Published online Oct 26, 2024. doi: 10.12998/wjcc.v12.i30.6383
Revised: July 26, 2024
Accepted: August 22, 2024
Published online: October 26, 2024
Processing time: 130 Days and 11 Hours
We planned this study considering that complications of deep neck infections can be seriously life threatening.
To raise awareness that introthoracic complications and necrotizing fasciitis are causes of serious mortality and morbidity.
This study was carried out with the participation of 188 patients who were treated at Mersin University Department of Otorhinolaryngology and Head and Neck Surgery at January 1, 2024. When the patient files were retrospectively examined, 16 of 188 patients (8.5%) were included in the study because they were observed to have necrotizing fasciitis and/or intrathoracic complications.
There were a total of 16 patients in this study, 9 males (56.25%) and 7 females (43.75%). All patients were adults (> 18 years) and the mean age was 50.37 years ± 15.37 years. Female patients had a mean age of 40.42 years ±13.38 years, whereas for male patients was 58.11 years ± 12.44 years.
Patients with necrotizing fasciitis and/or intrathoracic complications require more complicated and serious surgeries, intensive care unit monitoring, and mechanical ventilator support. Higher rates of morbidity and mortality should be expected in these patients who are hospitalized for longer periods of time.
Core Tip: Intrathoracic complications and necrotizing fasciitis are feared serious complications of deep neck infections. The need for aggressive surgery and long term hospitalization make this disease important. Emergency Medicine Specialists and Otolaryngologists should know the management and possible complications of these patients well and act quickly.
- Citation: Bal KK, Aslan C, Gür H, Bal ST, Ustun RO, Unal M. Deep neck infections mortal complications: Intrathoracic complications and necrotising fasciitis. World J Clin Cases 2024; 12(30): 6383-6390
- URL: https://www.wjgnet.com/2307-8960/full/v12/i30/6383.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i30.6383
Deep neck infections (DNIs) were first described by Galen in the second century[1]. DNIs are infections of cervical fascias and potential anatomical cervical spaces that can clinically vary from cellulitis/phlegmon to gross abscesses. The frequency of DNIs has decreased with the widespread use of antibiotics. However, owing to diagnosis and treatment delays, they can spread rapidly in the neck and mediastinum through the cervical spaces and cause various complications that result in serious morbidity and mortality. These complications include airway obstruction, necrotizing fasciitis, mediastinitis, pulmonary emphysema, pleural effusion, pericarditis, Lemierre syndrome, major artery/vein rupture, and sepsis[2]. Currently, the most common etiology of DNIs in adults is odontogenic infections, whereas the most common cause in the pediatric age group is tonsillopharyngitis. Lymphadenitis, salivary gland infections (sialadenitis and sialolithiasis), trauma, foreign bodies, invasive medical procedures (iatrogenic), intravenous drug use and addiction, congenital cysts, thyroiditis, and laryngoceles are other etiological causes. In addition, systemic diseases such as tuberculosis, cat scratch disease, toxoplasmosis, acquired immunodeficiency syndrome (AIDS), actinomycosis, syphilis, tularemia, brucellosis, Kawasaki disease, Kikuchi-Fujimoto disease, sarcoidosis, rheumatoid arthritis, and systemic lupus erythematosus are included in the etiology because they can cause suppurative lymphadenitis. However, the etiological cause cannot be determined in 20%-50% of patients[3-6].
Symptoms and signs vary according to disease progression and the site of involvement. The most common symptoms are pain, fever, and neck swelling and redness. In addition, heat increase, dysphagia, odynophagia, dyspnea, stridor, dysphonia, limited neck movements (torticollis), trismus, and crepitation may also be observed depending on the location of the infection. Loss of appetite, restlessness, and fatigue may also be observed in pediatric patients[6-9]. Although Streptococcus species and Staphylococcus aureus are the most common pathogens in microbiological examination of samples taken from DNIs patients, DNIs are generally multimicrobial infections. Aerobic pathogens are common; however, since anaerobic bacteria are difficult to grow in culture, they cause infection at a higher rate than reported[10-12]. In addition to anamnesis and physical examination, laboratory tests, ultrasonography, computed tomography (CT), magnetic resonance imaging, arteriography, and aspiration or puncture can be used to diagnose DNIs[13]. In the treatment of DNIs, combined medical antibiotic treatment and surgical drainage/debridement are the main modalities that ensure airway safety[6,7].
