Published online Sep 16, 2024. doi: 10.12998/wjcc.v12.i26.5968
Revised: June 19, 2024
Accepted: July 5, 2024
Published online: September 16, 2024
Processing time: 118 Days and 22.2 Hours
We report a case of uterine artery pseudoaneurysm (UAP) occurrence during hysteroscopic endometrial polypectomy and its treatment via uterine artery embolization (UAE).
A 48-year-old primigravid, primiparous patient was incidentally found to have an endometrial polyp during a health checkup, and underwent a hysteroscopic polypectomy at another hospital. Her cervix was dilated with a Laminken-R® device. After the Laminken-R® was withdrawn, a large amount of genital bleeding was observed. This bleeding persisted after the hysteroscopic polypectomy, and, as hemostasis became impossible, the patient was transferred to our hospital by ambulance. On arrival, transvaginal ultrasonography revealed a 3-cm hypoechoic mass with a swirling internal pulse on the right side of the uterus, and color Doppler ultrasonography showed feeder vessels penetrating the mass. Pelvic contrast-enhanced computed tomography (CT) confirmed the presence of a mass at this site, and vascular proliferation was observed within the uterine cavity. Consequently, UAP was diagnosed, and UAE was performed. The patient’s postoperative course was uneventful, and 6 mo post-UAE, no recurrence of blood flow to the UAP was observed.
When abnormal genital bleeding occurs during hysteroscopic surgery, ultrasonography and contrast-enhanced CT can assist in the detection of early UAPs.
Core Tip: When abnormal uterine bleeding occurs after hysteroscopic surgery, the possibility of uterine artery pseudoaneurysm (UAP) must be considered. Confirmed UAP must be managed promptly and appropriately.
- Citation: Kakinuma K, Kakinuma T, Ueyama K, Okamoto R, Yanagida K, Takeshima N, Ohwada M. Uterine artery pseudoaneurysm caused by hysteroscopic surgery: A case report. World J Clin Cases 2024; 12(26): 5968-5973
- URL: https://www.wjgnet.com/2307-8960/full/v12/i26/5968.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i26.5968
Uterine artery pseudoaneurysm (UAP) is an acquired condition in which the wall of the uterine artery collapses, and the arterial wall layers engulf the blood that has leaked from the vessel[1]. UAPs generally occur after delivery or miscarriage and often cause massive hemorrhage, but cases of its occurrence unrelated to pregnancy, such as during myomectomies, have also been reported. Although UAP is rare, it is a potentially life-threatening condition that can cause massive hemorrhage when it ruptures[2]. We report our experience of uterine artery embolization (UAE) to treat a patient who developed a UAP during hysteroscopic surgery.
A 48-year-old primigravid, primiparous patient (vaginal delivery) was transferred to our clinic for persistent genital bleeding after hysteroscopic polypectomy.
An endometrial polyp was incidentally identified during a health checkup, and a hysteroscopic polypectomy was conducted at another hospital. The cervix was dilated with a 5-mm Laminken-R® device (Ken Medical Company Ltd., Hyogo, Japan). After the Laminken-R® was withdrawn, a large amount of genital bleeding was observed, but transcervical resection was nevertheless performed. A rigid OLYMPUS hystero-resectoscope (OES Pro Resectoscope, Olympus Medical Systems Corporation, Japan) was used with 3% D-sorbitol (UromaticS®, Baxter Ltd., United States) as the perfusion solution. Although the procedure only took 15 min, the genital bleeding persisted even after the hysteroscopic polypectomy. As hemostasis proved impossible, the patient was brought to our hospital by ambulance for further investigation and treatment.
Nothing of note.
Nothing of note.
On examination upon arrival, her vital signs were as follows: Blood pressure, 108/72 mmHg; heart rate, 72 beats/min; and body temperature, 36.8 ºC.
Colposcopy revealed persistent bleeding from the external uterine orifice. Blood test results revealed anemia, with a hemoglobin level of 8.3 g/dL, but all other test results were unremarkable.
