Published online Oct 16, 2024. doi: 10.12998/wjcc.v12.i29.6302
Revised: June 20, 2024
Accepted: July 16, 2024
Published online: October 16, 2024
Processing time: 150 Days and 2.5 Hours
With 4.9 to 35 instances per 100000 cases, hyperparathyroidism is one of the rarest causes of acute pancreatitis. The major cause of primary hyperparathyroidism is a parathyroid adenoma, which can manifest clinically in various ways.
We discuss the unusual case of a 13-year-old boy with recurrent pancreatitis as the initial presentation of primary hyperparathyroidism. The cause of his recu
This case study stresses the importance of considering uncommon causes for re
Core Tip: Primary hyperparathyroidism (PHPT) should be considered as a potential cause when investigating cases of acute pancreatitis, especially in pediatric patients, even if blood parathyroid hormone levels initially appear normal. For an accurate diagnosis, PHPT may need a comprehensive investigation, including imaging techniques such as neck ultrasonography and scintigraphy. PHPT may sometimes only present as pancreatitis. To prevent recurrent episodes of pancreatitis and the difficulties that go along with it, early detection and treatment of PHPT are essential.
- Citation: Karim MM, Raza H, Parkash O. Recurrent acute pancreatitis as an initial presentation of primary hyperparathyroidism: A case report. World J Clin Cases 2024; 12(29): 6302-6306
- URL: https://www.wjgnet.com/2307-8960/full/v12/i29/6302.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i29.6302
Acute pancreatitis is a condition characterized by inflammation of the pancreas. It is a widespread condition that accounts for a significant portion of admissions to the gastrointestinal department. The worldwide incidence of acute pancreatitis is 4.9 to 35 per 100000 in the United States, which is increasing worldwide[1]. Gallstones and alcohol are responsible for more than half of the cases of acute pancreatitis in adults[2]. This is not the same for children and adolescents. The main culprits for acute pancreatitis in the pediatric population include abdominal trauma accounting for 13%-33% of cases[3]. Other causes include hereditary and infectious etiology.
Rarely, acute pancreatitis can manifest as hypercalcemia caused by primary hyperparathyroidism (PHPT). In 80%-85% of cases, benign parathyroid adenoma is the most frequent cause of PHPT[4]. Clinical presentation varies between individuals. Children and adolescents almost always have an unusual presentation[5]. In 1.5%-13% of those with PHPT they will develop acute pancreatitis. PHPT is a rare condition in children, with a prevalence of 2-5 per 100000 and an estimated incidence of 1 in 200000-300000[6].
We present a young boy with PHPT due to parathyroid adenoma who had multiple episodes of acute pancreatitis. The cause remained a query until the diagnosis was made. After treatment for parathyroid adenoma, no episodes of pancreatitis occurred, and the patient's symptoms resolved.
This case study emphasizes the value of thorough follow-up to reveal the underlying issues that can be resolved.
Generalized abdominal pain and vomiting for 2 days.
According to the patient and his parents, he was in his usual state of health 2 days previously when he developed abdominal pain in the epigastric region, of severe intensity, sudden onset, radiating to the back, and multiple episodes of vomiting associated with decreased appetite and nausea. The patient denied any prior similar episodes.
His past medical history was unremarkable.
Personal and family history was unremarkable, with no family history of hereditary diseases.
On arrival, the patient was stable. On examination, sluggish stomach sounds, slight right upper quadrant, and epigastric discomfort were documented. Other systemic examinations were unremarkable.
Laboratory workup was conducted including liver function tests, complete blood count, serum electrolytes, serum amylase, serum lipase, and lactate dehydrogenase (LDH). Serum amylase and lipase levels were found to be elevated at 361 IU/L and 447 U/L, respectively. Among others, serum calcium (12.5 mg/dL) and serum LDH (265 IU/L) were significant.