In this study, we aimed to retrospectively examine our patients who presented to our clinic in the last decade with intrathoracic complications and/or necrotizing fasciitis due to DNIs in terms of epidemiology, etiology, diagnosis and treatment methods, and postoperative follow-up, in light of the current literature.
This retrospective study included 16 patients who were hospitalized at the Department of Otolaryngology and Head and Neck Surgery, University of Mersin, at January 1, 2024, for necrotizing fasciitis and/or intrathoracic complications such as mediastinitis due to DNIs. Of the 188 patients who applied within 10 years, 172 were excluded because they did not have necrotizing fasciitis and/or mediastinitis (16 of 188 DNIs patients have necrotizing fasciitis and/or mediastinitis, 8.5%). This study was approved by the University of Mersin Clinical Research Ethics Committee (date: July 24, 2024, decision number: 703). All patients provided written and verbal informed consent for the publication of the details and images.
Hospitalized patients who underwent surgical and medical treatments were included in the study. Demographics, complaints, medical history, clinical symptoms and findings, preoperative CT scans and intraoperative photographs, bacterial culture results, antibiotics and their revision records, hospitalization time, infection etiology, affected cervical spaces, need for mechanical ventilation and intensive care unit admission, and postoperative follow-up were recorded for each patient. Patients who did not have necrotizing fasciitis and/or mediastinitis, were under the age of 18 years, had incomplete data, or were not hospitalized in the Otolaryngology Department were excluded from the study.
We examined the records of our hospital’s information processing automation system and archive unit. The patients and applications for the same disease conditions were examined individually. These factors were considered in this study. Statistically, the P value was not calculated. All given values are arithmetic mathematical values. No biostatistical software program was used.
In total, 16 patients were included in this study: 9 men (56.25%) and 7 women (43.75%). All patients were adults (> 18 years), and the mean age was 50.37 years ± 15.37 years. Female patients had a mean age of 40.42 years ± 13.38 years, whereas for male patients, the mean age was 58.11 years ± 12.44 years.