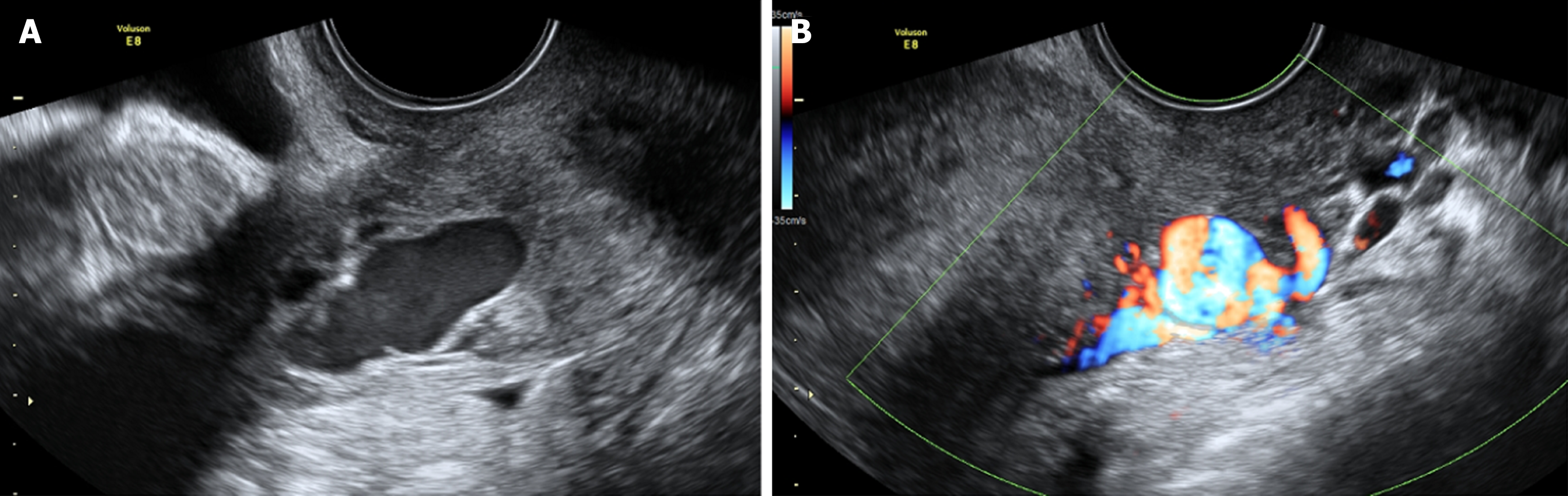
Transvaginal ultrasonography: A 3-cm hypoechoic mass with a swirling internal pulse was apparent in the right wall of the uterus (Figure 1A), and color Doppler revealed abundant turbulent blood flow into the mass (Figure 1B).
