the measurement results of reviewer 2. Higher SBA and mSBA values were observed for females compared to males. There was no correlation between SBA and age for SBA. However, a negative and low-level correlation was observed between mSBA values and age for both reviewers.
SBA and mSBA measurements indicated excellent agreement regarding interobserver and intraobserver diffe
Core Tip: This was a retrospective study to evaluate the interobserver and intraobserver reliability of the skull base angles (SBA) (Koenigsberg standard) and modified SBA (mSBA) measurement techniques. There was an excellent agreement between reviewers. Higher SBA and mSBA values were observed for females compared to males. There was no correlation between SBA and age for SBA. SBA and mSBA measurements showed high agreement for interobserver and intraobserver differences. The study found that SBA angles were reliable measuring methodologies for application on magnetic resonance images.
- Citation: Kizilgoz V, Aydin S, Aydemir H, Keles P, Kantarci M. Interobserver and intraobserver reliability of skull base angles measured on magnetic resonance images. World J Clin Cases 2024; 12(34): 6687-6695
- URL: https://www.wjgnet.com/2307-8960/full/v12/i34/6687.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i34.6687
Platybasia is the term used to define the abnormal flattening of the skull base. Craniofacial anomalies, Arnold-Chiari malformation, cleidocranial dysostosis, and osteogenesis imperfecta are well-known congenital disorders in which platybasia is observed. Morphologically, an abnormal obtuse cranial basal angle is formed, and this angle alteration provides the clue for diagnosing platybasia[1]. On the other hand, platybasia alone is asymptomatic and causes symptoms when observed together with basilar invagination, which describes the upward displacement of the spine into the foramen magnum[2]. Craniocervical kyphosis is another entity in which the skull base angle is lower than expected in normal individuals. Basilar invagination is also associated with this condition, as in platybasia[3].
The first diagnostics methods were described on plain skull radiographs. However, radiographs have been replaced by cross-sectional imaging according to the developing imaging techniques, and new methods have been established using traditional landmarks and on magnetic resonance (MR) images. In this current study, the methods of Koenigsberg et al[1] were used to measure the skull base angles (SBA), including the adapted technique from radiographs and their modified method on MR images. The authors aimed to verify the interobserver and intraobserver reliabilities for both methods and the effect of sex and age on measurements.
After the institutional ethics committee approval (Date: April 5, 2023, Number: 28290, Session: 06, Approval number: E-1845334.11.ED.28290), all patients ≥ 18-years-old who had undergone non-contrast cranial MR examinations during September 2023 were reinterpreted regarding the SBA measurements in this retrospective, cross-sectional study. The authors aimed to measure the angles on skeletally mature patients. They listed the patients using non-enhanced cranial MR imaging and those who were 18 years or older in the picture archiving and communication system (PACS) of our institutional hospital. The MR images of 247 females and 144 males (391 total patients with a mean age of 45.26 ± 16.72 years) were re-interpreted regarding the SBA. The MR images with motion artifacts were excluded from the study; however, no MR studies were observed in this condition among the study population. The workflow of the study is summarized in Figure 1.
A 1.5 tesla MR machine (Siemens Magnetom Era, Erlangen, Germany) with a 16-channel standard head coil was used for all patients undergoing MR imaging. Axial plane T1-weighted spin echo [time to repeat (TR): 434 ms, time to echo (TE): 11 ms, number of excitation (NEX): 1, slice thickness 5 mm], axial plane T2-weighted turbo spin echo (TR: 5600 ms, TE: 103 ms, NEX: 1, slice thickness 5 mm), sagittal T1-weighted turbo spin echo (TR: 449 ms, TE: 9.8 ms, NEX: 1, slice thickness 5 mm), sagittal T2-weighted turbo spin echo (TR: 4810 ms, TE: 81 ms, NEX: 1, slice thickness: 5 mm), axial plane FLAIR (TR: 9000 ms, TE: 84 ms, NEX: 1, slice thickness: 4 mm), and coronal T2-weighted turbo spin echo (TR: 5230 ms, TE: 81 ms, NEX: 1, slice thickness: 5 mm) sequences were used to obtain conventional cranial MR images.