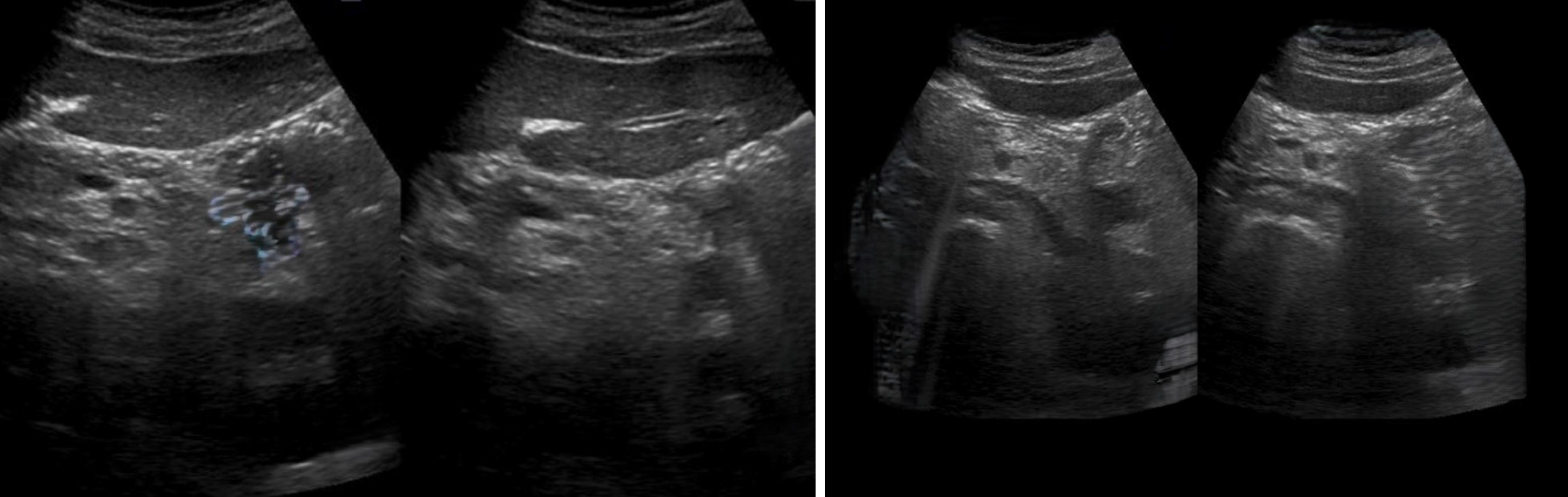
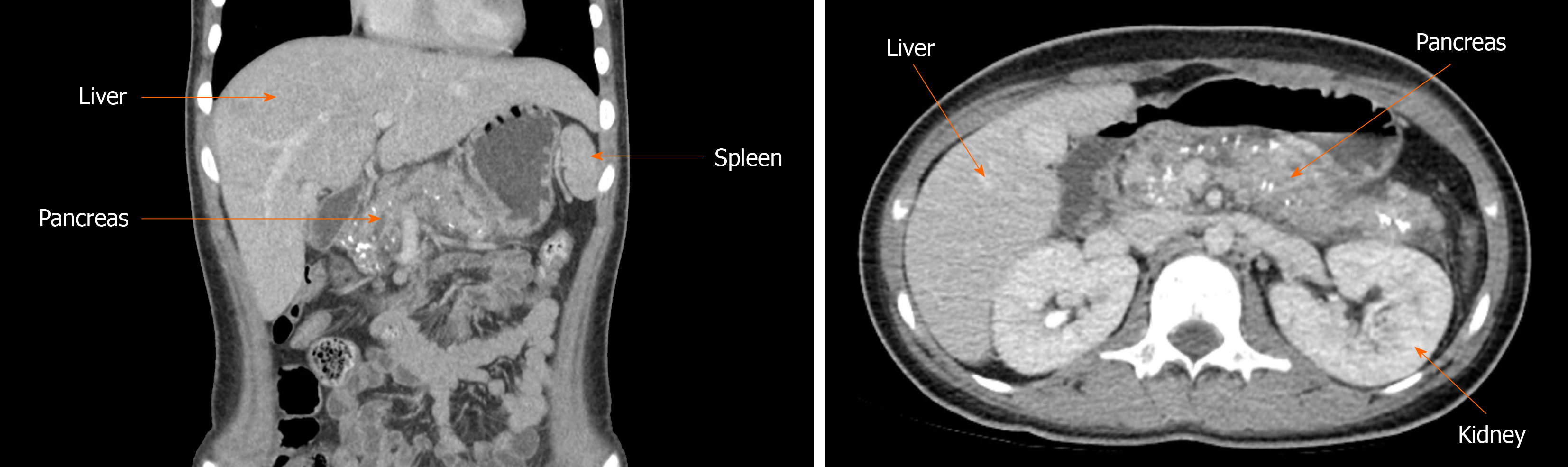
Ultrasound (US) of the abdomen was performed which showed the head of the pancreas with the suggestion of a streak of peripancreatic fluid, mild to moderate ascites, and mild left-sided pleural effusion. US findings were consistent with acute pancreatitis (Figure 1). In 2022, the patient was admitted again with similar complaints, a CT scan showed acute pancreatitis with early chronic changes (Figure 2).