While three (18.75%) patients had no comorbidities, 13 (81.25%) had comorbidities. The most common comorbid disease was diabetes mellitus (62.5%). Hypertension and chronic ischemic heart disease were the second and third most common comorbidities, respectively.
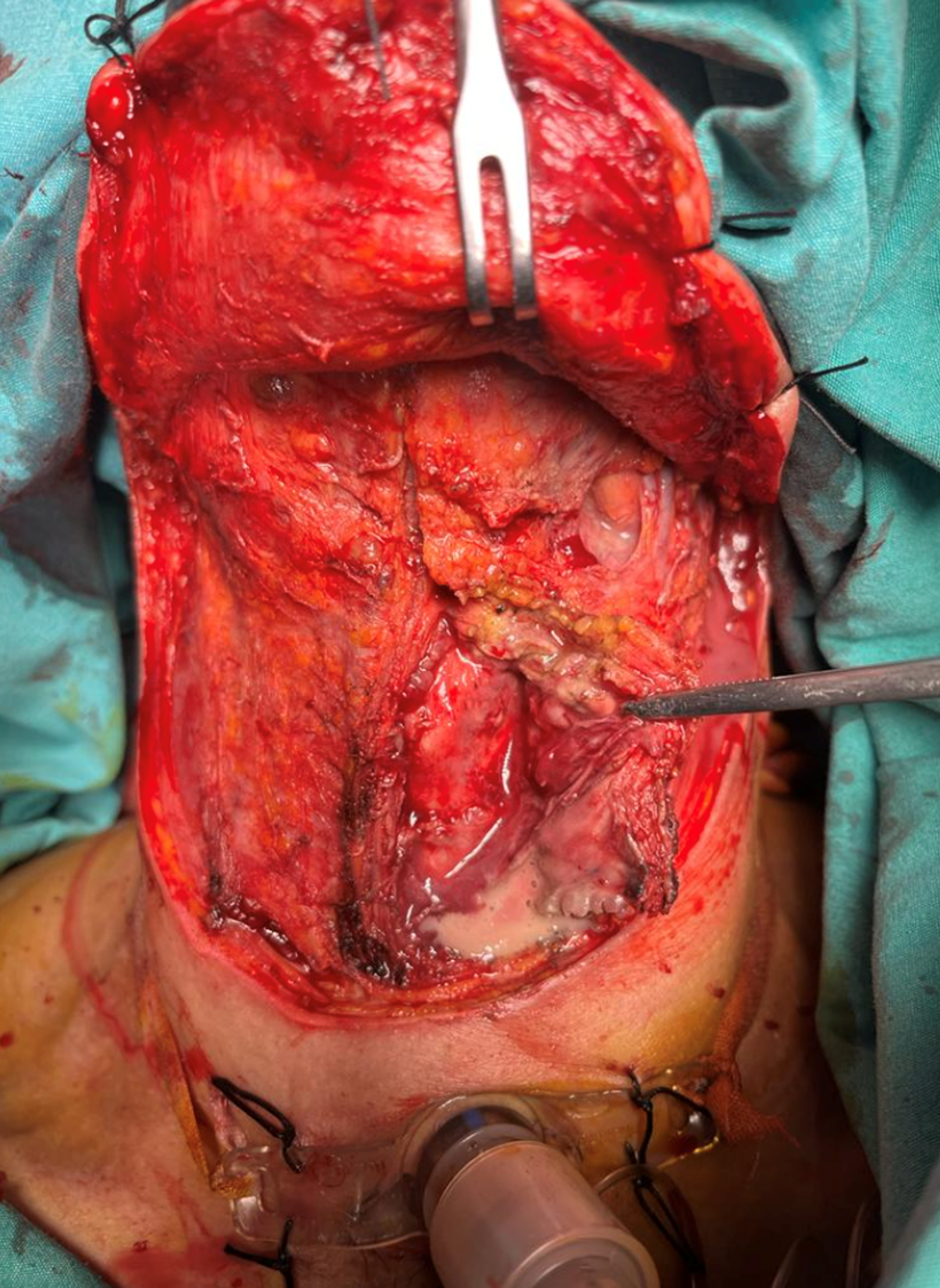
All patients underwent preoperative contrast-enhanced neck and thoracic CT. The most common finding on physical examination was pain (87.5%), followed by fever (68.75%) and dysphagia (62.5%). Other findings included dyspnea, neck crepitation, and neck enlargement. In all the patients, more than one neck region was involved. The most frequently affected regions were submandibular (81.25%), parapharyngeal (62.5%), and retropharyngeal (31.25%) regions, respectively. Two patients had an infection in the posterocervical region, and one patient had an infection in the supraclavicular region. The etiology was odontogenic in 11 (68.75%) patients, tonsillitis in two (12.5%) patients, skin infection in two (12.5%) patients, and no etiology could be found in one (6.25%) patient. While isolated necrotizing fasciitis was present in 15 patients, additional intrathoracic complications were observed in five patients. Intrathoracic complications without necrotizing fasciitis occurred in only one patient. The most common intrathoracic complications were mediastinitis and pleural effusion. The patients with intrathoracic complications underwent video-assisted thoracoscopic surgery (VATS), thoracotomy, and neck exploration. While VATS was performed in one patient, classical thoracotomy was conducted in four patients. A thoracic tube was inserted in these five patients in the same session.
The average hospitalization time of the patients was 22.31 days ± 12.57 days. Twelve patients (75%) were followed in intensive care. Postoperative mechanical ventilation was required in four of these patients (33.3%). The average length of stay in the intensive care was 12.75 days ± 6.12 days. Tracheotomy was performed in five of the patients (31.25%). One patient (6.25%) died on postoperative day 5. This patient had necrotizing fasciitis with no intrathoracic complications.
Bacterial growth was observed in tissue and abscess cultures of 11 patients. Two patients harbored more than one pathogen: methicillin-sensitive coagulase-negative Staphylococcus in five patients (45.45%), methicillin-resistant Staphylococcus aureus in three patients (27.27%), Streptococcus viridans in one patient (9.09%), Escherichia coli in one patient (9.09%), and Enterococcus in one patient (9.09%).