Two radiologists with 11 years and 18 years of experience interpreted the MR images and were blinded to each other. They measured the patients using the PACS system of our institution (Akgün Viewer, v7.5; Etimesgut, Ankara, Türkiye). Each reviewer measured the standard SBA and the modified SBA (mSBA) using the technique described by Koenigsberg et al[1] in the literature. According to this method, the angle formed between the line drawn from the nasion to the center of the hypophysis gland and another line joining the center of hypophysis gland to the anterior border of the foramen magnum indicated the SBA. The line from the tip of the dorsum sella extending across the anterior cranial fossa and a second line drawn along the posterior margin of the clivus formed the mSBA (Figure 2). Each reviewer measured both these angles twice within a 15-day interval on independent panels using the same PACS system. The angles were measured to the hundredths place. The reviewers evaluated the patients in a randomized order for each reviewing period, which was different from each other[2,3].
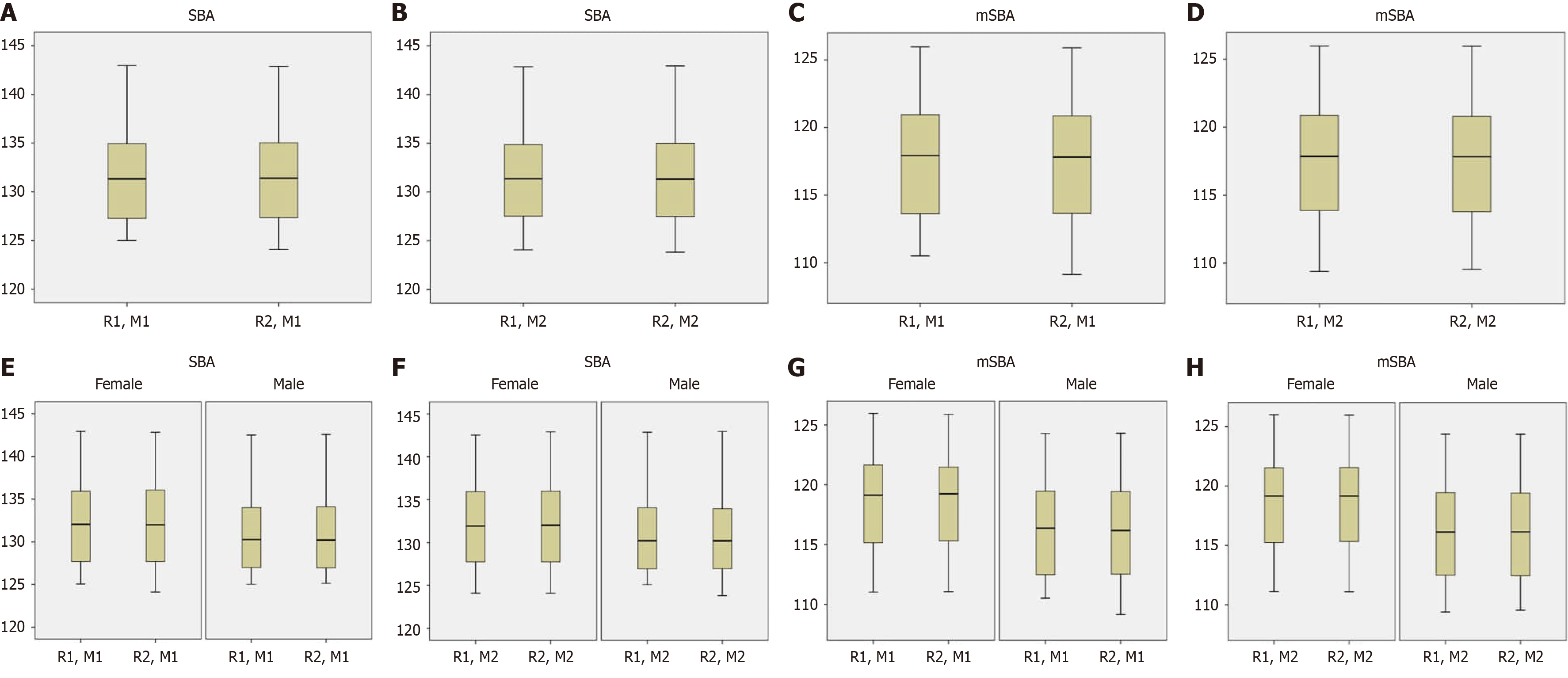
All statistical analyses were calculated using SPSS statistics v22.0 for Windows (IBM Corp., Armonk, NY, United States). Intraclass correlation coefficient (ICC) values were presented to determine the interobserver and intraobserver agreement levels. The classification method from Koo et al[4] was used to represent the agreement levels. According to these agreement levels, values less than 0.50 indicated poor, values between 0.50 and 0.75 showed moderate, values between 0.75 and 0.90 revealed good, and values greater than 0.90 pointed out an excellent agreement[4]. Data distributions of each reviewer were presented with box-plot analyses. Shapiro-Wilk tests were carried out to reveal the distribution characteristics of the data obtained. Due to the data distribution characteristics, non-parametric tests (Mann-Whitney U tests) were carried out for sex differences. Spearman’s Rho correlation test was carried out to verify the correlation between the measured angles and age. P values less than 0.05 indicated significance.