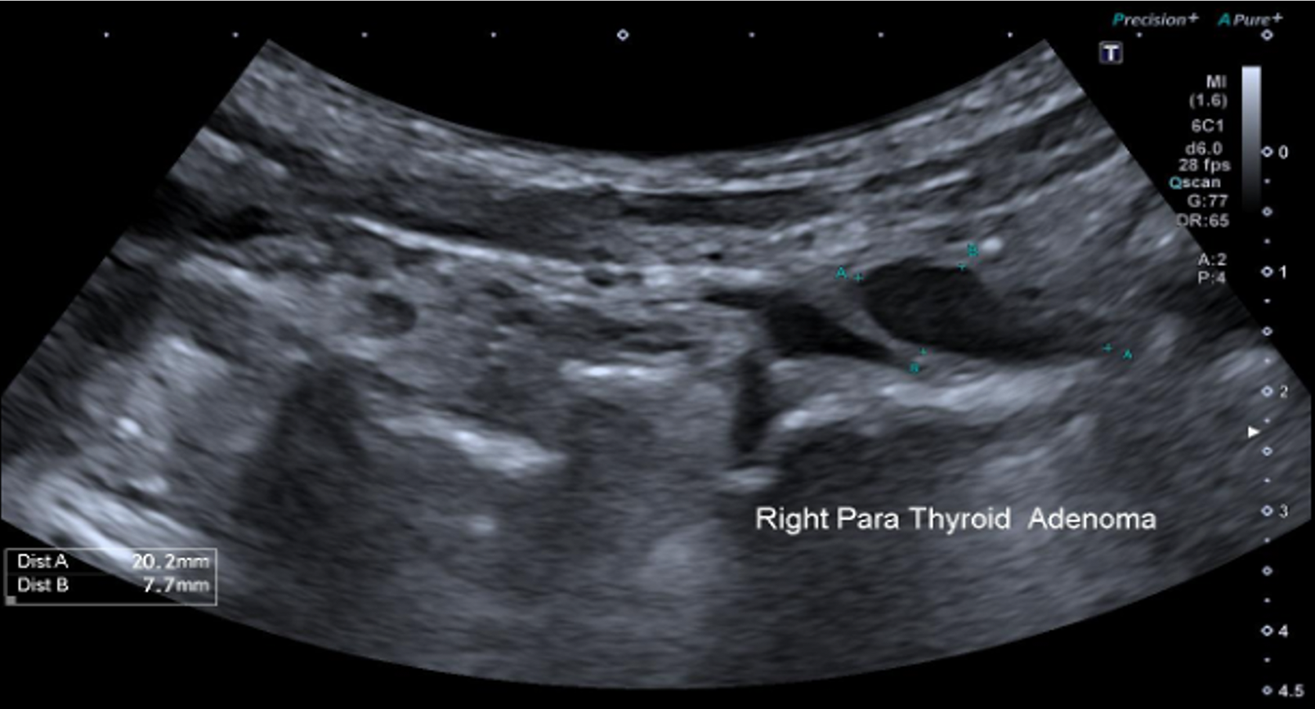
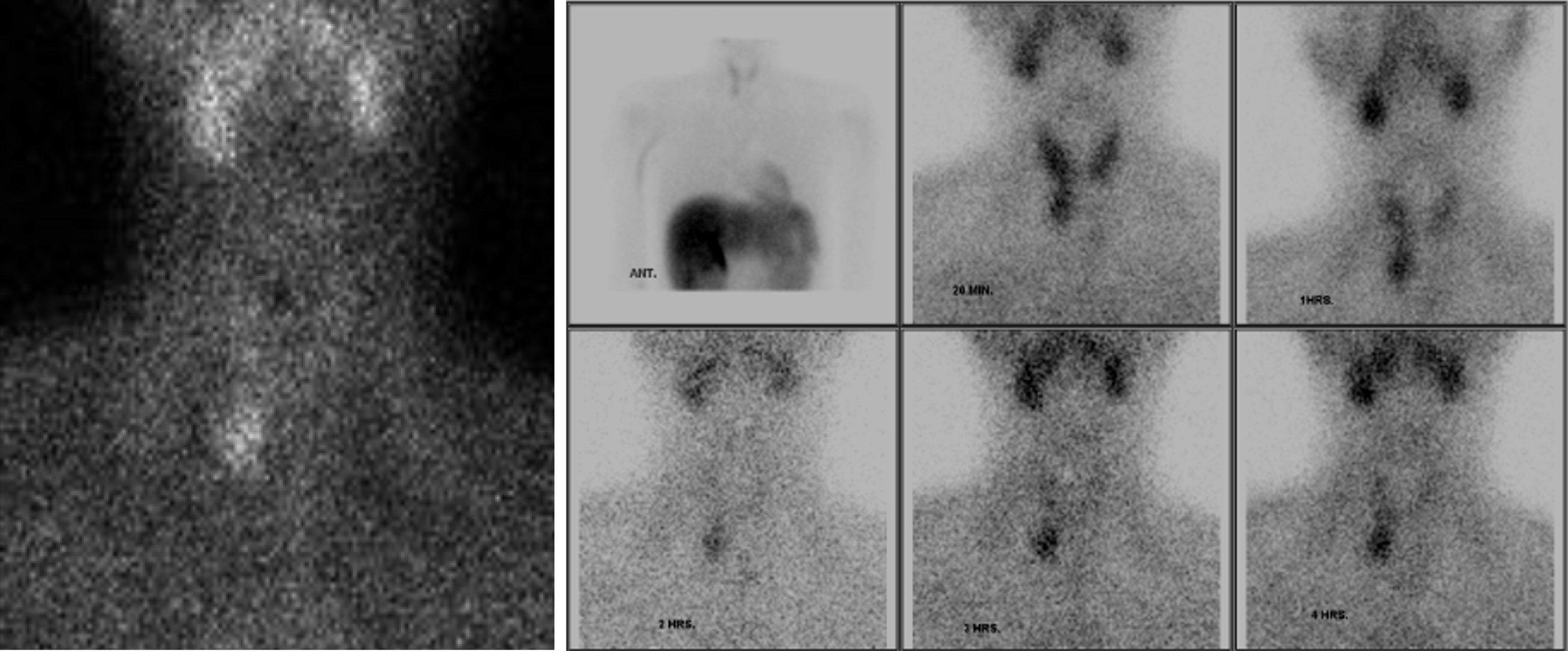
The pediatric endocrinology team advised a neck US (Figure 3), and a scintigraphy scan (Figure 4). The US of the neck showed a parathyroid adenoma at the lower pole of the right thyroid lobe.
Parathyroid adenoma.
Surgical removal of the parathyroid adenoma.
Following resection of the adenoma, serum calcium levels normalized, and the patient’s symptoms resolved.
Acute pancreatitis as a complication of hypercalcemia due to PHPT has been defined in the literature. The mechanism is still unclear, but the theory is that raised serum calcium levels activate trypsinogen to trypsin, causing pancreatic damage and calcium deposits in the pancreatic duct, resulting in obstruction[7].
Lanitis et al[8] reported that the relationship between pancreatitis and PHPT is not incidental but a consequence of hypercalcemia. As early as the late 1950s, Cope et al[9] suggested acute pancreatitis as a sole presentation of PHPT and a clue to the diagnosis of PHPT. A review study in Vellore reported a causal relationship between acute pancreatitis and PHPT. This study also reported that patients with PHPT have a 28-fold higher risk of developing pancreatitis than patients with no evidence of PHPT[10]. A similar survey by Ramachandran et al[11] reported a linear relationship bet
Diagnosing PHPT in children is difficult as it is uncommon in children, resulting in misdiagnosis or a delayed diag
Underdiagnosis and delayed diagnosis of PHTP primarily due to the normal levels of PTH result in an increased risk of developing complications.