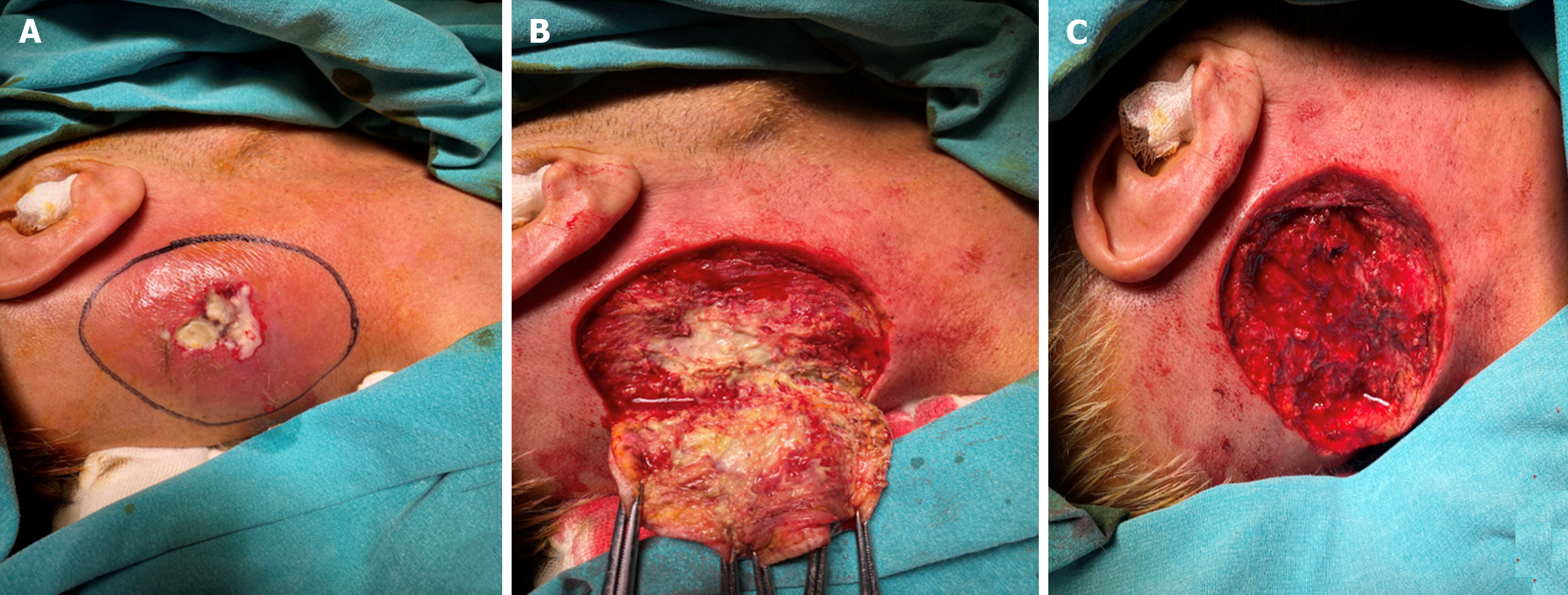
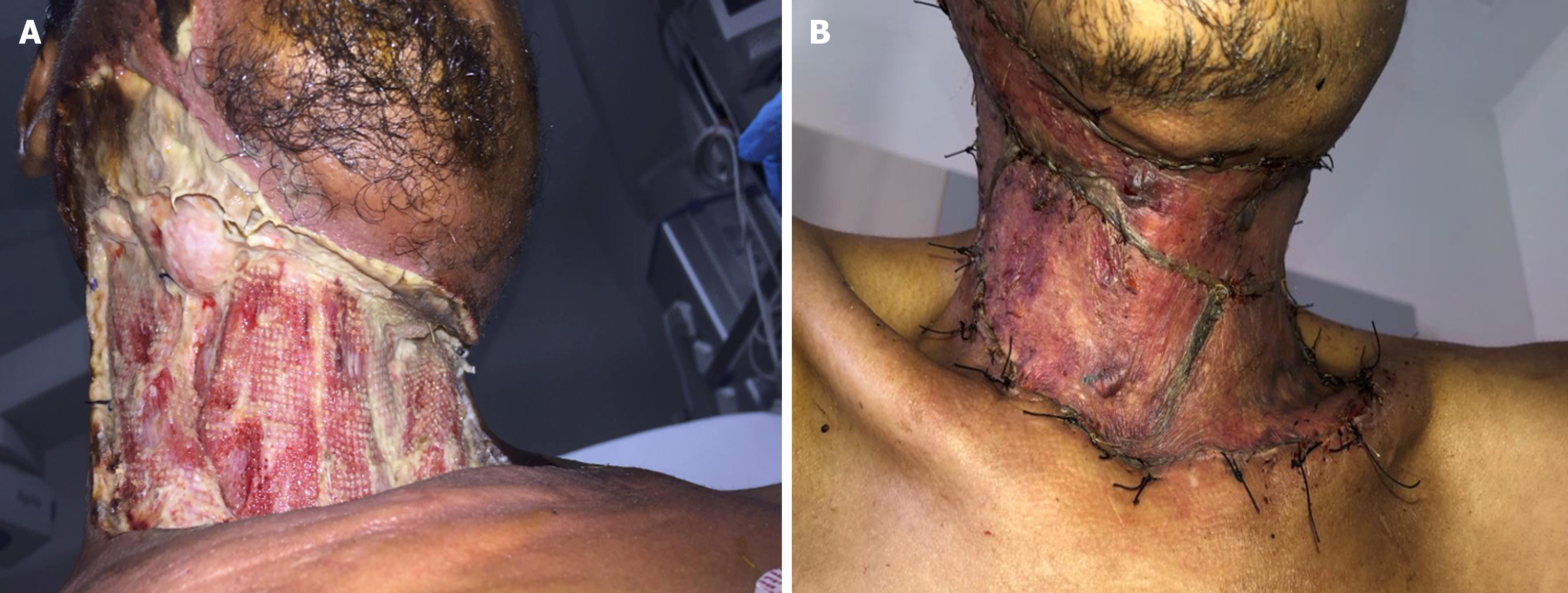
Antibiotic treatment was revised in eight (50%) patients during follow-up. While necrotizing fasciitis patients were subjected to daily wound debridement under local anesthesia, one of our patients (6.25%) required re-exploration under general anesthesia. In all patients, intravenous empirical antibiotic and surgical treatments were combined. Four patients (25%) additionally received hyperbaric oxygen therapy during postoperative