Published online Sep 6, 2024. doi: 10.12998/wjcc.v12.i25.5798
Revised: May 28, 2024
Accepted: July 1, 2024
Published online: September 6, 2024
Processing time: 84 Days and 16.5 Hours
Hemolymphangioma is a rare, noninvasive benign tumor that originates from vascular and lymphatic malformations. It is usually congenital and can present with varying symptoms depending on its location and size. There are very few reports of hemolymphangiomas within the spinal canal, and giant lesions are exceptionally rare.
In July 2023, a 64-year-old male with a giant intravertebral epidural hemolymphangioma from thoracic 11 to lumbar 2 (T11-L2) was admitted to the Department of Spine Surgery at the People's Hospital of Binzhou City, China. The patient experienced progressive lumbar and left lower limb pain, numbness, weakness in both lower limbs, and difficulty with urination and defecation. Imaging studies revealed a large cystic mass in the spinal canal at T11-L2. Surgical decompression was performed, and the pathology confirmed hemolymphangioma.
Complete resection of hemolymphangiomas has the best prognosis, and final diagnosis relies on pathologic diagnosis. In this case, the mass was removed intact with a pedicle nail rod system, leading to adequate spinal decompression and restoration of spinal stability.
Core Tip: This case report emphasizes the importance of accurate diagnosis using magnetic resonance imaging combined with patient history and pathology. Surgical resection is the most effective treatment for hemolymphangiomas, especially when their growth compresses surrounding tissues. Complete radical resection may be necessary to prevent recurrence. The risk of recurrence is low, and there have been no reports of malignant transformation.
- Citation: Sun SF, Wang XH, Yuan YY, Shao YD. Rare giant intradural epidural hemolymphangioma: A case report. World J Clin Cases 2024; 12(25): 5798-5804
- URL: https://www.wjgnet.com/2307-8960/full/v12/i25/5798.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i25.5798
Hemolymphangioma is a rare, noninvasive benign tumor arising from vascular and lymphatic malformations. Vascular malformations may be congenital or acquired, but is most commonly congenital, with an estimated incidence of 1.2 to 2.8 per 1000 newborns. Previous reports have described hemolymphangiomas in the abdomen[1-4], mediastinum[5], chest[6], oral[7], and cardiac[8]. There are fewer reports of intravertebral hemolymphangiomas in the literature[9], and in particular, giant hemolymphangiomas are extremely rare. We here report a patient with a giant intravertebral epidural hemolymphangioma of thoracic 11 to lumber 2 (T11-L2) who was admitted to the Department of Spine Surgery of the People's Hospital of Binzhou City of the First Medical University of Shandong Province, China in July 2023.
A 64-year-old male presented with low back pain accompanied by pain and numbness in the left lower extremity progressively worsening for more than 10 days.
Symptoms appeared more than 10 days before the onset of the disease, with unexplained lumbar pain and pain in the left lower limb, which gradually worsened, and there was numbness and weakness in both lower limbs, defecation and urination disorders, and difficulty in getting out of bed and walking.
The patient had a history of bilateral lower limb fracture surgery, with residual bilateral foot inversion deformity and calf muscle atrophy, and he usually traveled with the help of a tricycle and walked slowly.
The patient had no family history of tumors.
The patient was found to have physiological curvature of the lumbar spine, left-sided percussion pain next to the spinous processes of the upper lumbar vertebrae, and radiating pain in the left lower limb. The patient also experienced decreased sensation in the saddle area, left buttock, lateral thigh, lateral calf, bilateral calf muscle atrophy, bilateral foot inversion deformity, and muscle strength of the lower limb on both sides of the body of grade III.
Routine blood tests, liver and kidney function, and coagulation series did not show any obvious abnormalities.