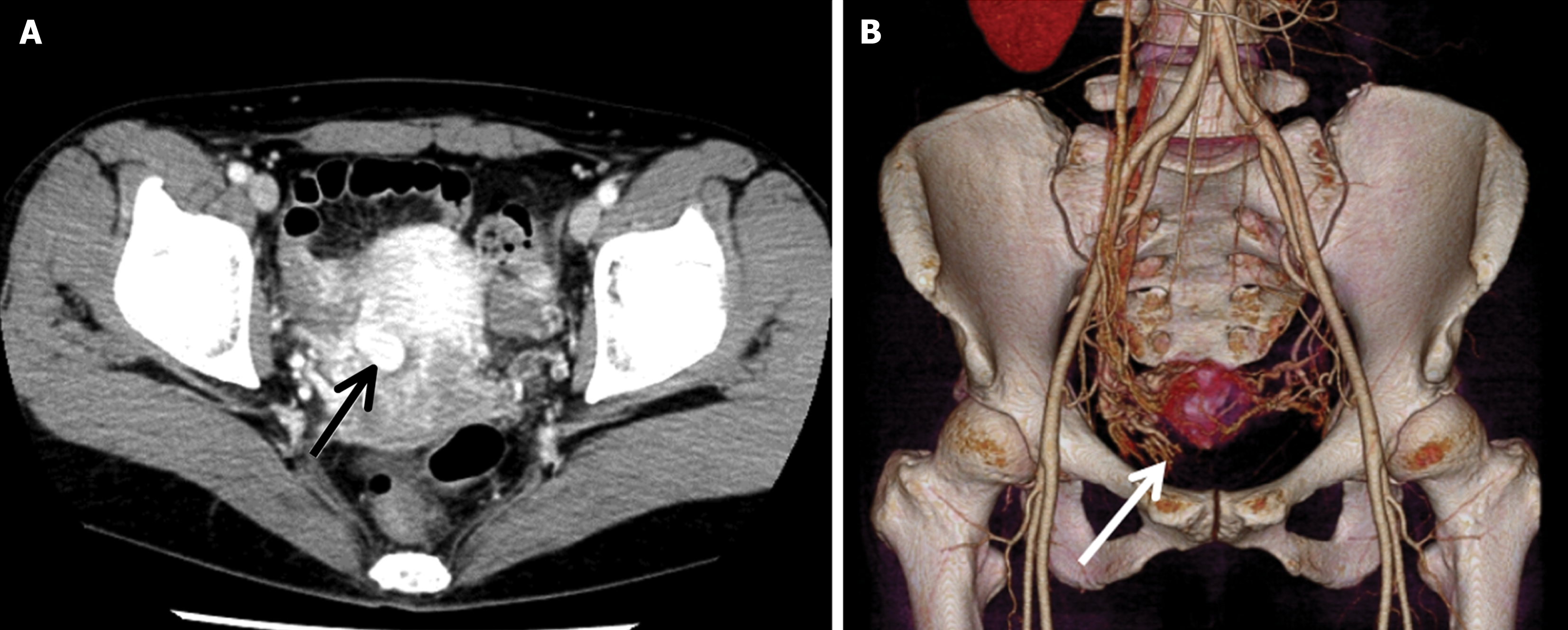
Pelvic contrast-enhanced computed tomography (CT) showed the presence of a contrast-enhanced mass at the site identified on ultrasonography (Figure 2A). Three-dimensional image reconstruction showed that the aneurysm was continuous with the right uterine artery. A UAP in the right uterine artery trunk was diagnosed (Figure 2B).
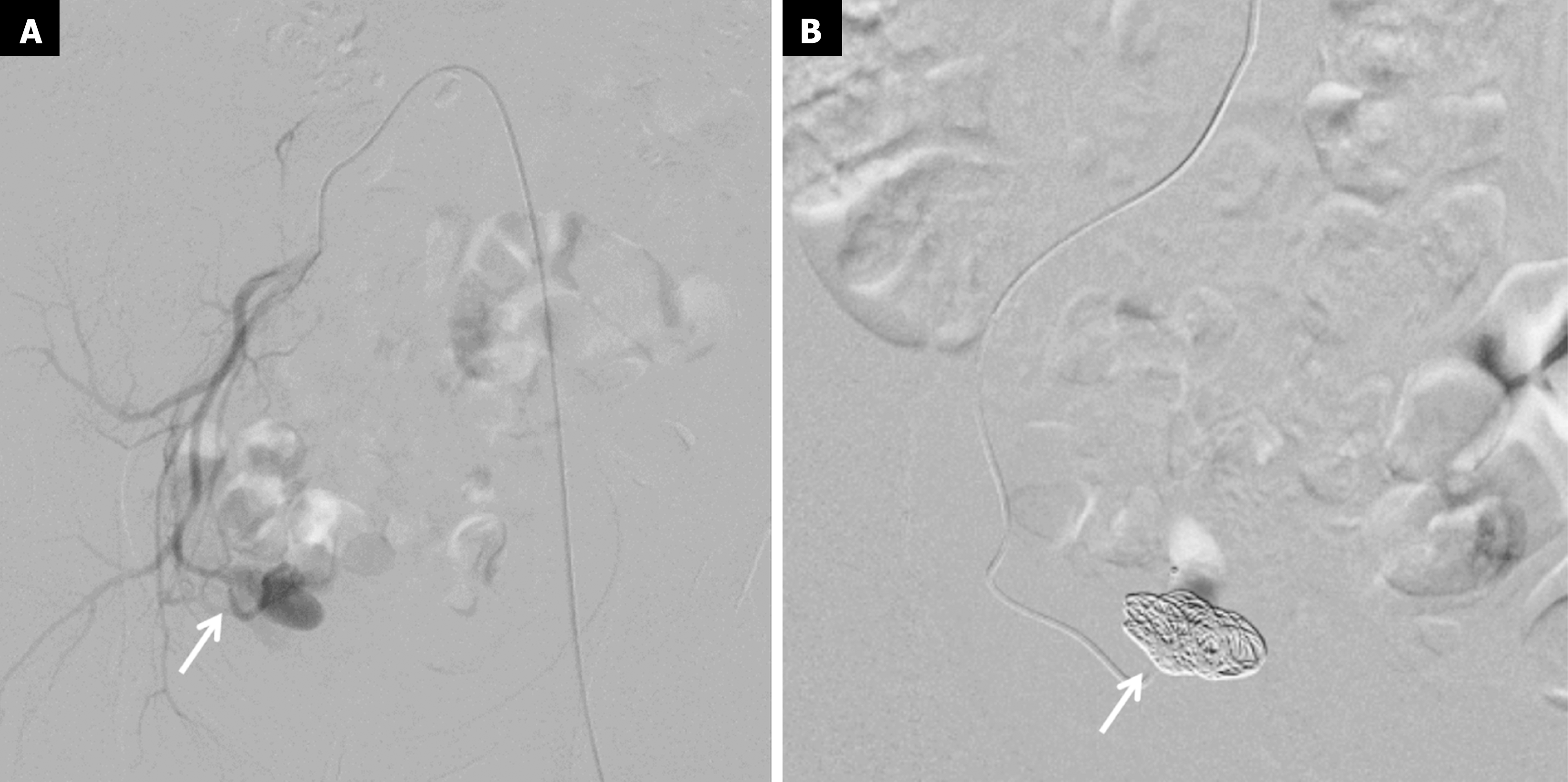
Because of the risk of bleeding, UAE was chosen as the treatment method. Angiography showed the formation of a 3-cm UAP in the descending branch of the right uterine artery (Figure 3A). There was no sign of extravasation. Since the blood flow to the UAP was observed, and this patient did not want to have a baby and wanted to ensure hemostasis, the feeder artery was subjected to coil embolization (Figure 3B). The patient’s post-treatment course was uneventful, and, after color Doppler ultrasonography confirmed that there was no recurrence of blood flow to the uterine pseudoaneurysm, she was discharged on postoperative day 4.
Presently, 6 mo post-UAE, her course has been uneventful, with no recurrence of blood flow to the UAP.
UAP is a condition in which the wall of a uterine blood vessel collapses due to some invasive event, and the resulting leaked blood is engulfed by soft tissue, forming a cavity that is in communication with the vessel. The walls of the cavity are fragile and break down easily, frequently causing massive hemorrhage[1]. UAPs frequently develop during the puerperal period or after a miscarriage and reportedly occur in 0.2–0.3% of all pregnancies[2,3]. The most reported cause unrelated to pregnancy is myomectomy[4]. In rare cases, it is caused by adeno myomectomy, cervical conization, abdominal total hysterectomy, transvaginal simple total hysterectomy, and robot-assisted total hysterectomy[5-9].