follow-up. Skin grafting was performed on five patients with skin and tissue defects by plastic and reconstructive surgeons during the postoperative period. Patients were routinely administered oral amoxicillin, clavunate, or cefdinir for 10-14 days after discharge.
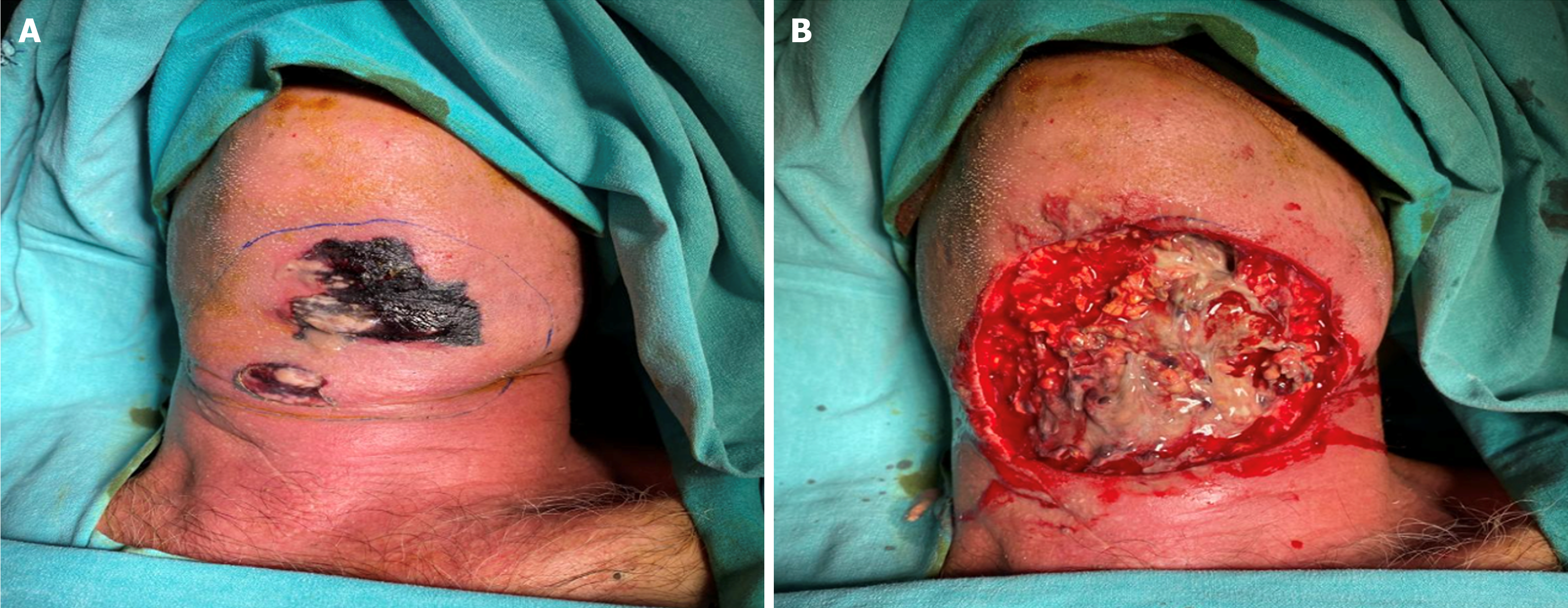
The patients’ preoperative, intraoperative, and postoperative images and tomography sections are shown in Figures 1, 2, 3, 4, 5 and 6, and a striking intraoperative video (Video) has been added.