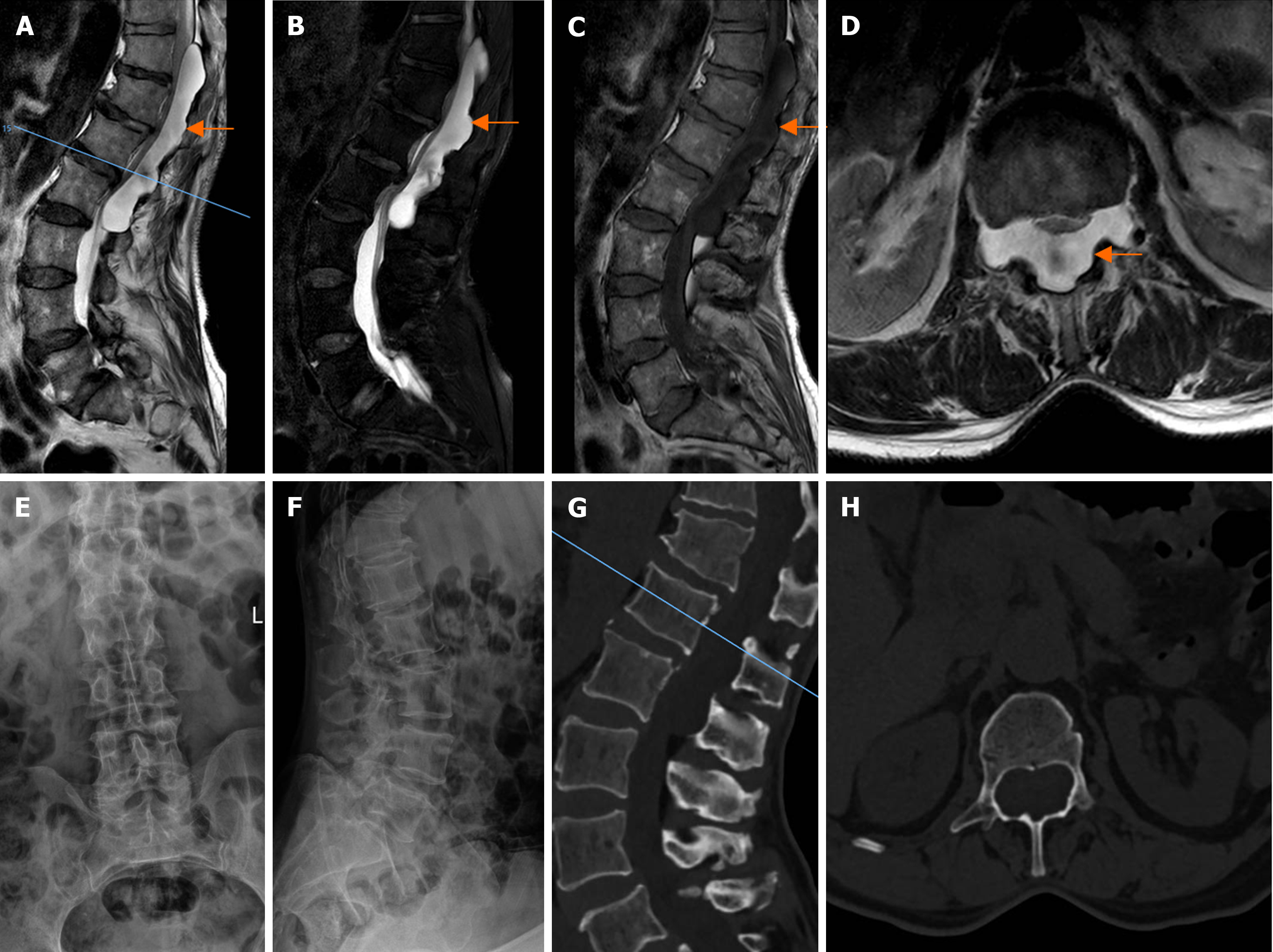
Magnetic resonance imaging (MRI) showed degenerative changes in the thoracic and lumbar spine, and a huge cystic extramedullary and extradural lesion in the spinal canal at the level of T11-L2, which showed low signal on T1WI, high signal on T2WI, and a high signal in the sequence of compression lipids (Figure 1A-D). Severe compression of the spinal cord, which was tightly adhered to the posterior wall of the vertebral body was also observed, the cyst was clearly demarcated from the dura, and it was considered that a cystic neuron sheath tumor was highly possible. Enhanced scanning was performed for further observation. Computed tomography (CT) of the lumbar spine showed a huge extradural cystic lesion in the spinal canal at the level of T11-L2, with compensatory enlargement of the spinal canal, thinning of the vertebral plate, and slenderness of the pedicle (Figure 1G and H). Frontal and lateral X-rays of the lumbar spine showed lumbar degeneration suggestive of T12 vertebral instability (Figure 1E and F).