Ultrasonography is regarded as a helpful modality in diagnosing UAPs[10]. On transvaginal ultrasonography, a UAP can be visualized as an area of low brightness, and on color Doppler ultrasonography, pulsatile spiral blood flow, known as “swirling blood flow” is evident at the same site. Dynamic CT is another useful imaging modality[11] that enables the visualization of not only UAP as an area of early enhancement continuous with a blood vessel, but also of the responsible vessel, thus enabling timely diagnosis. Whether or not the UAP has ruptured can easily be determined from the presence or absence of extravasation, making this an essential modality to decide on the management and treatment strategy for UAPs.
The treatment method used in this case, UAE, is used in almost all cases of genital bleeding, and it is reportedly effective[12-14]. Regarding the incidence of complications of UAE, those associated with vascular contrast procedures account for approximately 6%–9% of total complications. The most common complication is post-UAE fever, and other symptoms, including pain, endometritis, intrauterine adhesions, uterine necrosis, pelvic infections, and reduced ovarian function, may also occur[15-18]. Although post-UAE fertility is believed to be comparatively good, some studies have reported significant increases in the rates of miscarriage, postpartum hemorrhage, premature birth, and abnormal fetal presentation following UAE, as well as cases of intrauterine fetal growth restriction. Thus, women who become pregnant after UAE require careful perinatal management[1,19].
In cases where the UAP is asymptomatic, there is no consensus on whether UAE should be conducted prophylactically or whether the watch-and-wait strategy should be adopted. Although some asymptomatic UAPs resolve spontaneously, others rupture and cause massive bleeding; currently, it is difficult to predict whether a UAP will rupture. The treatment strategy for an unruptured UAP merits further investigation. At this stage, indications for treatment must be determined according to individual patient factors, such as changes in the size of the UAP and treatment resources available at specific institutions, including the feasibility of emergency UAE when bleeding occurs.
In the present case, a UAP that had not been evident on preoperative imaging was observed after hysteroscopic surgery, suggesting that the surgery may have induced the UAP. Cervical dilation is not always necessary for small-diameter hysteroscopic surgery. However, in our patient, the procedure was conducted with a conventional rigid hysteroscope, and the cervix was therefore dilated preoperatively with a 5-mm Laminken-R® before performing the hysteroscopic polypectomy. The profuse genital bleeding observed after the Laminken-R® was withdrawn suggests that the UAP was caused either by direct injury from the Laminken-R® or due to over-dilation. The perfusion solution used during hysteroscopic surgery increases the intrauterine pressure, and this could also have led to the collapse of the vascular wall. Laminken-R® insertion involves blunt manipulation and must be conducted with caution since it is an invasive device. When inserting the Laminken-R®, the direction of the uterine cavity should be checked, and a uterine probe must be used to measure its length. Furthermore, the Laminken-R® comes in a range of sizes, and observing the cervix before dilation is important for choosing the correct size. In addition, the appropriate flow rate for the perfusion solution used during hysteroscopy may vary between individuals, depending on factors such as the volume of the uterine cavity and the flexibility of the myometrium, and attention must also be paid to this flow rate to avoid an excessive increase in intrauterine pressure.
In the event of abnormal uterine bleeding after hysteroscopic surgery, the possibility of a UAP must be considered; transvaginal ultrasonography and tomography using color Doppler ultrasonography and dynamic CT must be conducted to ensure prompt and appropriate management.
