Published online Aug 26, 2024. doi: 10.12998/wjcc.v12.i24.5476
Revised: June 11, 2024
Accepted: June 26, 2024
Published online: August 26, 2024
Processing time: 125 Days and 1.3 Hours
Constipation is a common gastrointestinal disorder characterized by infrequent bowel movements and difficulty in passing stools. It can significantly affect an individual's quality of life and overall well-being. Understanding the causes of constipation is important for its effective management and treatment. In this paper, we have reviewed the primary causes of constipation or functional con
Core Tip: The etiology of constipation is complex, involving a series of primary and secondary causes. Some of the primary factors reviewed in this paper include decreased interstitial cells of Cajal, altered colonic motility, enteric nervous system dysfunction, intestinal flora disturbances, and psychological influences. Clarifying the etiology of constipation can sig
- Citation: Zeng XL, Zhu LJ, Yang XD. Exploration of the complex origins of primary constipation. World J Clin Cases 2024; 12(24): 5476-5482
- URL: https://www.wjgnet.com/2307-8960/full/v12/i24/5476.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i24.5476
Constipation is a clinical condition with a high incidence rate. It is often difficult to manage and can induce cardio
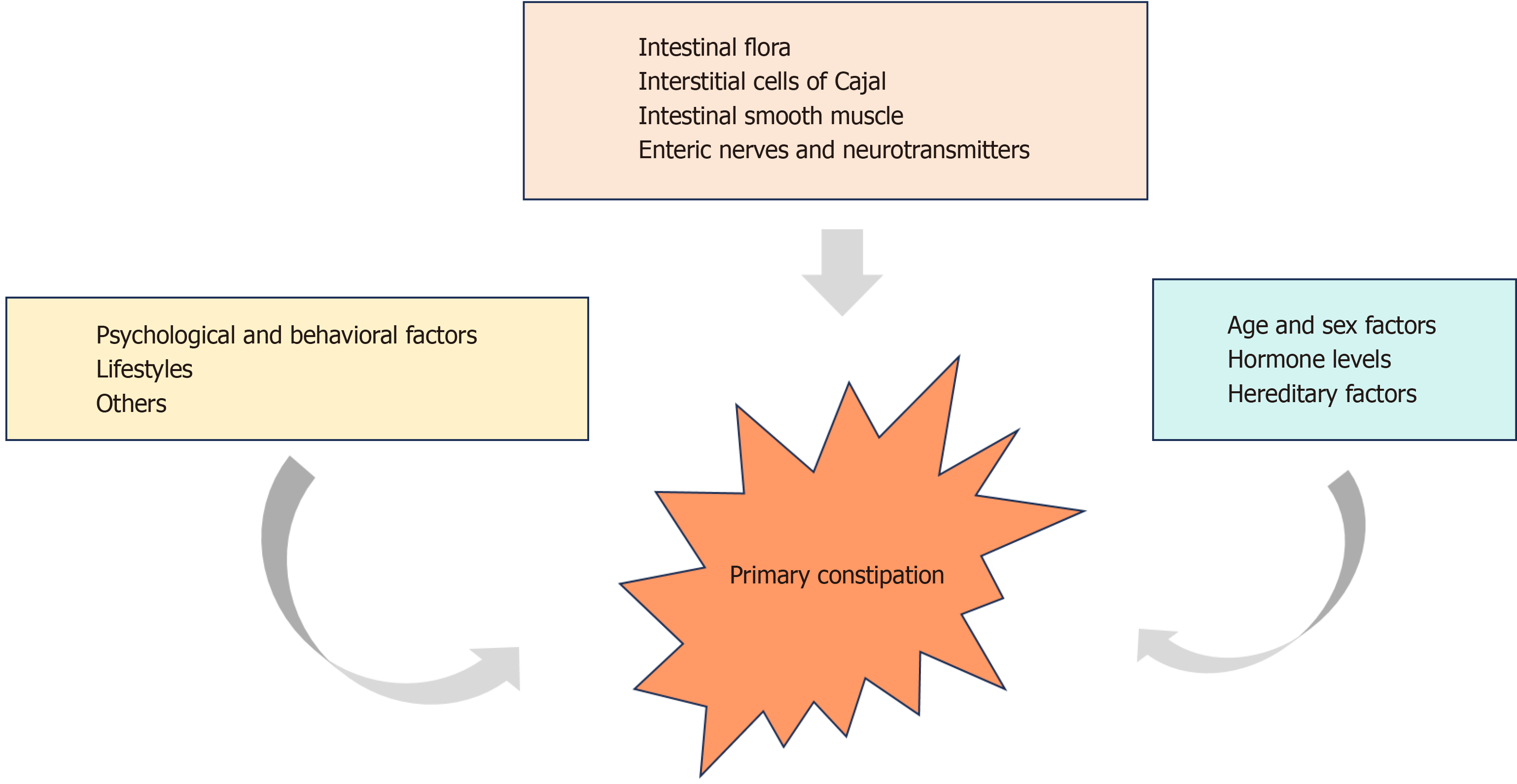
The causes of primary constipation include factors such as interstitial cells of Cajal (ICCs), enteric nerves and neurotransmitters, intestinal flora, intestinal smooth muscle, age, sex, hormone levels, genetic factors, psychological and behavioral factors, and lifestyle factors (Figure 1; Table 1).