In this study, 247 females and 144 males (n =391 patients) were reinterpreted regarding the SBA. The demographic data of the patients involved in the study are summarized in Table 1. There was excellent agreement between each measurement of the reviewers and between two different reviewers regarding SBA and mSBA measurements. Intraobserver comparisons also indicated an excellent agreement for SBA and mSBA measurements (Table 2). The data distributions regarding the SBA measurements were presented in box plots (Figure 3).
| Characteristics | n |
| Sex | |
| Total, n = 391 | |
| Females | 247 (63.2) |
| Males | 144 (36.8) |
| Age | |
| Mean | 45.26 |
| Standard deviation | 16.72 |
| Minimum | 18 |
| Maximum | 96 |
| Age groups | |
| 18 and 19 | 18 |
| 20-29 | 63 |
| 30-39 | 72 |
| 40-49 | 77 |
| 50-59 | 71 |
| 60-69 | 60 |
| 70-79 | 21 |
| 80-89 | 8 |
| 90-99 | 1 |
| Parameter | Subparameter | 95 %CI | Intraclass correlation coefficient | |
| Lower bound | Upper bound | |||
| Reviewer 1 | SBA | 0.998 | 0.999 | 0.998 |
| mSBA | 0.999 | 0.999 | 0.999 | |
| Reviewer 2 | SBA | 0.997 | 0.998 | 0.997 |
| mSBA | 0.999 | 0.999 | 0.999 | |
| R1 vs R2 for M1 | SBA | 0.997 | 0.998 | 0.998 |
| mSBA | 0.998 | 0.999 | 0.998 | |
| R1 vs R2 for M2 | SBA | 0.996 | 0.997 | 0.996 |
| mSBA | 0.999 | 0.999 | 0.999 | |
Higher SBA measurement results were observed for both reviewers in females than in males. There were also higher values measured for females than in males regarding mSBA measurements (Table 3).
| Interpretations by the reviewers | Female | Male | P value |
| SBA | |||
| R1 | 132.19 ± 4.88 | 130.92 ± 4.52 | 0.011 |
| R2 | 132.22 ± 4.88 | 130.96 ± 4.49 | 0.012 |
| mSBA | |||
| R1 | 118.23 ± 3.72 | 116.20 ± 3.66 | < 0.001 |
| R2 | 118.19 ± 3.70 | 116.20 ± 3.63 | < 0.001 |
The correlation analysis between SBA measurements and age indicated a low-level, negative, and significant correlation between mSBA and age for both reviewers. However, no significant correlation was observed between SBA and age (Table 4).
| Measurement and reviewer | Correlation coefficient | P value |
| SBA measurement by R1 | 0.014 | 0.788 |
| SBA measurement by R2 | 0.021 | 0.685 |
| mSBA measurement by R1 | -0.235 | < 0.001 |
| mSBA measurement by R2 | -0.233 | < 0.001 |
The terms platybasia and basilar invagination were used interchangeably for a long time. Basilar invagination is the prolapse of the vertebral column into the foramen magnum; however, platybasia defines an abnormal obtuse angle between the anterior skull base and the clivus[5]. Basilar invagination is often associated with other anomalies of the craniovertebral junction, including an incomplete ring of the atlas, atlantooccipital assimilation, and hypoplasia of the basiocciput, occipital condyles, or atlas. This condition is also associated with neuronal axis abnormalities such as Chiari malformation, syringobulbia, syringomyelia, and hydrocephalus[6].
In the recent classification of the basilar invagination, type 1 indicates the odontoid process invaginates inside the foramen magnum, and type 2 represents the flattened cranium base[7]. In both types of basilar invagination, an increased clivus-axial angulation and ventral compression of the skull base to neuronal structures are observed[3].
Platybasia is suggested to be more prevalent in type 2 basilar invagination than in type 1. Patients with platybasia have a more acute clivus canal angle. In addition, they show greater cervical lordosis than patients without platybasia[8]. Craniocervical alterations have also been mentioned to be associated with voice production or the development of a more forward head posture[9]. Craniocervical and craniomedullar angle alterations have also been shown to be associated with cervicogenic headache[10].