After reviewing our experience, engaging in a comprehensive assessment is advisable to determine the underlying cause of undetermined pancreatitis. When encountering hypercalcemia accompanied by serum PTH within normal ranges, it is essential to include PHPT in the list of potential differential diagnoses.
Due to the rarity of PHPT, it poses a diagnostic challenge for physicians. PHPT should be included in the differential diagnoses when evaluating the cause of undefined pancreatitis even with normal PTH levels. Pancreatitis can be a solo presentation, as seen in our case. High clinical suspicion can help diagnose and manage PHPT early to avoid its complications.
| 1. | Vege SS. Etiology of acute pancreatitis - UpToDate. Mar 18, 2024. [cited 3 July 2024]. Available from: https://www.uptodate.com/contents/etiology-of-acute-pancreatitis. |
| 2. | Gapp J, Tariq A, Chandra S. Acute Pancreatitis. 2023 Feb 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. [PubMed] |
| 3. | Uretsky G, Goldschmiedt M, James K. Childhood pancreatitis. Am Fam Physician. 1999;59:2507-2512. [PubMed] |
| 4. | National Organization for Rare Disorders. Primary Hyperparathyroidism. May 17, 2023. [cited 3 July 2024]. Available from: https://rarediseases.org/rare-diseases/primary-hyperparathyroidism/. |
| 5. | Venail F, Nicollas R, Morin D, Mackle T, Garnier JM, Triglia JM, Mondain M. Solitary parathyroid adenoma: a rare cause of primary hyperparathyroidism in children. Laryngoscope. 2007;117:946-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Mancilla EE. Pediatric Hyperparathyroidism: Practice Essentials, Pathophysiology, Etiology. Dec 7, 2022. [cited 3 July 2024]. Available from: https://emedicine.medscape.com/article/921453-overview?icd=login_success_gg_match_norm&isSocialFTC=true#a6. |
| 7. | Garg PK, editor. Acute Pancreatitis - ECAB. New Delhi: Elsevier Health Sciences, 2013. |
| 8. | Lanitis S, Sivakumar S, Zaman N, Westerland O, Al Mufti R, Hadjiminas DJ. Recurrent acute pancreatitis as the first and sole presentation of undiagnosed primary hyperparathyroidism. Ann R Coll Surg Engl. 2010;92:W29-W31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Cope O, Culver PJ, Mixter CGJ, Nardi GL. Pancreatitis, A Diagnostic Clue to Hyperparathyroidsm. Ann Surg. 1957;145:857-863. |
| 10. | Jacob JJ, John M, Thomas N, Chacko A, Cherian R, Selvan B, Nair A, Seshadri M. Does hyperparathyroidism cause pancreatitis? A South Indian experience and a review of published work. ANZ J Surg. 2006;76:740-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Ramachandran R, Nair GC, Babu MJC, Jacob P. Acute pancreatitis and primary hyperparathyroidism. Formos J Surg. 2018;51:219-222. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Mixter CG, Keynes WM, Cope O. Further Experience with Pancreatitis as a Diagnostic Clue to Hyperparathyroidism. N Engl J Med. 1962;266:265-272. [DOI] [Full Text] |
| 13. | Lawson ML, Miller SF, Ellis G, Filler RM, Kooh SW. Primary hyperparathyroidism in a paediatric hospital. QJM. 1996;89:921-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 58] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Mischis-Troussard C, Goudet P, Verges B, Cougard P, Tavernier C, Maillefert JF. Primary hyperparathyroidism with normal serum intact parathyroid hormone levels. QJM. 2000;93:365-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Amin AL, Wang TS, Wade TJ, Yen TW. Normal PTH levels in primary hyperparathyroidism: still the same disease? Ann Surg Oncol. 2011;18:3437-3442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/licenses/by-nc/4.0/