| Classification | Etiology | |
| Primary constipation | Intestinal flora | |
| Interstitial cells of Cajal | ||
| Intestinal smooth muscle | ||
| Enteric nerves and neurotransmitters | ||
| Age and sex factors | ||
| Hormone levels | ||
| Hereditary factors | ||
| Psychological and behavioral factors | ||
| Lifestyles | ||
| Others | ||
| Secondary constipation | Secondary conditions | Mechanical obstruction |
| Metabolic disorders | ||
| Neuropathy | ||
| Anorectal disorders | ||
| Others | ||
| Medications | Anticholinergics | |
| Antipsychotics | ||
| Analgesics | ||
| 5-HT receptor antagonists | ||
| Others | ||
ICCs are polymorphic cells located in the smooth muscles of the gastrointestinal tract. They play a crucial role in distributing and regulating the basic electrical activity of the gastrointestinal tract, mediating neural signals, and main
Neuromodulation of the gastrointestinal tract is extraordinarily complex and is subject to regulation by the intrinsic enteric nervous system, central nervous system, and visceral nervous system. ENS is a highly autonomous network composed of neurons, nerve fibers, and supporting cells within the digestive tract[19]. Numerous studies have confirmed abnormalities in the ENS of patients with slow-transit constipation (STC), including decreased neurons and glial cells, ultrastructural changes, and altered neurotransmitters. Furthermore, an enteric neuropathic disorder has been proposed as the essence of STC[20-23]. In the ENS, the excitatory neurotransmitters received by ICCs include neurokinin 1, NK3, acetylcholine, substance P, and 5-hydroxytryptamine, which promote the contraction of the intestinal wall and accelerate intestinal motility. Moreover, inhibitory neurotransmitters, such as nitric oxide, nitric oxide synthase, and vasoactive intestinal peptide, relax the intestinal wall[24-27].
Intestinal flora affects digestive tract development, participates in the formation of the immune system, and maintains digestive tract homeostasis. Attaluri et al's findings have demonstrated that the prevalence of methanogenic flora was higher (P < 0.05) in the STC group (75%) than in the normal transit constipation (NTC) group (44%) or the control group (28%) (P < 0.05)[28]. The NTC group also produced more methane than the control group (P < 0.05), and the baseline, peak, and area under the curve of the methane response were moderately correlated with colonic transit (P < 0.05)[28]. Ohkusa et al[29] found that patients with IBS-C had reduced Actinobacteria counts in the fecal samples and increased Bacteroides levels in the mucosal samples when compared with healthy subjects. Moreover, treatment with synbiotics, probiotics, prebiotics, antibiotics, and fecal microbiota transplants improved the clinical symptoms in patients with constipation[29]. Gastrointestinal microorganisms, especially their populations, play a crucial role in maintaining the structural integrity of the gastrointestinal mucosal barrier, immune regulation, nutrient metabolism, and resistance to pathogens, mainly by increasing the expression of tight junction proteins (i.e., ZO-1 and occludin), and their dysregulation is associated with FC and IBS-C[30].