DNIs are infective conditions of the cervical fascias and anatomical potential spaces formed by these fascias. DNIs and their complications are more common in men than in women (male/female ratio 1.77-1.3:1)[12]. In our study, the male/female ratio was 1.28:1, similar to that reported in the literature.
In the absence of broad-spectrum antibiotics, DNIs are most commonly caused by tonsillopharyngitis and upper respiratory tract infections and more frequently develop within the parapharyngeal area. The prevalence of tonsillopharyngitis-induced DNIs has decreased because of the widespread use of antibiotics in the early period. Currently, DNIs mostly develop in the submandibular area because of odontogenic infections. Tonsillopharyngitis is the most common cause in children[12,14-16].
All the patients in our study were adults, and the most common etiological factor was odontogenic infection (68.75%). Diabetes mellitus is the most common comorbidity in the literature[6,14]. In our study, in accordance with the literature, DM was the most common comorbid disease (62.5%); hypertension and chronic ischemic heart disease were other common comorbid diseases.
In Adoviča et al’s study in 36.2% of the patients and Treviño-Gonzalez et al’s study in 76% of the patients, the submandibular region was the most affected area[12,17]. In our study, the most affected region was the submandibular region (81.25%), consistent with previous findings.
Early diagnosis and treatment are important for the prognosis of DNIs. Once airway safety is ensured, surgical drainage/debridement and broad-spectrum antibiotics are the primary treatment modalities. Preoperative contrast-enhanced neck and thoracic CT is important for the diagnosis of complications and surgical planning. Detection of the causative pathogen in culture and revision of empirical treatment are crucial for the treatment and course of the disease[10-12]. In our clinical practice, we routinely request contrast-enhanced CT of the neck and thoracic sections, including the upper mediastinum, for all cases with suspicious clinical, laboratory, or physical examination findings. We strongly recommend that all clinicians dealing with DNIs cases routinely request neck-limited thoracic (including the upper mediastinum) CT and, in case of doubt, imaging of the entire thorax.
DNIs are polymicrobial, and the most common pathogens are staphylococci and streptococci[12,14,17,18]. Combined with surgery, broad-spectrum empiric systemic antibiotic treatment that is effective against aerobic and anaerobic bacteria is essential for the treatment of DNIs. Currently, combinations of ampicillin-sulbactam, metronidazole, and third-generation cephalosporins are most commonly used in systemic empiric antibiotic treatment[12,14-16]. DNIs spread rapidly into the neck and mediastinum through the cervical cavities, causing various complications that can lead to serious morbidity and mortality. Complications include airway obstruction, necrotizing fasciitis, mediastinitis, pulmonary emphysema, pleural effusion, pericarditis, Lemierre syndrome, major artery/vein rupture, and sepsis. In patients who develop complications, the need for surgery, duration of hospitalization and intensive care unit stay, morbidity, and mortality increase[19-22]. In a study by Treviño-Gonzalez et al[17], the average hospitalization period in patients with DNIs was 8.55 days, while it was 27 days in patients who developed complications. In Ban et al’s study, tracheotomy was performed in 32.9% of DNIs patients, and this rate was 9.2% in Crespo et al’s study[20,23]. The mortality rate of uncomplicated DNIs is 1%-12% but is 10%-40% in patients who develop necrotizing fasciitis and mediastinitis[19-22]. Rapid and radical surgical debridement is important in patients with necrotizing fasciitis. Although an average of three debridements is performed per patient, we perform a large number of debridements in our clinical practice. In line with the literature, we believe that it is beneficial to keep in mind the option of elective tracheotomy in the first session in patients whose repeated debridement is anticipated to be performed under general anesthesia. We use povidone-iodine, hydrogen peroxide, warm saline, and boric acid in powder form for wound cleaning and care after debridement. Repetitive debridement and curettage of necrotic tissues, antibiotic selection compatible with broad-spectrum bacterial culture, and simultaneous hyperbaric oxygen therapy have become indisputable treatment modalities for this patient group[22]. We believe that boric acid in the powder form is beneficial because it creates a suitable granulation ground for skin grafts to be applied in subsequent sessions.