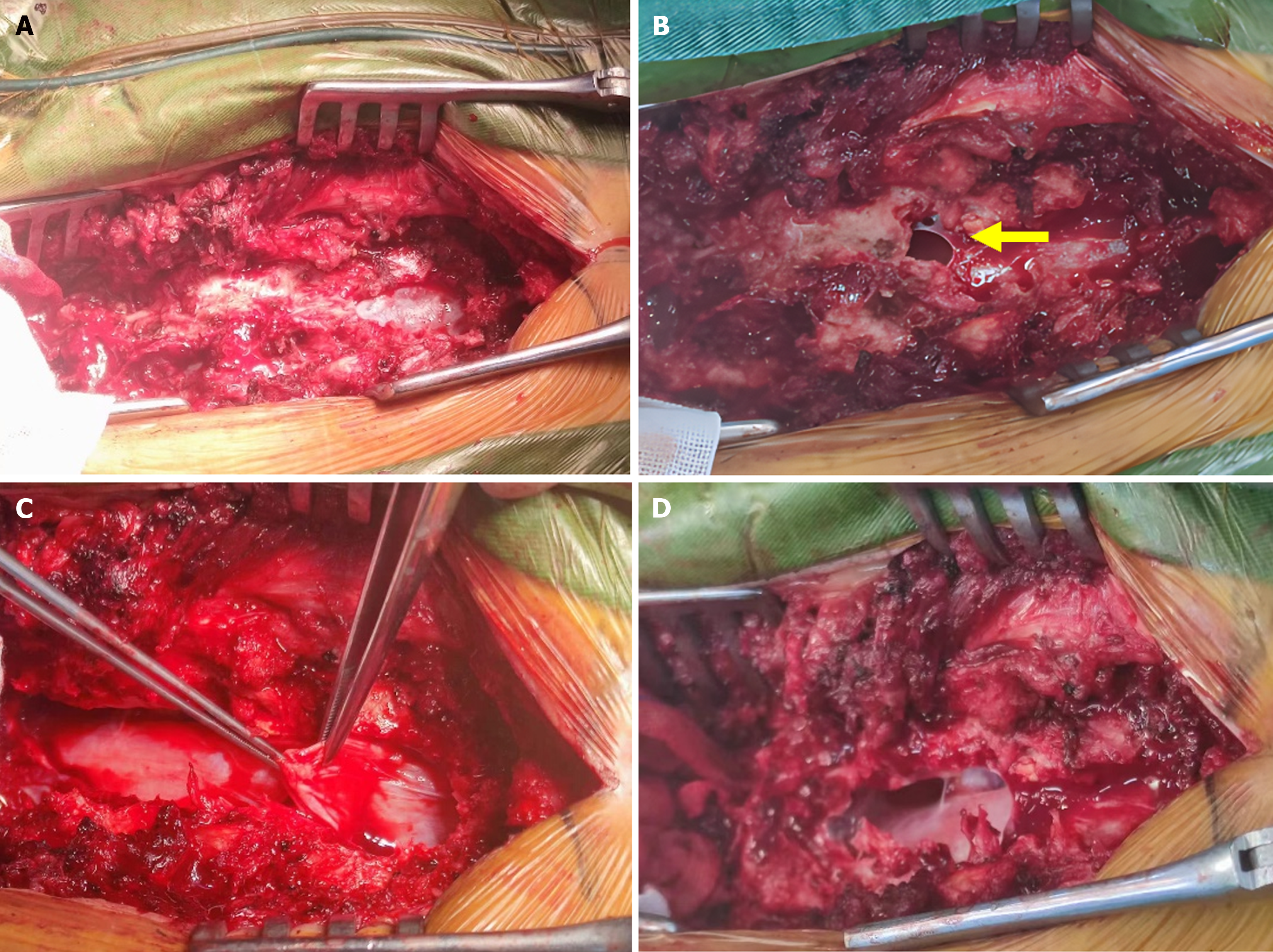
Combined with the patient’s medical history and imaging examinations, the initial diagnosis was an intradural mass in the thoracolumbar spinal canal. Following a preoperative examination to check for contraindications to surgery, resection of the thoracolumbar intravertebral epidural mass and internal fixation with a transpedicular root nail was performed on July 10, 2023 under general anesthesia. During the operation, a posterior median incision was made, and the paraspinal muscles were peeled off to reveal the T11, T12, L1, and L2 spinous processes, vertebral plates, articular synovial joints, and the sphenoid process, part of the vertebral plate, and articular synovial joints were bitten using bone biting forceps, and the caudal and caudal ends of the mass and the sides of the mass were fully exposed (Figure 2A). The mass was observed to be cystic, reddish-brown in color, with a slim ependymal membrane, an irregular morphology, partial adhesion with the dura, and a bright fluid flow in the internal part of the mass (Figure 2B), which was carefully peeled away, and then removed by complete peeling (Figure 2C and D). The mass was carefully and completely excised, and then sent to pathology. One 5.5 mm × 40 mm universal pedicle nail was inserted into each of the T11 and L2 pedicles under direct visualization according to anatomical landmarks, and the tail of the nail was connected to a pair of pre-curved connecting rods for locking and fixation.
According the histopathologic examination, the patient was diagnosed with an intradural epidural hemolymphangioma.
Postoperatively, the patient was given continuous cardiac monitoring within 24 hours, cefuroxime sodium was applied to prevent infection within 48 hours, analgesic, hemostatic, and nutritive neurologic medication was applied, regular dressing changes were made to observe the condition of the incision, and appropriate functional exercises were instructed. The patient recovered well and was discharged on postoperative day 14.
The operation went smoothly, and the results were satisfactory at 8-month follow-up. The patient’s activity level before disease onset was restored.
Hemolymphangiomas are congenital malformations of the vascular system that can be divided into primary and secondary lymphatic tumors. Primary tumors are congenital malformations of the lymphatic vascular system that may develop as a result of embryonic dysplasia of the veno-lymphatic connection between the vascular tissue and the somatic circulation. In contrast, secondary tumors may result from poor lymphatic drainage and lymphatic injury due to surgery or trauma[10].