The brain-gut axis is a bidirectional pathway linking cognitive and emotional centers to the neuroendocrine, ENS, and immune systems. On one hand, stimuli and intrinsic information connect to advanced nerve centers through the enteric nerve chain to affect gastrointestinal sensation, motility, and secretion. However, gastrointestinal functions can consecutively affect pain, emotions, and behavior in the central nervous system. Thus, psychophysiological abnormalities are the causal factors for gastrointestinal disorders. In Dykes et al’s study comprising 28 patients with constipation, 17 (61%) had a current psychiatric disorder and 18 (64%) had a history of psychiatric illness[31]. FC has also been associated with several behavioral factors. For example, Saps et al[32] studied 1334 children with functional gastrointestinal dis
Lesions of the intestinal smooth muscle can trigger altered colonic motility. Sun et al[33] found that the intestinal smooth muscle of STC rats was thinned, with intercellularly separated and disorganized atrophied cytosol. Zhong et al[34] found that drugs can improve constipation by promoting the assembly of actin filaments into tight bundles and stress fibers, thereby enhancing the contractility of intestinal smooth muscle cells. In addition, many studies[35,36] have pointed out that the occurrence of constipation is related to the significant thinning of intestinal smooth muscle and the decrease of intestinal contractility.
According to an epidemiological investigation, the ratio of female to male patients with constipation was 2.2:1, with the chances of constipation increasing with age, as has been evidenced in individuals aged > 65 years due to decreased intestinal peristaltic function[37]. Another study reported an overall prevalence of FC of 26.8%, which was significantly higher in women than in men (P = 0.019)[4]; this difference may be attributed to the fact that women are at a higher risk of injury to the pelvic floor muscles and nerves required for defecation[4].
Chan et al's survey of first-degree relatives and spouses of adult patients with chronic constipation meeting the Rome II criteria revealed that the prevalence of constipation among relatives of patients with constipation was 16.4%[38], whereas that among the relatives of patients without constipation was 9.1%, suggesting that family members of patients with constipation are at a higher risk of developing constipation.
It is widely accepted that diet is closely associated with constipation[39,40]. For instance, in Jung et al’s study[41], for patients with FC, brown rice-based and wheat-based diets led to improved bowel functions as a result of reduced bowel transit time and increased bowel movements when compared with white rice-based diets. Furthermore, appropriate exercise has been suggested to relieve constipation symptoms[42], although some scholars disagree[43]. Owing to the methodological shortcomings, the actual effect of exercise on constipation cannot be definitively determined, warranting further prospective studies in this direction.
Ulusoy et al[44] compared 91 children with constipation and 100 healthy controls and found that the serum gastric motility levels were significantly lower in children with constipation than in healthy controls (P = 0.008), suggesting re
First-line therapies for the treatment of constipation comprise discussing the appropriate and customized diet, exercise, and bowel-management techniques relevant to the patient’s case. Current recommendations suggest that women should consume 20-28 g of fiber and men should consume 30-38 g of fiber in their diets daily, and physical activity should be encouraged in able-bodied patients[48]. Other measures, such as establishing a regular defecation routine and proper toileting habits, are also recommended[49]. If first-line therapies are unsuccessful, pharmacological therapies, such as the use of calcium polycarbophil, psyllium, polyethylene glycol, bisacodyl, and others, should be considered as the next therapeutic option. However, these medications are associated with side effects and may not be always effective[50]. Novel approaches combining several measures need to be explored in larger clinical trials to strategize ways to better manage the disease.
Constipation significantly affects the physical and mental health of individuals. The etiology of constipation is complex, involving a series of primary and secondary causes. Some of the primary factors reviewed in this paper include decreased ICC, altered colonic motility, ENS dysfunction, intestinal flora disturbances, and psychological influences. Clarifying the etiology of constipation can significantly facilitate the management of this disease through an interdisciplinary approach, incorporating dietary modifications, lifestyle changes, pharmacotherapy, and psychological interventions.