| 1. | Goldberg J, Pereira L, Berghella V. Pregnancy after uterine artery embolization. Obstet Gynecol. 2002;100:869-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Matsubara S, Kuwata T, Usui R, Ohkuchi A. Uterine artery pseudoaneurysm: a master of deception. Arch Gynecol Obstet. 2014;289:469-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Baba Y, Matsubara S, Kuwata T, Ohkuchi A, Usui R, Saruyama M, Nakata M, Suzuki M. Uterine artery pseudoaneurysm: not a rare condition occurring after non-traumatic delivery or non-traumatic abortion. Arch Gynecol Obstet. 2014;290:435-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Takeda A, Kato K, Mori M, Sakai K, Mitsui T, Nakamura H. Late massive uterine hemorrhage caused by ruptured uterine artery pseudoaneurysm after laparoscopic-assisted myomectomy. J Minim Invasive Gynecol. 2008;15:212-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Matsubara S, Usui R, Sato T, Kuwata T, Ohkuchi A, Nakata M. Adenomyomectomy, curettage, and then uterine artery pseudoaneurysm occupying the entire uterine cavity. J Obstet Gynaecol Res. 2013;39:1103-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Moon G, Jeon S, Nam KH, Choi S, Sunwoo J, Ryu A. Pseudoaneurysm of uterine artery causing intra-abdominal and vaginal bleeding after cervical conization. Obstet Gynecol Sci. 2015;58:256-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Lee WK, Roche CJ, Duddalwar VA, Buckley AR, Morris DC. Pseudoaneurysm of the uterine artery after abdominal hysterectomy: radiologic diagnosis and management. Am J Obstet Gynecol. 2001;185:1269-1272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Langer JE, Cope C. Ultrasonographic diagnosis of uterine artery pseudoaneurysm after hysterectomy. J Ultrasound Med. 1999;18:711-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Gerardi MA, Díaz-Montes TP. Late onset hemorrhage caused by ruptured uterine artery pseudoaneurysm after robotic-assisted total hysterectomy. J Robot Surg. 2011;5:295-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Matsubara S. Pseudoaneurysm: a chameleon in obstetrical emergency practice. Arch Gynecol Obstet. 2011;283:669-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Isono W, Tsutsumi R, Wada-Hiraike O, Fujimoto A, Osuga Y, Yano T, Taketani Y. Uterine artery pseudoaneurysm after cesarean section: case report and literature review. J Minim Invasive Gynecol. 2010;17:687-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Wan AY, Shin JH, Yoon HK, Ko GY, Park S, Seong NJ, Yoon CJ. Post-operative hemorrhage after myomectomy: safety and efficacy of transcatheter uterine artery embolization. Korean J Radiol. 2014;15:356-363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Takeda A, Koike W, Imoto S, Nakamura H. Conservative management of uterine artery pseudoaneurysm after laparoscopic-assisted myomectomy and subsequent pregnancy outcome: case series and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2014;182:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Ito N, Natimatsu Y, Tsukada J, Sato A, Hasegawa I, Lin BL. Two cases of postmyomectomy pseudoaneurysm treated by transarterial embolization. Cardiovasc Intervent Radiol. 2013;36:1681-1685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Badawy SZ, Etman A, Singh M, Murphy K, Mayelli T, Philadelphia M. Uterine artery embolization: the role in obstetrics and gynecology. Clin Imaging. 2001;25:288-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 107] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Vegas G, Illescas T, Muñoz M, Pérez-Piñar A. Selective pelvic arterial embolization in the management of obstetric hemorrhage. Eur J Obstet Gynecol Reprod Biol. 2006;127:68-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 17. | Hong TM, Tseng HS, Lee RC, Wang JH, Chang CY. Uterine artery embolization: an effective treatment for intractable obstetric haemorrhage. Clin Radiol. 2004;59:96-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 80] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 18. | Kirby JM, Kachura JR, Rajan DK, Sniderman KW, Simons ME, Windrim RC, Kingdom JC. Arterial embolization for primary postpartum hemorrhage. J Vasc Interv Radiol. 2009;20:1036-1045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 19. | Inoue S, Masuyama H, Hiramatsu Y; Multi-Institutional Study Group of Transarterial Embolization for Massive Obstetric Haemorrhage in Chugoku & Shikoku Area Society of Obstetrics and Gynecology. Efficacy of transarterial embolisation in the management of post-partum haemorrhage and its impact on subsequent pregnancies. Aust N Z J Obstet Gynaecol. 2014;54:541-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/