The basis of the cranium is involved in specific measurements to measure the craniocervical stability, which relies on the integrity of the craniocervical junction[11]. Angular craniometry angles may be divided into four main groups based on past studies in the literature. Two represent the primary cranial angles, while the other two measurements are secondary cranial angles. The basal angle and Boogard’s angle are the primary cranial angles. Basal angle is defined as the angle formed by lines from the nasion to the top of the dorsum sella and from this point to the basion. Boogard’s angle is formed between the top of the dorsum sella, basion, and opisthion[8]. These methods used to be performed by skull radiographs, which are now uncommon, and a modification of these methods to MR imaging has become mandatory. Koenigsberg et al[1] adopted the SBA measuring methodology utilizing the traditional landmarks in plain radiographs and applied this technique to midline sagittal MR images. They also developed a modified skull base measurement technique, presented the results along with the conversant method, and reported in their study with normal ranges of the angles. Both the standard and the modified method provided lower measurement values than those previously presented in studies via traditional radiographies[1].
The reliability of the craniocervical measurements has been previously mentioned. The head position in relation to the cervical spine has been studied on lateral radiographs, and the nasal-sella line/odontoid process tangent provided very high intraobserver and interobserver ICC values (0.99 and 0.97 for each reviewer and 0.98 for the interobserver) in a study with 39 healthy female subjects[12]. Upright dynamic MR imaging was used in another study with 50 adults and presented moderate to excellent agreement for four measures of craniocervical stability, including basion-axial interval, basion-axial angle, the Grabb-Oakes line, and basion-dens interval[11]. The angle of the odontoid apex to Chamberlain’s line had excellent, Boogard’s angle had good to excellent, clivo-axial and clivo-dens angles provided good, and clivo-palate angle had moderate to good inter-rater reliability in a study using computerized tomography and MR images of 42 patients with basilar invagination and 79 controls[13].
Some authors studied the cervicomedullar angle, which is another parameter to be measured other than bony structures. The line that passes through the ventral side of the medulla oblongata and the line that passes along the ventral surface of the upper cervical spinal cord formed this angle. A study by Wang et al[14] reported excellent intraobserver repeatability and interobserver reliability for cervicomedullar angle measured on the MR images of 200 adult Chinese patients[14].
This current study focused on the angles to be measured on bony structures of the skull base, independent from C2 vertebra, dens, or cervical axis, and excellent intra- and inter-observer agreements were calculated in a relatively greater number of patients among the other studies in the literature. The reviewers of the research evaluated the same patient list in a randomized order for each reviewing period that was different from each other to determine the repeatability and reproducibility of the SBA measurements.
There was no difference between female and male groups regarding the basal angle measurements in a study with 49 adult patients who underwent computed tomography examination with suspected vascular conditions unrelated to the craniovertebral junction anomalies (P = 0.84)[15]. Another study performed the basal angle measurements on MR images, including 200 adults and 50 children, and reported a good interobserver agreement with a Pearson correlation coefficient of 0.85. There was no difference between females and males regarding the basal angle measurements in the study, and the P values were 0.238 and 0.930 for each reviewer.
In another study, age groups were established as under 26-years-old, between 26-years-old and 60-years-old, and more than 60-years-old. No differences were observed between these age groups according to each reviewer’s measurement results (P values were 0.328 and 0.475 for each reviewer)[16]. Both these studies used the term basal angle indicating the mSBA angle in this current study; therefore, to compare our results with these reports, higher mSBA angles were obtained in the female group, unlike these past studies. In addition, a low-level, negative, and significant correlation between mSBA and age was revealed according to the results of this current study.
Lateral cranial radiographs were useful to evaluate skull base anomalies in the beginning, and the measurement techniques were applied to diagnose or rule out these conditions such as platybasia or cranial kyphosis were based on radiographic landmarks. Using an appropriate dose, technique, and positioning, a two-dimensional radiographic projection of the three-dimensional skull provided these landmarks to be obvious and guided the SBAs to be measured accurately. Adaptation of these measurement methods to cross-sectional images was necessary since radiographies have been replaced by cross-sectional imaging techniques.
This study aimed to assess the usability of this technique on MR images and the methods published by Koenigsberg et al[1] were applied to obtain datasets in this current study; however, technical adaptation was not easy in some cases. The sagittal slices were not always projected on the exact mid-sagittal plane and the nearest plane to the mid-sagittal slice were used to perform the measurements. The millimetric slice thicknesses (5 mm in this study for the sagittal plane T1 weighted images) in this situation were slightly challenging and time consuming. The high ICC values of interobserver and intraobserver agreement indicated that these angle measurements can be successfully adapted to MR images.