The mortality risk of descending mediastinitis is high and is more fatal in adults than in children. Aggressive treatment is essential, regardless of age. Transthoracic and thoracoscopic methods are preferred for mediastinitis treatment. If left untreated, the mortality rate of mediastinitis is 85%. More than 50% of cases of descending necrotizing fasciitis (DNM) are odontogenic. Poor oral hygiene, diabetes, AIDS, intravenous drug abuse, and chronic alcoholism are predisposing factors for DNM. According to the classification of mediastinitis by Endo et al[20], the surgical options include transcervical drainage, subxiphoidal mediastinal drainage without sternotomy, and classical thoracotomy. Guan et al[24] created a DNM classification system. The authors also mentioned transcervical mediastinal drainage, infraxiphoid thoracoscopy, VATS, and classical thoracotomy. In the common opinion of the authors, VATS is an excellent option for the treatment of early-stage DNM[24-27]. The VATS rate in our DNM cases (some of our patients had additional problems such as pneumonia-pleural effusion-empyema) was 20%. The reason why we performed surgery with classical thoracotomy in 80% of our patients was that Type IIb and Type 3 cases took up more space in our case series, and most of our patients were not considered early-stage DNM and could not benefit from VATS.
In our study, the average hospitalization time was 22.31 days ± 12.57 days. Twelve patients (75%) were followed in intensive care, four of whom (33.3%) required postoperative mechanical ventilation. The average length of stay in intensive care was 12.75 days ± 6.12 days. Tracheotomy was performed in five of the patients (31.25%). One of our patients died in the postoperative period (6.25%). Consistent with the literature, staphylococci and streptococci were the most common pathogens. Antibiotic treatment was revised in eight patients (50%) during follow-up.
DNIs are one of the otolaryngology emergencies and a serious public health problem by causing high mortality and morbidity. Ensuring airway safety is the first principle of the treatment. Patients with necrotising fasciitis and/or intrathoracic complications need more complicated surgeries, intensive care and mechanic ventilation, have a higher morbidity–mortality and longer hospitalisation period. Because of that; early diagnosis, aggressive surgical treatment and medical management contribute to improved survival.
| 1. | Chen MK, Wen YS, Chang CC, Huang MT, Hsiao HC. Predisposing factors of life-threatening deep neck infection: logistic regression analysis of 214 cases. J Otolaryngol. 1998;27:141-144. [PubMed] |
| 2. | Cordesmeyer R, Kauffmann P, Markus T, Sömmer C, Eiffert H, Bremmer F, Laskawi R. Bacterial and histopathological findings in deep head and neck infections: a retrospective analysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2017;124:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Yang SW, Chen TM, Chen TA. Migrating fish bone complicating a deep neck abscess. Chang Gung Med J. 2005;28:872-875. [PubMed] |
| 4. | Ungkanont K, Yellon RF, Weissman JL, Casselbrant ML, González-Valdepeña H, Bluestone CD. Head and neck space infections in infants and children. Otolaryngol Head Neck Surg. 1995;112:375-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Plaza Mayor G, Martínez-San Millán J, Martínez-Vidal A. Is conservative treatment of deep neck space infections appropriate? Head Neck. 2001;23:126-133. [PubMed] [DOI] [Full Text] |
| 6. | Bal KK, Unal M, Delialioglu N, Oztornaci RO, Ismi O, Vayisoglu Y. Diagnostic and therapeutic approaches in deep neck infections: an analysis of 74 consecutive patients. Braz J Otorhinolaryngol. 2022;88:511-522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Gidley PW, Ghorayeb BY, Stiernberg CM. Contemporary management of deep neck space infections. Otolaryngol Head Neck Surg. 1997;116:16-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 8. | Har-El G, Aroesty JH, Shaha A, Lucente FE. Changing trends in deep neck abscess. A retrospective study of 110 patients. Oral Surg Oral Med Oral Pathol. 1994;77:446-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 128] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Tom MB, Rice DH. Presentation and management of neck abscess: a retrospective analysis. Laryngoscope. 