Clinically, the development of hemolymphangiomas may vary from slow-growing cysts over many years to rapidly enlarging tumors with no invasive capacity. Hemolymphangiomas are rare in clinical practice, probably due to a low incidence and lack of clinical manifestations. In this case, the patient's first symptom was low back pain and left lower extremity pain, which gradually worsened, and there was a cauda equina nerve damage syndrome, including numbness and weakness of both lower extremities, and dysuria, which was probably due to the huge tumor in the vertebral canal. On CT, the periphery of the lesion was markedly thinner in the vertebral arch root and the vertebral plate bone, the cyst encroached on the intervertebral foramen course with the dumbbell sign, and significant encroachment into the surrounding tissues. Hemolymphangiomas mainly present as cystic or spongy lesions. Imaging studies, including ultrasound, CT, and MRI, are important for confirming the diagnosis, determining the nature of the tumor, observing its extension and relationship to the surrounding tissues, and assisting in the selection of surgical strategy and subsequent treatment[11]. The definitive diagnosis of the tumor in this case was based on histological evidence (Figure 3). Histologically, hemolymphangiomas are composed of dense fibrous tissue that develops in bands between numerous vascular spaces, invades subcutaneous fat and involves blood vessels or lymphatic vessels[12]. According to the 2018 classification of the International Society for the Study of Vascular Anomalies, vascular anomalies are divided into two categories: Vascular tumors and vascular malformations, which are distinguished by the presence of abnormal proliferation of vascular endothelial cells in vascular tumors but not in vascular malformations, a classification perspective that is widely accepted. Vascular malformations have normal endothelial cells and are structural developmental abnormalities of the vasculature manifested by abnormal dilation, enlargement, tortuosity, and communication of the vasculature. Based on the type of vasculature involved, vascular malformations are classified into four groups: Simple vascular malformations, combined vascular malformations, malformations of medium and large vessels with a name or vascular malformations with an anatomical name, and malformations of the vasculature in combination with other lesions. Combined vascular malformations are defined as two or more malformations occurring in the same lesion[13]. The microscopic pathology in this study showed approximately 70% lymphovascular tissue and 30% vascular tissue (Figure 3). Based on the International Society for the Study of Vascular Anomalies (ISSVA) rules of terminology, it appears that the lesions in this study should be categorized as "combined vascular malformations". Unfortunately, the pathology department did not perform further immunohistochemical tests.
The incidence of hemolymphangiomas is 1.2 to 2.8/1000 newborns[14], and both sexes are affected equally. In this study, a review of the literature up to March 10, 2024 was conducted using the PubMed database. A search strategy was used to identify all possible studies involving the use of the term "hemolymphangioma". A total of 116 previous studies on this type of tumor were identified, with a total of 23 relevant publications in the last 5 years, and only 1 report on intradural epidural hemolymphangioma[9]. To the best of our knowledge, this is the first report of such a large intradural epidural lymphangioma of the spinal canal. In our case, the tumor presented as a huge cystic lesion in the spinal canal. The author is not a professional vascular surgeon and is limited by the scope of the author's disciplinary specialties to do a more in-depth study on vascular anomalies.
Usually, en bloc resection provides the best outcome with a low recurrence rate[15]; however, careful follow-up is required. Furthermore, recurrence rates vary due to complexity, anatomic location, and adequacy of resection. According to the literature, the recurrence rate of lesions undergoing complete resection is 10%-27%, while the recurrence rate of lesions undergoing partial resection may be as high as 50%-100%[11]. Non-surgical treatments including cryotherapy, laser therapy, radiation therapy and local sclerotherapy injections are less effective than surgery[3,5,16].
In this case study, the posterior wall of the spinal canal was resected and the mass was completely removed, which resulted in adequate decompression of the spinal canal, and at the same time, the pedicle nail rod system was performed for fixation to reestablish stability of the spinal column. Considering that some of the pedicles were slim, which made it difficult to place the nails, the nails were placed under direct visualization after resecting the posterior wall of the spinal canal, to ensure the accuracy of nail placement. Postoperative review of CT and X-ray images showed that the pedicle nail was well positioned, firmly fixed (Figure 4), and could be moved at an early stage. Good clinical results were achieved, and no recurrence was seen at the 8-month follow-up.
The incidence of spinal hemolymphangiomas is low and clinical diagnosis remains challenging. Pathological diagnosis of vascular anomalies according to the ISSVA classification can be very good to improve the consistency with the clinical specialties in maintaining the classification and diagnosis of the disease, although at this stage the different systems (such as the central nervous system, bone and soft tissues, gastrointestinal system, pediatrics, dermatopathology, etc.) have not yet reached a complete unification of diagnostic names of this group of diseases, but with the increase in awareness of this phenomenon, this phenomenon will be further improved. In this article, we report a large hemolymphangioma of the thoracolumbar spinal canal, In our opinion, MRI combined with history and pathology is needed to make an accurate diagnosis of hemolymphangioma in the spinal canal and epidural space, and surgical resection seems to be the most effective treatment, especially when the tumor grows and puts pressure on the surrounding tissues. To prevent recurrence, complete radical resection may be necessary. All cases in the literature had good clinical outcomes, the risk of recurrence appears to be low, and no cases of malignant transformation have been reported to date. This case report helps to raise clinicians' awareness of the importance of MRI, history, and pathology in the differential diagnosis of vascular anomalies.