| 1. | Sumida K, Molnar MZ, Potukuchi PK, Thomas F, Lu JL, Yamagata K, Kalantar-Zadeh K, Kovesdy CP. Constipation and risk of death and cardiovascular events. Atherosclerosis. 2019;281:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 198] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 2. | Tashiro N, Budhathoki S, Ohnaka K, Toyomura K, Kono S, Ueki T, Tanaka M, Kakeji Y, Maehara Y, Okamura T, Ikejiri K, Futami K, Maekawa T, Yasunami Y, Takenaka K, Ichimiya H, Terasaka R. Constipation and colorectal cancer risk: the Fukuoka Colorectal Cancer Study. Asian Pac J Cancer Prev. 2011;12:2025-2030. [PubMed] |
| 3. | Suares NC, Ford AC. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol. 2011;106:1582-91; quiz 1581, 1592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 674] [Cited by in RCA: 622] [Article Influence: 41.5] [Reference Citation Analysis (0)] |
| 4. | McCrea GL, Miaskowski C, Stotts NA, Macera L, Varma MG. A review of the literature on gender and age differences in the prevalence and characteristics of constipation in North America. J Pain Symptom Manage. 2009;37:737-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 119] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Vazquez Roque M, Bouras EP. Epidemiology and management of chronic constipation in elderly patients. Clin Interv Aging. 2015;10:919-930. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Oswari H, Alatas FS, Hegar B, Cheng W, Pramadyani A, Benninga MA, Rajindrajith S. Epidemiology of Paediatric constipation in Indonesia and its association with exposure to stressful life events. BMC Gastroenterol. 2018;18:146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Serra J, Pohl D, Azpiroz F, Chiarioni G, Ducrotté P, Gourcerol G, Hungin APS, Layer P, Mendive JM, Pfeifer J, Rogler G, Scott SM, Simrén M, Whorwell P; Functional Constipation Guidelines Working Group. European society of neurogastroenterology and motility guidelines on functional constipation in adults. Neurogastroenterol Motil. 2020;32:e13762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 153] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 8. | Serra J, Mascort-Roca J, Marzo-Castillejo M, Delgado Aros S, Ferrándiz Santos J, Rey Diaz Rubio E, Mearin Manrique F. Clinical practice guidelines for the management of constipation in adults. Part 1: Definition, aetiology and clinical manifestations. Gastroenterol Hepatol. 2017;40:132-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Remes-Troche JM, Coss-Adame E, Lopéz-Colombo A, Amieva-Balmori M, Carmona Sánchez R, Charúa Guindic L, Flores Rendón R, Gómez Escudero O, González Martínez M, Icaza Chávez ME, Morales Arámbula M, Schmulson M, Tamayo de la Cuesta JL, Valdovinos MÁ, Vázquez Elizondo G. The Mexican consensus on chronic constipation. Rev Gastroenterol Mex (Engl Ed). 2018;83:168-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Andrews CN, Storr M. The pathophysiology of chronic constipation. Can J Gastroenterol. 2011;25 Suppl B:16B-21B. [PubMed] |
| 11. | Faussone-Pellegrini MS, Thuneberg L. Guide to the identification of interstitial cells of Cajal. Microsc Res Tech. 1999;47:248-266. [PubMed] [DOI] [Full Text] |
| 12. | Wang XY, Sanders KM, Ward SM. Intimate relationship between interstitial cells of cajal and enteric nerves in the guinea-pig small intestine. Cell Tissue Res. 1999;295:247-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 128] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 13. | Klein S, Seidler B, Kettenberger A, Sibaev A, Rohn M, Feil R, Allescher HD, Vanderwinden JM, Hofmann F, Schemann M, Rad R, Storr MA, Schmid RM, Schneider G, Saur D. Interstitial cells of Cajal integrate excitatory and inhibitory neurotransmission with intestinal slow-wave activity. Nat Commun. 2013;4:1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 185] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 14. | Strege PR, Gibbons SJ, Mazzone A, Bernard CE, Beyder A, Farrugia G. EAVK segment "c" sequence confers Ca(2+)-dependent changes to the kinetics of full-length human Ano1. Am J Physiol Gastrointest Liver Physiol. 2017;312:G572-G579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Park CG, Kim YD, Kim MY, Kim JS, Choi S, Yeum CH, Parajuli SP, Park JS, Jeong HS, So I, Kim KW, Jun JY. Inhibition of pacemaker currents by nitric oxide via activation of ATP-sensitive K+ channels in cultured interstitial cells of Cajal from the mouse small intestine. Naunyn Schmiedebergs Arch Pharmacol. 2007;376:175-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Zhou J, O'Connor MD, Ho V. The Potential for Gut Organoid Derived Interstitial Cells of Cajal in Replacement Therapy. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Huizinga JD, Martz S, Gil V, Wang XY, Jimenez M, Parsons S. Two independent networks of interstitial cells of cajal work cooperatively with the enteric nervous system to create colonic motor patterns. Front Neurosci. 2011;5:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | Wang YB, Ling J, Zhang WZ, Li G, Qiu W, Zheng JH, Zhao XH. Effect of bisacodyl on rats with slow transit constipation. Braz J Med Biol Res. 2018;51:e7372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Gariepy CE. Developmental disorders of the enteric nervous system: genetic and molecular bases. J Pediatr Gastroenterol Nutr. 2004;39:5-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Bassotti G, Villanacci V. Slow transit constipation: a functional disorder becomes an enteric neuropathy. World J Gastroenterol. 2006;12:4609-4613. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 73] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 21. | Bassotti G, Villanacci V. Can "functional" constipation be considered as a form of enteric neuro-gliopathy? Glia. 2011;59:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Bassotti G, Villanacci V, Maurer CA, Fisogni S, Di Fabio F, Cadei M, Morelli A, Panagiotis T, Cathomas G, Salerni B. The role of glial cells and apoptosis of enteric neurones in the neuropathology of intractable slow transit constipation. Gut. 2006;55:41-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 156] [Article Influence: 7.8] [Reference Citation Analysis (1)] |
| 23. | Wedel T, Roblick UJ, Ott V, Eggers R, Schiedeck TH, Krammer HJ, Bruch HP. Oligoneuronal hypoganglionosis in patients with idiopathic slow-transit constipation. Dis Colon Rectum. 2002;45:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 73] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 24. | Han Y, Wang JM. Effects of Jianpiyiqitongbian Formula on the quality of life evaluation and related enteric neurotransmitters in slow-transmitting constipation with lung and spleen qi deficiency type. Zhongyiyao Linchuang Zazhi. 2018;30:518-520. [DOI] [Full Text] |
| 25. | Israelyan N, Del Colle A, Li Z, Park Y, Xing A, Jacobsen JPR, Luna RA, Jensen DD, Madra M, Saurman V, Rahim R, Latorre R, Law K, Carson W, Bunnett NW, Caron MG, Margolis KG. Effects of Serotonin and Slow-Release 5-Hydroxytryptophan on Gastrointestinal Motility in a Mouse Model of Depression. Gastroenterology. 2019;157:507-521.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 142] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 26. | King SK, Sutcliffe JR, Ong SY, Lee M, Koh TL, Wong SQ, Farmer PJ, Peck CJ, Stanton MP, Keck J, Cook DJ, Chow CW, Hutson JM, Southwell BR. Substance P and vasoactive intestinal peptide are reduced in right transverse colon in pediatric slow-transit constipation. Neurogastroenterol Motil. 2010;22:883-892, e234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Singh RD, Gibbons SJ, Saravanaperumal SA, Du P, Hennig GW, Eisenman ST, Mazzone A, Hayashi Y, Cao C, Stoltz GJ, Ordog T, Rock JR, Harfe BD, Szurszewski JH, Farrugia G. Ano1, a Ca2+-activated Cl- channel, coordinates contractility in mouse intestine by Ca2+ transient coordination between interstitial cells of Cajal. J Physiol. 2014;592:4051-4068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 100] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 28. | Attaluri A, Jackson M, Valestin J, Rao SS. Methanogenic flora is associated with altered colonic transit but not stool characteristics in constipation without IBS. Am J Gastroenterol. 2010;105:1407-1411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 29. | Ohkusa T, Koido S, Nishikawa Y, Sato N. Gut Microbiota and Chronic Constipation: A Review and Update. Front Med (Lausanne). 2019;6:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 106] [Cited by in RCA: 240] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 30. | Carco C, Young W, Gearry RB, Talley NJ, McNabb WC, Roy NC. Increasing Evidence That Irritable Bowel Syndrome and Functional Gastrointestinal Disorders Have a Microbial Pathogenesis. Front Cell Infect Microbiol. 2020;10:468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (1)] |
| 31. | Dykes S, Smilgin-Humphreys S, Bass C. Chronic idiopathic constipation: a psychological enquiry. Eur J Gastroenterol Hepatol. 2001;13:39-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 32. | Saps M, Velasco-Benitez CA, Fernandez Valdes L, Mejia J, Villamarin E, Moreno J, Ramirez C, González MJ, Vallenilla I, Falcon AC, Axelrod C. The impact of incorporating toilet-training status in the pediatric Rome IV criteria for functional constipation in infant and toddlers. Neurogastroenterol Motil. 2020;32:e13912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 33. | Sun J, Guo H, Chen L, Wu XL, Li H, Pei LX, Peng YJ, Lu B. Effects of electroacupuncture on the structure of colonic smooth muscle and Cajal mesenchymal stromal cells in rats with slow-transmitting constipation. Zhenci Yanjiu. 2011;36:171-175. [DOI] [Full Text] |