1988;98:877-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Martínez Pascual P, Pinacho Martinez P, Friedlander E, Martin Oviedo C, Scola Yurrita B. Peritonsillar and deep neck infections: a review of 330 cases. Braz J Otorhinolaryngol. 2018;84:305-310. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Shimizu Y, Hidaka H, Ozawa D, Kakuta R, Nomura K, Yano H, Watanabe KI, Katori Y. Clinical and bacteriological differences of deep neck infection in pediatric and adult patients: Review of 123 cases. Int J Pediatr Otorhinolaryngol. 2017;99:95-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 12. | Adoviča A, Veidere L, Ronis M, Sumeraga G. Deep neck infections: review of 263 cases. Otolaryngol Pol. 2017;71:37-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Nagy M, Backstrom J. Comparison of the sensitivity of lateral neck radiographs and computed tomography scanning in pediatric deep-neck infections. Laryngoscope. 1999;109:775-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Bakir S, Tanriverdi MH, Gün R, Yorgancilar AE, Yildirim M, Tekbaş G, Palanci Y, Meriç K, Topçu I. Deep neck space infections: a retrospective review of 173 cases. Am J Otolaryngol. 2012;33:56-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Kataria G, Saxena A, Bhagat S, Singh B, Goyal I, Vijayvergia S, Sachdeva P. Prevalence of odontogenic deep neck space infections (DNSI): a retrospective analysis of 76 cases of DNSI. Int J Otorhinolaryngol Head Neck Surg. 2015;1:11. [DOI] [Full Text] |
| 16. | Doležalová H, Zemek J, Tuček L. Deep Neck infections of Odontogenic Origin and Their Clinical Significance. A Retrospective Study from Hradec Králové, Czech Republic. Acta Medica (Hradec Kralove). 2015;58:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Treviño-Gonzalez JL, Maldonado-Chapa F, González-Larios A, Morales-Del Angel JA, Soto-Galindo GA, Zafiro García-Villanueva JM. Deep Neck Infections: Demographic and Clinical Factors Associated with Poor Outcomes. ORL J Otorhinolaryngol Relat Spec. 2022;84:130-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Çetin AÇ, Olgun Y, Özses A, Erdağ TK. A New Trend in the Management of Pediatric Deep Neck Abscess: Achievement of the Medical Treatment Alone. Turk Arch Otorhinolaryngol. 2017;55:57-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Boscolo-Rizzo P, Stellin M, Muzzi E, Mantovani M, Fuson R, Lupato V, Trabalzini F, Da Mosto MC. Deep neck infections: a study of 365 cases highlighting recommendations for management and treatment. Eur Arch Otorhinolaryngol. 2012;269:1241-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 20. | Crespo AN, Chone CT, Fonseca AS, Montenegro MC, Pereira R, Milani JA. Clinical versus computed tomography evaluation in the diagnosis and management of deep neck infection. Sao Paulo Med J. 2004;122:259-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 21. | Prabhu SR, Nirmalkumar ES. Acute Fascial Space Infections of the Neck: 1034 cases in 17 years follow up. Ann Maxillofac Surg. 2019;9:118-123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Gunaratne DA, Tseros EA, Hasan Z, Kudpaje AS, Suruliraj A, Smith MC, Riffat F, Palme CE. Cervical necrotizing fasciitis: Systematic review and analysis of 1235 reported cases from the literature. Head Neck. 2018;40:2094-2102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 23. | Ban MJ, Jung JY, Kim JW, Park KN, Lee SW, Koh YW, Park JH. A clinical prediction score to determine surgical drainage of deep neck infection: A retrospective case-control study. Int J Surg. 2018;52:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Guan X, Liang X, Liang X, Wang F, Qian W, Zhang W. A new classification of descending necrotizing mediastinitis and surgical strategies. Ann Transl Med. 2021;9:356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Hu CY, Lien KH, Chen SL, Chan KC. Risk Factors of Descending Necrotizing Mediastinitis in Deep Neck Abscesses. Medicina (Kaunas). 2022;58:1758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 26. | Endo S, Murayama F, Hasegawa T, Yamamoto S, Yamaguchi T, Sohara Y, Fuse K, Miyata M, Nishino H. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Cardiovasc Surg. 1999;47:14-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 129] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 27. | Weiner KAS, Rieger CC, Wohl DL, Harley EH. Retropharyngeal Abscess With Mediastinal Extension: A Case Series and Review of the Literature. Ear Nose Throat J. 2023;102:580-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/