| 1. | Chen Q, Xia J. A giant hemolymphangioma of the pancreas: A case report and literature review. Medicine (Baltimore). 2018;97:e12599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Lim HJ, Shin KS, Lee JE, You SK, Kim KH. Rare Case of Large Hemolymphangioma in the Small Bowel Mesentery: A Case Report. J Korean Soc Radiol. 2023;84:504-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 3. | Li X, Zhang Y, Sun H, Shao Q, Zhang S, Li F, Jiao Z. Hemolymphangioma of the transverse mesocolon: a case report and literature review. Transl Cancer Res. 2021;10:3849-3855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 4. | Li Y, Ta L, Xu Y, Liu J. Giant Hepatic Hemolymphangioma With Peritoneal Effusion in Children: A Case Report and Literature Review. Front Pediatr. 2022;10:817521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 5. | Ying Q, Cui S, Zhou K, Chen Y, Wei P, Ye Q. Hemolymphangioma invasion of R scapula and mediastinum: a rare case report. Pediatr Hematol Oncol. 2022;39:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Song S, Chang D, Li H, Li B, Xu K, Liu C, Cui Y. Rare cystic lymphangioma in the chest wall of an adult patient: A case report and comprehensive review of the literature. Thorac Cancer. 2020;11:3388-3390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 7. | Jain S, Dhingra S, Tandon S, Lamba AK, Faraz F. Oral Hemangiolymphangioma Presenting As Gingival Enlargement: A Rare Case With Literature Review. Cureus. 2023;15:e46674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Chen B, Fan T, Cao Y, Hu L, Yu G. Case report: obstruction in the right ventricular outflow tract due to hemolymphangioma. Front Cardiovasc Med. 2023;10:1142970. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Pan X, Dong Y, Yuan T, Yan Y, Tong D. Two cases of hemolymphangioma in the thoracic spinal canal and spinal epidural space on MRI: The first report in the literature. Medicine (Baltimore). 2017;96:e9524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Liu L, Xiao Y, Yue X, Wang Q. Extremely rare pediatric primary scrotum tumor: spermatic cord hemolymphangioma for a case report and literature review. World J Surg Oncol. 2023;21:226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Wang H, Cao J, Huang H, Yang D, Wu Z, Luo Y, Ling W. Contrast-enhanced ultrasound-based Bosniak classification for evaluating of a cystic renal mass: a rare case description of renal hemolymphangioma. Quant Imaging Med Surg. 2023;13:1221-1226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 12. | Xu J, Zhang C, Tang C. A case of jejunal hemolymphangioma. Dig Liver Dis. 2023;55:291-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Leyman B, Govaerts D, Dormaar JT, Meeus J, Bila M, Coropciuc R, Willaert R, Politis C. A 16-year retrospective study of vascular anomalies in the head and neck region. Head Face Med. 2023;19:32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 14. | Li Y, Pang X, Yang H, Gao C, Peng B. Hemolymphangioma of the waist: A case report and review of the literature. Oncol Lett. 2015;9:2629-2632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Pandey S, Fan M, Chang D, Zhu J, Zhu Y, Li Z. Hemolymphangioma of Greater Omentum: A Rare Case Report. Medicine (Baltimore). 2016;95:e3508. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Azevedo ABD, Satake HH, Faustino ISP, Curioso PAB, Almeida OPD, Silva ARS, Lopes MA. Hemolymphangioma: A Case Report. Oral Surg, Oral Med, Oral Pathol and Oral Radiol. 2020;130: e173. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/