T1-weighted images have been used because it has the superiority to reveal the anatomical details as in previous morphological evaluations in the literature; however, a 1.5 tesla MR machine was used in this research. Using 3.0 tesla MR devices or higher magnetic field strength would provide clearer anatomical detail and depict the bony borders better. On the other hand, the aim of the study was performing the SBAs in a more widely used 1.5 tesla MR machine, by which most of the MR images were obtained in our daily practice. The regular angle measurement function of the PACS system of our institution was used in this research. No other complex programs, additional software, or post processing was required to perform the angle measurements. The purpose of the current research was to indicate the interobserver and intraobserver agreement levels of the SBAs using the MR images rather than diagnosing skull base anomalies. As an interesting side note, the reviewers did not encountered any skull base anomalies in the study population during the data collection of this study.
There were limitations of the study. First, the reviewers in this study were experienced specialists with many years of practice. Measurement results, including less experienced specialists or residents, would be beneficial to understand the reliability of the measurement techniques. Second, two radiologists performed the measurements; however, inter
Performing the SBA measurements on a large number of patient images by a research team including a large group of various specialists with different levels of expertise would provide better information to clarify the aim of this research. This effort is expected to add valuable information to the literature.
Intraobserver and interobserver ICC calculations revealed an excellent agreement regarding SBA and mSBA mea
| 1. | Koenigsberg RA, Vakil N, Hong TA, Htaik T, Faerber E, Maiorano T, Dua M, Faro S, Gonzales C. Evaluation of platybasia with MR imaging. AJNR Am J Neuroradiol. 2005;26:89-92. [PubMed] |
| 2. | Ferreira JA, Botelho RV. Determination of Normal Values of the Basal Angle in the Era of Magnetic Resonance Imaging. World Neurosurg. 2019;132:363-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Botelho RV, Ferreira JA, Zandonadi Ferreira ED. Basilar Invagination: A Craniocervical Kyphosis. World Neurosurg. 2018;117:e180-e186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9979] [Cited by in RCA: 17998] [Article Influence: 1799.8] [Reference Citation Analysis (1)] |
| 5. | Shah A, Serchi E. Management of basilar invagination: A historical perspective. J Craniovertebr Junction Spine. 2016;7:96-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Smith JS, Shaffrey CI, Abel MF, Menezes AH. Basilar invagination. Neurosurgery. 2010;66:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 122] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 7. | Botelho RV, Diniz JM. Basilar Invagination: cranio-cervical kyphosis rather than prolapse from the upper cervical spine. J Neurol Neuromedicine. 2017;2:15-19. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Botelho RV, Ferreira ED. Angular craniometry in craniocervical junction malformation. Neurosurg Rev. 2013;36:603-10; discussion 610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 9. | Miller NA, Gregory JS, Semple SI, Aspden RM, Stollery PJ, Gilbert FJ. The effects of humming and pitch on craniofacial and craniocervical morphology measured using MRI. J Voice. 2012;26:90-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Çoban G, Çöven İ, Çifçi BE, Yıldırım E, Yazıcı AC, Horasanlı B. The importance of craniovertebral and cervicomedullary angles in cervicogenic headache. Diagn Interv Radiol. 2014;20:172-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Nicholson LL, Rao PJ, Lee M, Wong TM, Cheng RHY, Chan C. Reference values of four measures of craniocervical stability using upright dynamic magnetic resonance imaging. Radiol Med. 2023;128:330-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Gadotti IC, Armijo-Olivo S, Silveira A, Magee D. Reliability of the craniocervical posture assessment: visual and angular measurements using photographs and radiographs. J Manipulative Physiol Ther. 2013;36:619-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Baysal B, Eser MB, Sorkun M. Radiological approach to basilar invagination type B: Reliability and accuracy. J Neuroradiol. 2022;49:33-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Wang S, Wang C, Passias PG, Li G, Yan M, Zhou H. Interobserver and intraobserver reliability of the cervicomedullary angle in a normal adult population. Eur Spine J. 2009;18:1349-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Dash C, Singla R, Agarwal M, Kumar A, Kumar H, Mishra S, Sharma BS. Craniovertebral junction evaluation by computed tomography in asymptomatic individuals in the Indian population. Neurol India. 2018;66:797-803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Hirunpat S, Wimolsiri N, Sanghan N. Normal Value of Skull Base Angle Using the Modified Magnetic Resonance Imaging Technique in Thai Population. J Oral Health Craniofac Sci. 2017;2:017-021. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/