| 34. | Zhong W, Sun B, Ruan H, Yang G, Qian B, Cao H, He L, Fan Y, Roberts AG, Liu X, Hu X, Liang Y, Ye Q, Yin T, Wang B, Yang C, Sun T, Zhou H. Deglycosylated Azithromycin Targets Transgelin to Enhance Intestinal Smooth Muscle Function. iScience. 2020;23:101464. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 35. | Yamaji M, Mahmoud M, Evans IM, Zachary IC. Neuropilin 1 is essential for gastrointestinal smooth muscle contractility and motility in aged mice. PLoS One. 2015;10:e0115563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 36. | Kim JE, Go J, Lee HS, Hong JT, Hwang DY. Spicatoside A in red Liriope platyphylla displays a laxative effect in a constipation rat model via regulating mAChRs and ER stress signaling. Int J Mol Med. 2019;43:185-198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 37. | Higgins PD, Johanson JF. Epidemiology of constipation in North America: a systematic review. Am J Gastroenterol. 2004;99:750-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 692] [Cited by in RCA: 687] [Article Influence: 31.2] [Reference Citation Analysis (1)] |
| 38. | Chan AO, Hui WM, Lam KF, Leung G, Yuen MF, Lam SK, Wong BC. Familial aggregation in constipated subjects in a tertiary referral center. Am J Gastroenterol. 2007;102:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Yang J, Wang HP, Zhou L, Xu CF. Effect of dietary fiber on constipation: a meta analysis. World J Gastroenterol. 2012;18:7378-7383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 165] [Cited by in RCA: 177] [Article Influence: 12.6] [Reference Citation Analysis (6)] |
| 40. | Yurtdaş G, Acar-Tek N, Akbulut G, Cemali Ö, Arslan N, Beyaz Coşkun A, Zengin FH. Risk Factors for Constipation in Adults: A Cross-Sectional Study. J Am Coll Nutr. 2020;39:713-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 41. | Jung SJ, Oh MR, Park SH, Chae SW. Effects of rice-based and wheat-based diets on bowel movements in young Korean women with functional constipation. Eur J Clin Nutr. 2020;74:1565-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 42. | Simrén M. Physical activity and the gastrointestinal tract. Eur J Gastroenterol Hepatol. 2002;14:1053-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Gao R, Tao Y, Zhou C, Li J, Wang X, Chen L, Li F, Guo L. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scand J Gastroenterol. 2019;54:169-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (1)] |
| 44. | Ulusoy E, Arslan N, Küme T, Ülgenalp A, Çirali C, Bozkaya Ö, Ercal D. Serum motilin levels and motilin gene polymorphisms in children with functional constipation. Minerva Pediatr (Torino). 2021;73:420-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 45. | Cong P, Pricolo V, Biancani P, Behar J. Abnormalities of prostaglandins and cyclooxygenase enzymes in female patients with slow-transit constipation. Gastroenterology. 2007;133:445-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 46. | Wang Y, Jiang Y, Jiang L, Xiong W, Wang Y, Gao X, Chen Q, Lin L, Yu T, Tang Y. Estrogen increases the expression of BKCa and impairs the contraction of colon smooth muscle via upregulation of sphingosine kinase 1. J Cell Physiol. 2023;238:2390-2406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 47. | Oh JE, Kim YW, Park SY, Kim JY. Estrogen rather than progesterone cause constipation in both female and male mice. Korean J Physiol Pharmacol. 2013;17:423-426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 48. | Shams-White MM, Pannucci TE, Lerman JL, Herrick KA, Zimmer M, Meyers Mathieu K, Stoody EE, Reedy J. Healthy Eating Index-2020: Review and Update Process to Reflect the Dietary Guidelines for Americans,2020-2025. J Acad Nutr Diet. 2023;123:1280-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 310] [Article Influence: 103.3] [Reference Citation Analysis (0)] |
| 49. | Lucak S, Lunsford TN, Harris LA. Evaluation and Treatment of Constipation in the Geriatric Population. Clin Geriatr Med. 2021;37:85-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (12)] |
| 50. | Locke GR 3rd, Pemberton JH, Phillips SF. American Gastroenterological Association Medical Position Statement: guidelines on constipation. Gastroenterology. 2000;119:1761-1766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 146] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: Https://creativecommons.org/Licenses/by-nc/4.0/